Similar presentations:
General characteristic of infectious diseases with the faeco-oral mechanism of transmission
1.
General characteristic of infectiousdiseases with the faeco-oral mechanism of
transmission .
Typhoid fever ( Typhus abdominalis )
and Paratyphoid A,B,C
2.
For diseases with the faeco-oral mechanism oftransmission typically:
- specific localization of the causative agent in intestine
determines its removing from the infected organism with
faeces or vomiting mass.
- further it can penetrate into a susceptible organism, using
ways of transmission (water, food, contact-household),
including various factors of transmission ( foodstuff,
water, hands, flies, household goods, toys, ground) which
directly participate in carry of the causative agent from its
source to susceptible persons
- in intestine the causative agent can be: in a lumen of
intestine, in epithelium intestine, in a thickness mucous
membrane of intestine, in lymphatic formations of
intestine).
3.
Causative agent can constantly be in intestine (cholera,dysentery, some helminthic invasion) or temporarily, penetrate
from intestine in blood and other bodies (ascariasis,
amebiasis, strongyloidiasis, trichinosis, echinococcosis).
Therefore allocate primary and secondary localization of
the causative agent in an organism of the patient:
Typhoid fever ( Typhus abdominalis ) and Paratyphoid A,B,
the causative agent multiplies in intestine ( primary
localization ), but it, as a rule, will penetrate into blood and
internal bodies (secondary localization),
The virus of a hepatites A - being multiplies in liver cells,
will penetrate into intestine through bile ducts,
Enteroviruses- except for epithelium intestine, can will be
multiplied in epithelium URT (secondary localization), that
enable the causative agents to be allocated from an
organism not only through intestine, but also through
other bodies with urine, sputum, etc.
4.
To intestinal infections, behind exception helminthicinvasion the tendency to entire damage of the population is
not peculiar. Even at high morbidity rate in district many
usually do not fall ill.
Therefore continuous natural immunization at them is
actually impossible. The level of morbidity as against acute
infections of respiratory ways ( flu, measles) is regulated
by contamination of the population. The natural immune
section with rare exception (dysentery, VHA) influences on
of morbidity rate a little.
Rise of morbidity rate coincides with the warm period of
year. In moderate climatic zones of the earth it is registered
during summery or autumnal time is more often
5.
Typhoid fever (Typhus abdominalis)and Paratyphoid A,B,C - typical disease with the
faeco-oral mechanism of transmission.
Identification - typhoid fever is an acute anthroponosis systemic disease resulting from infection with
S.typhi and accompanying by:
bacteriemia, fever, intoxication, abdominal discomfort,
malaise,
spleenomegaly, damage of lymphatic derivations of a small
intestine and mesenterial nodes, scanty roseolous rash
6.
Historic reference:From times Hippokrates (466 - 377 up to AD) to the18th
century all diseases, which were accompanied by a fever and
oppression or loss of consciousness were named by typhoids
( typhos – it is smoke, fog )
• 1874 - Брович discovered of the causative agent the first time!
1876 - Н.И.Соколов discovered its in Peyer’s patches
• 1880 - K. Eberth - discovered its in a spleen and mesenterial nodes
• 1884 - G.Gaffky received of the agent in pure culture
• 1887 - А.И. Вильчур received its from a blood
• 1896 - M.Gruber revealed a phenomenon of an agglutination, and Widal G.F.I used this phenomenon
for diagnosis typhoid the first time!
7.
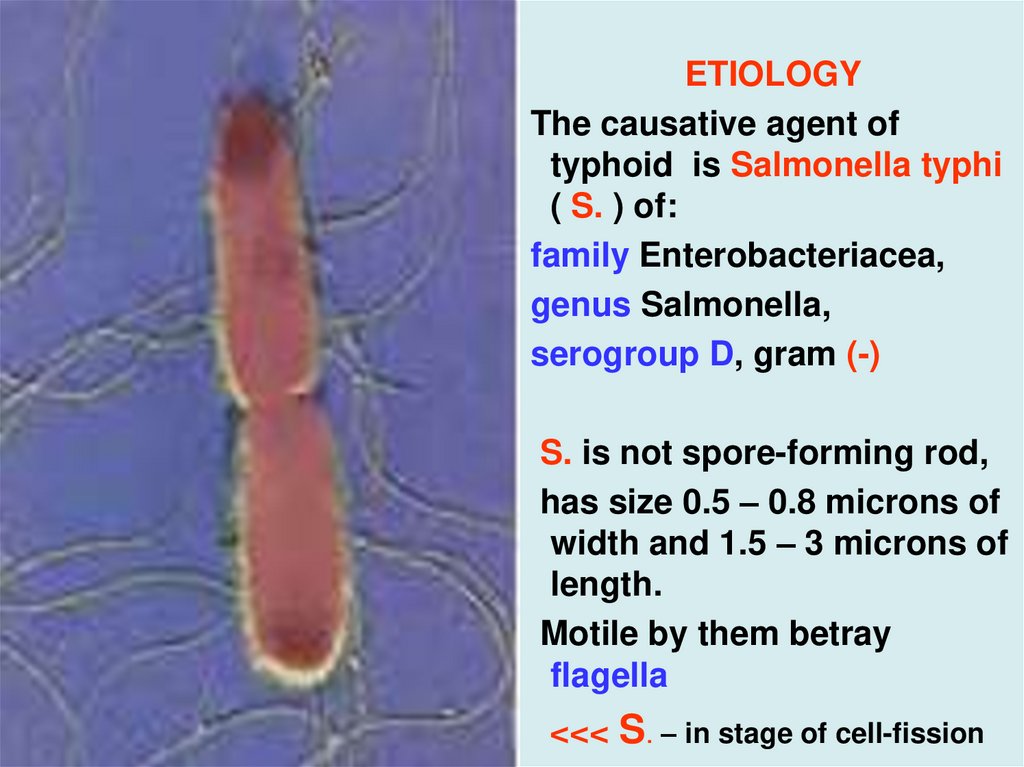
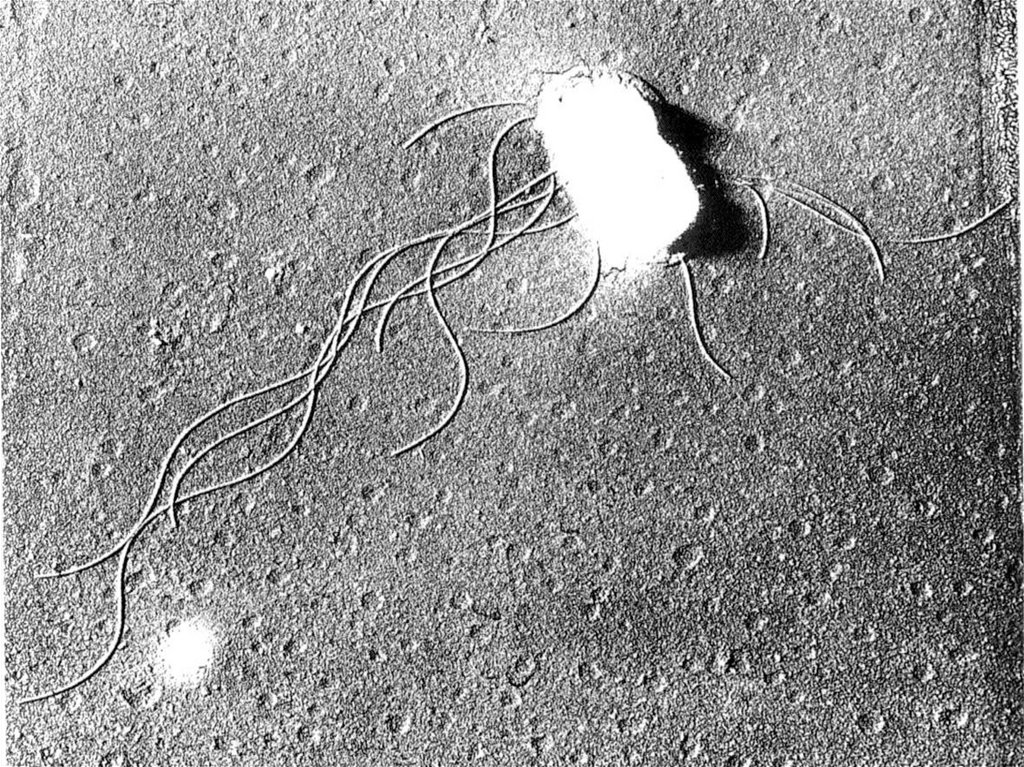
ETIOLOGYThe causative agent of
typhoid is Salmonella typhi
( S. ) of:
family Enterobacteriacea,
genus Salmonella,
serogroup D, gram (-)
S. is not spore-forming rod,
has size 0.5 – 0.8 microns of
width and 1.5 – 3 microns of
length.
Motile by them betray
flagella
<<< S. – in stage of cell-fission
8.
9.
S. can longly be survived in an organism as filtered or L- ofthe forms.
S. are survived by months in environment.
S. not only are longly survived, but also are multiplied in
foodstuffs (milk, cheese, jelly, forcemeat etc.) and not
changing their gustatory qualities.
S. well endure low temperature, but at warming up to 60 dg.
C destroy them through 30 minutes and at boiling instantly
S. are inactivated desinfectants in usual concentrations in
during 3 - 5 minutes.
10.
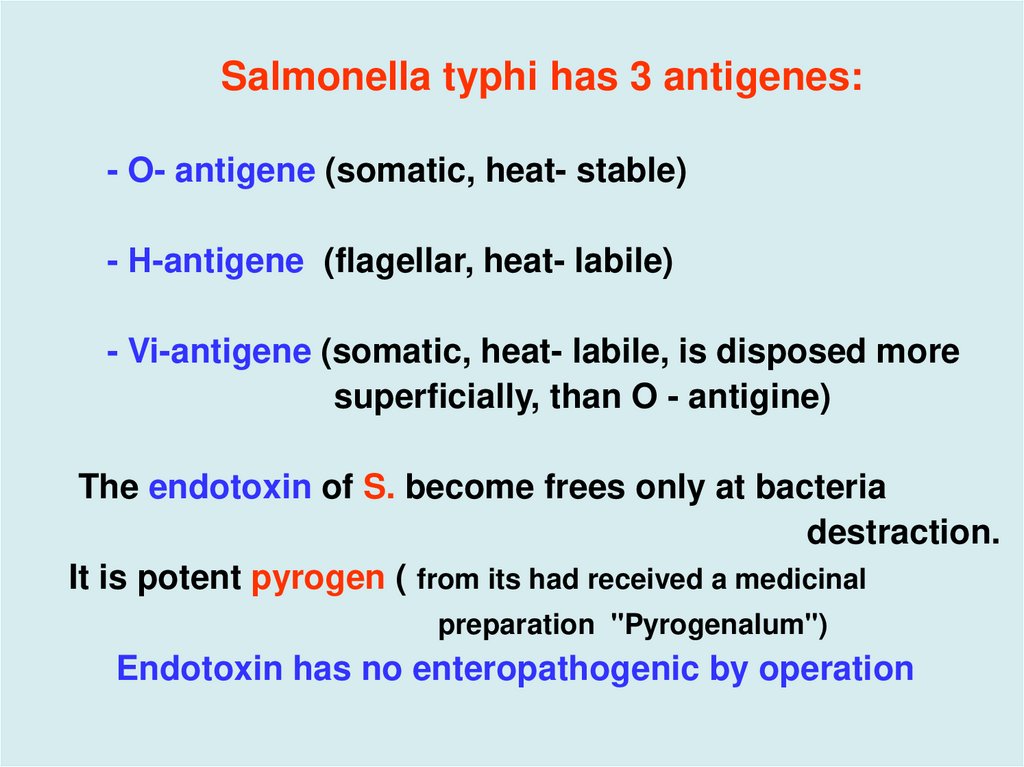
Salmonella typhi has 3 antigenes:- O- antigene (somatic, heat- stable)
- Н-antigene (flagellar, heat- labile)
- Vi-antigene (somatic, heat- labile, is disposed more
superficially, than O - antigine)
The endotoxin of S. become frees only at bacteria
destraction.
It is potent pyrogen ( from its had received a medicinal
preparation "Pyrogenalum")
Endotoxin has no enteropathogenic by operation
11.
Epidemiology: typhoid fever is anthroponosisThe source – sick the persons (20 – 30%) or the carriers
( 70%- 80%) which secrete of S . typhi with a feces, urine,
sputum
Transmission is by the faecal-oral route
The factors of transmission:
- contaminated water (more often)
- contaminated foodstuffs (molluscs – oysters, mussels)
- contact to the sick the person or subjects enclosing
him
Age of majority of the patients: - from 15 up to 45 years
( more often are sick men )
Seasonal prevalence - in summer-autumn.
12.
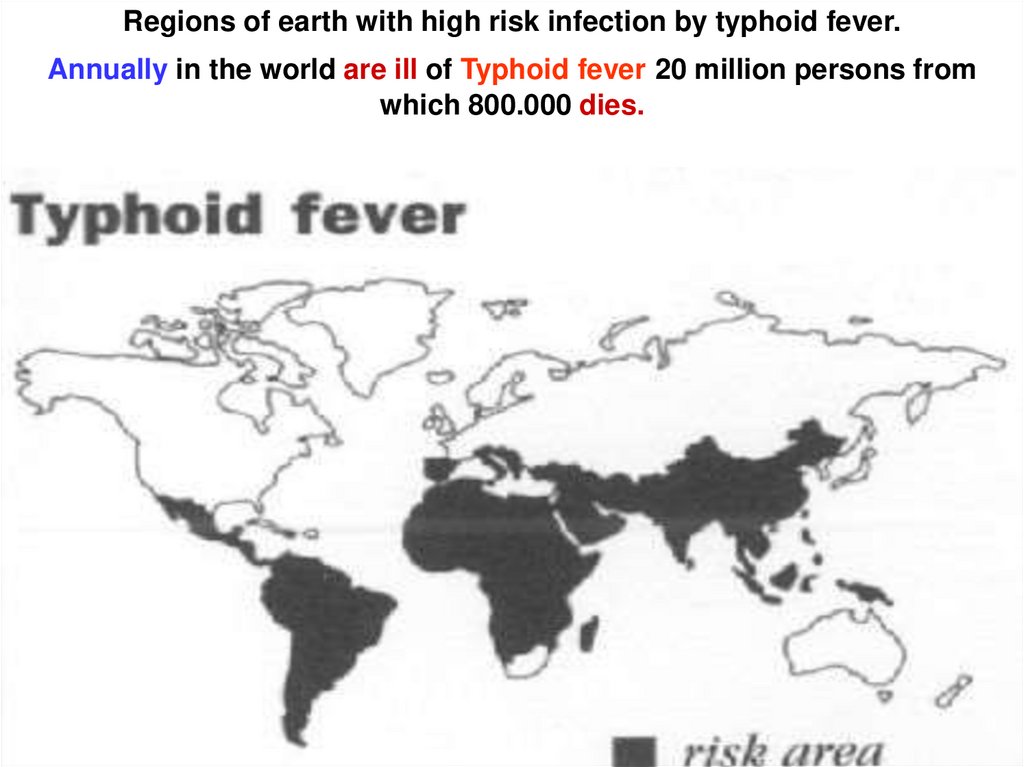
Regions of earth with high risk infection by typhoid fever.Annually in the world are ill of Typhoid fever 20 million persons from
which 800.000 dies.
13.
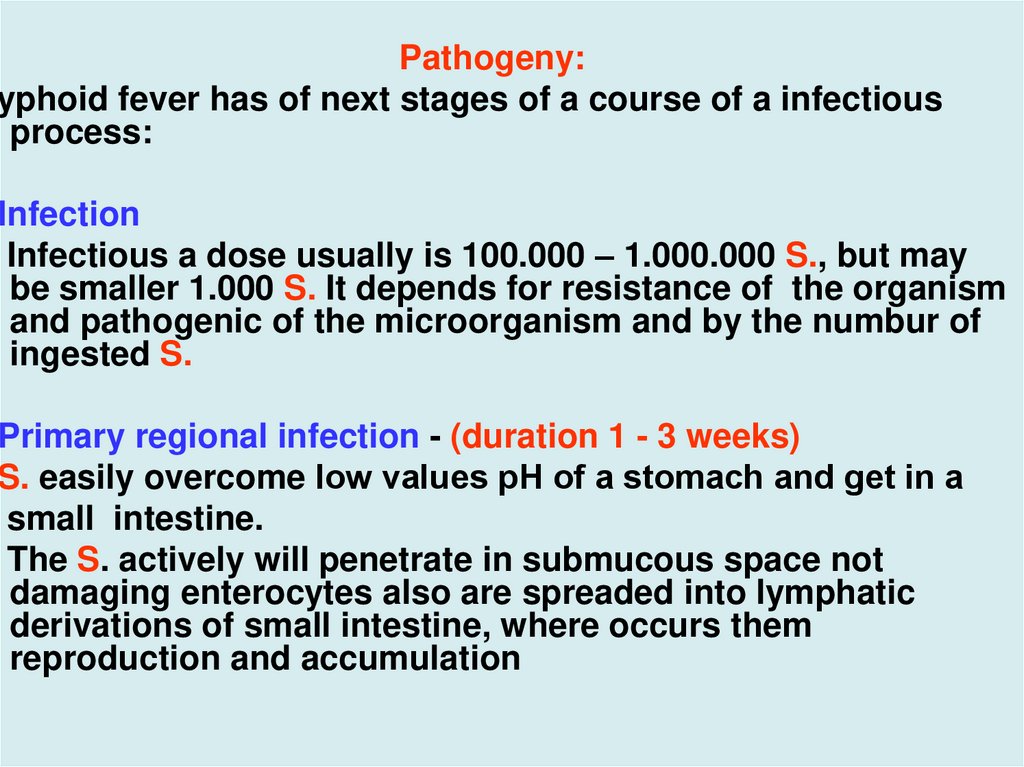
Pathogeny:Typhoid fever has of next stages of a course of a infectious
process:
Infection
Infectious a dose usually is 100.000 – 1.000.000 S., but may
be smaller 1.000 S. It depends for resistance of the organism
and pathogenic of the microorganism and by the numbur of
ingested S.
Primary regional infection - (duration 1 - 3 weeks)
S. easily overcome low values рН of a stomach and get in a
small intestine.
The S. actively will penetrate in submucous space not
damaging enterocytes also are spreaded into lymphatic
derivations of small intestine, where occurs them
reproduction and accumulation
14.
3. Part S. attack leucocytes, which start to work outprostaglandin Е, causing a secretory diarrhoea.
The phagocytes may be transport S. in other sites SMP
( system macrophagal of phagocytes ) because of the
uncompleted phagocytosis
4.Other part S. will already penetrate into a blood at this
stage of illness, causing a short-term bacteriemia, which,
however, results in a damage of many bodies of SМP
5.Bacteriemia and toxinemia (1st week of illness)
- is characterized by development of lymphadenites and
lymphangites, by cerebriform bloating of Peyer’s patches
and long bacteriemia with repeated drifts S. in bodies
SMP.
15.
16.
6.The parenchymatous dissimination of S. (2 - 3 weeks ofillness) It is characterized by a damage, practically, of all
internal bodies with creation in them of typhoid
granulomas contened macrophages ( 90 % ) and of
neutrophils ( 10 % ), toxic damage a CNS - central nervous
system (typhous status), bone marrow (leukopenia), by
appearance on a skin scanty roseolous of a rash.
7. Excretory - allergic stage of illness: ( 2-3 weeks of
illness)
It is characterized:
- by massive excretion of the S. through kidneys, cholic
track, crypts of an intestine, with a sputum
- by violation of microcirculation in capillaries with their
partial thrombosing, development of a coagulopathy
- maximal strain of immune processes
- by local allergic responses
17.
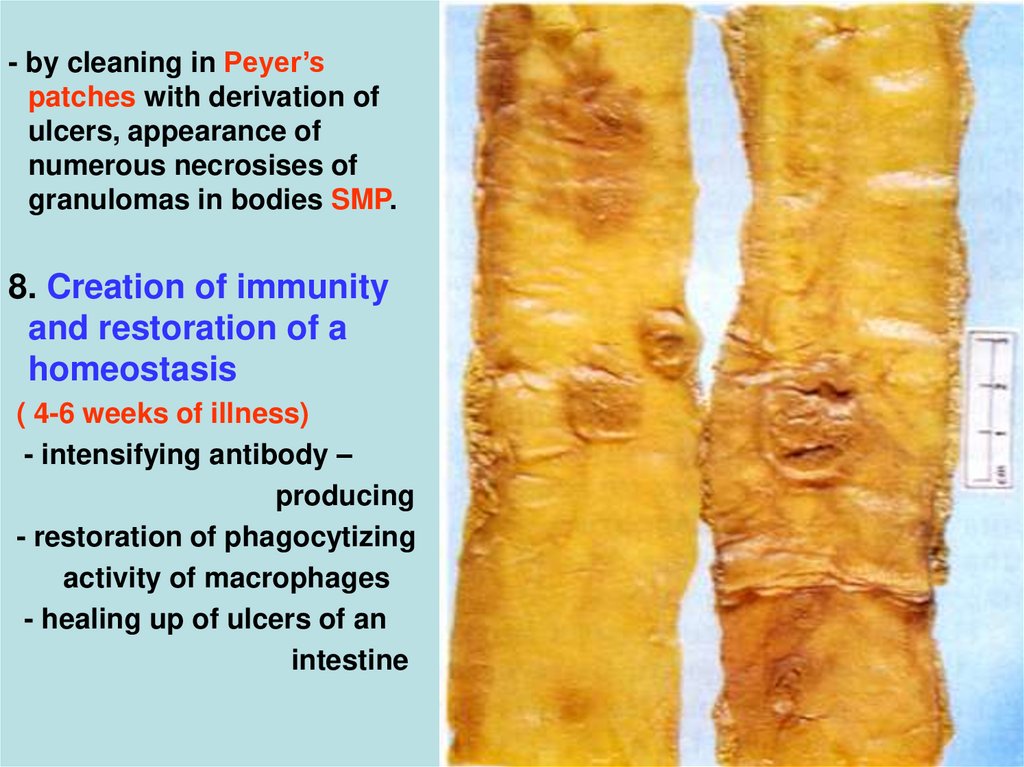
- by cleaning in Peyer’spatches with derivation of
ulcers, appearance of
numerous necrosises of
granulomas in bodies SMP.
8. Creation of immunity
and restoration of a
homeostasis
( 4-6 weeks of illness)
- intensifying antibody –
producing
- restoration of phagocytizing
activity of macrophages
- healing up of ulcers of an
intestine
18.
Period of convalescence (5 - 6 weeks of illness)- normalization of microcirculation and restoration of the
functions the struck bodies
- period of a self-healing of ulcers
- creation of immunity
Features of a bacteriemia at a typhoid:
- the bacteriemia is always inappreciable (less than 50 S. in
1 ml. blood )
- the endotoxin in a blood, practically, is not found out
- the endotoxin mainly renders local action, is especial in
places of a clumps S.
19.
Pathomorphology- lymphatic nodes, liver, spleen, bone marrow are pletoric
with the centers of a necrosis
- hyperplasia of all bodies SMP with a proliferation of
monocytes
- in a gall bladder the centers of an inflammation have focal
and nonconstant character
- in lungs are discovered the signs of a bronchitis almost
for all patients
- from any tissue of the perished is possible to find out S.!
20.
Cliniccal manifestationsThe incubation interval of typhoid fever is useally 9 - 14
days but it may be from 5 to 40 days. The duration of
incubation interval depends in the number, virulence of
ingested S, and state of a macrorganism.
There are such periods during course of infectious process:
Initial:
- the fever accrues gradually for 2-3 days and reaches 3940dg.C ( Now 66 % of patients are ill acutely)
- headache increasing with each day
- inversion of dream (sleepiness–in the afternoon, insomnia–at
night)
- weakness, lowering of appetite, chilling, adynamia
- dynamic meteorism, constipation, sometimes short-term
secretory diarrhoea
21.
Objective:- Inhibited and adynamic, the paleness of a skin is (more
often) or hyperemia of the face
- tachycardia with change then on a relative bradycardia
- lower of BP
- moderate respiration and dry rales
- coated and enlarged of tongue with impressions of teeth!!!
- abdominal distention and murmur in the right hypogastric
area, local obtusion there of a percussion’s sound (s- m
Падалка)
- enlargement of a liver and spleen - with 3- 4 days of illness
- WBC - moderate leukocytosis, but with 4 - 5 days of illness
- leukopenia, eosinopenia , relative lymphocytosis and
thrombocytopenia
- the changes of urine correspond – to syndrome " toxic"
kidney.
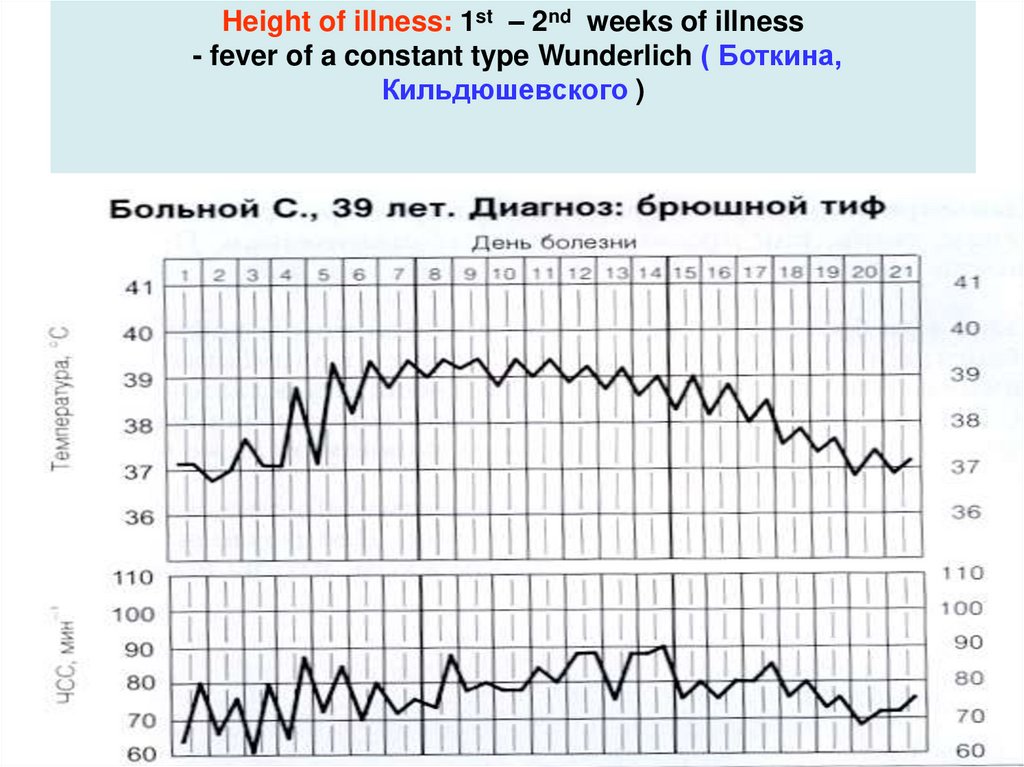
22. Height of illness: 1st – 2nd weeks of illness - fever of a constant type Wunderlich ( Боткина, Кильдюшевского )
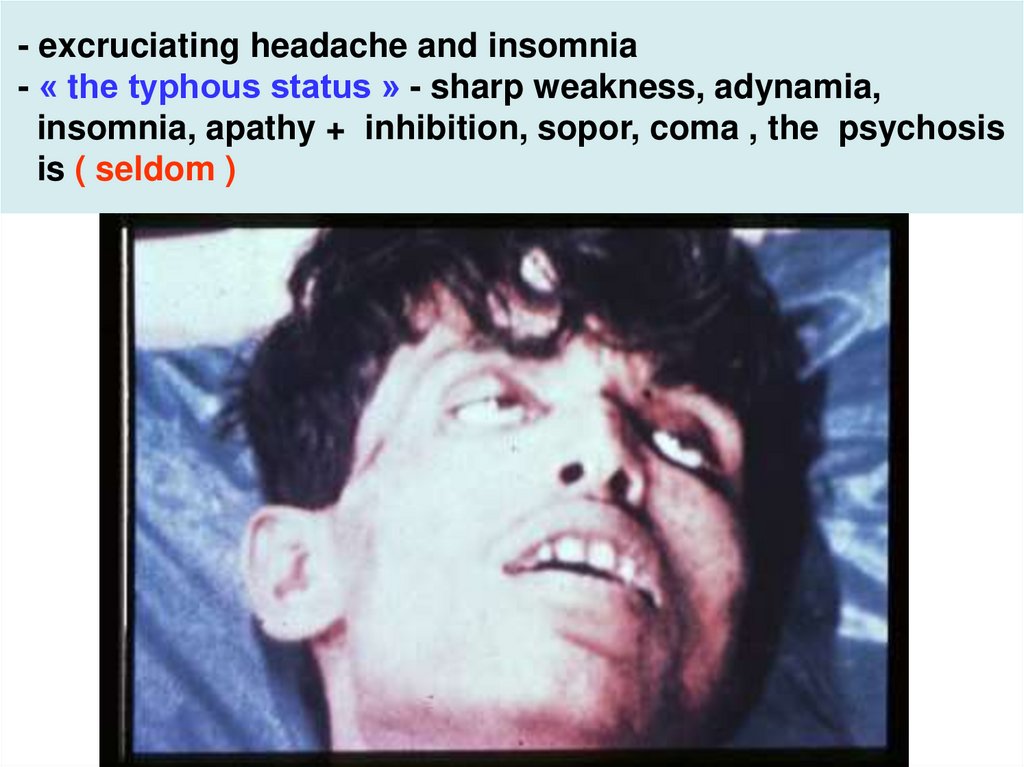
23. - excruciating headache and insomnia - « the typhous status » - sharp weakness, adynamia, insomnia, apathy + inhibition, sopor,
coma , the psychosisis ( seldom )
24.
25.
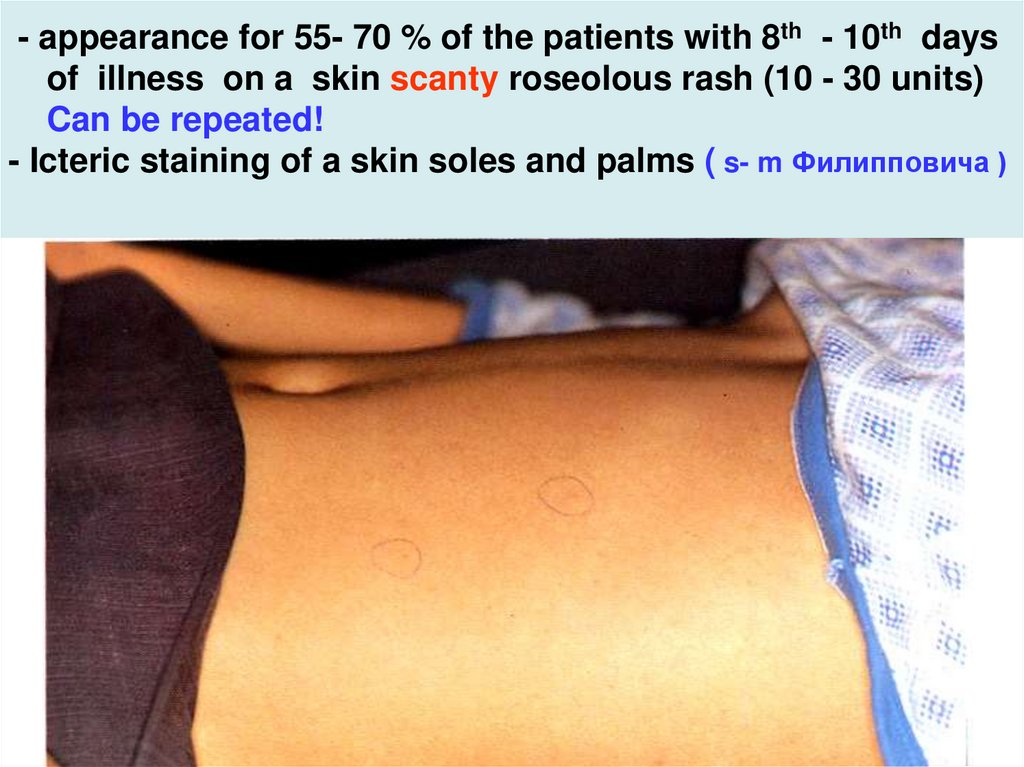
26. - appearance for 55- 70 % of the patients with 8th - 10th days of illness on a skin scanty roseolous rash (10 - 30 units) Can
be repeated!- Icteric staining of a skin soles and palms ( s- m Филипповича )
27. - skin acyanotic, dry, hot - the lips dry with scabs but herpes does not happen - weakness of cardiac sounds, a bradycardia,
dicrotism ofpulse, lowering BP, systolic murmur at the heart apex
- lungs - moderate respiration, dry rales
- tongue coated patch from up white to brown colour and
enlarged with impressions of teeth !!
28.
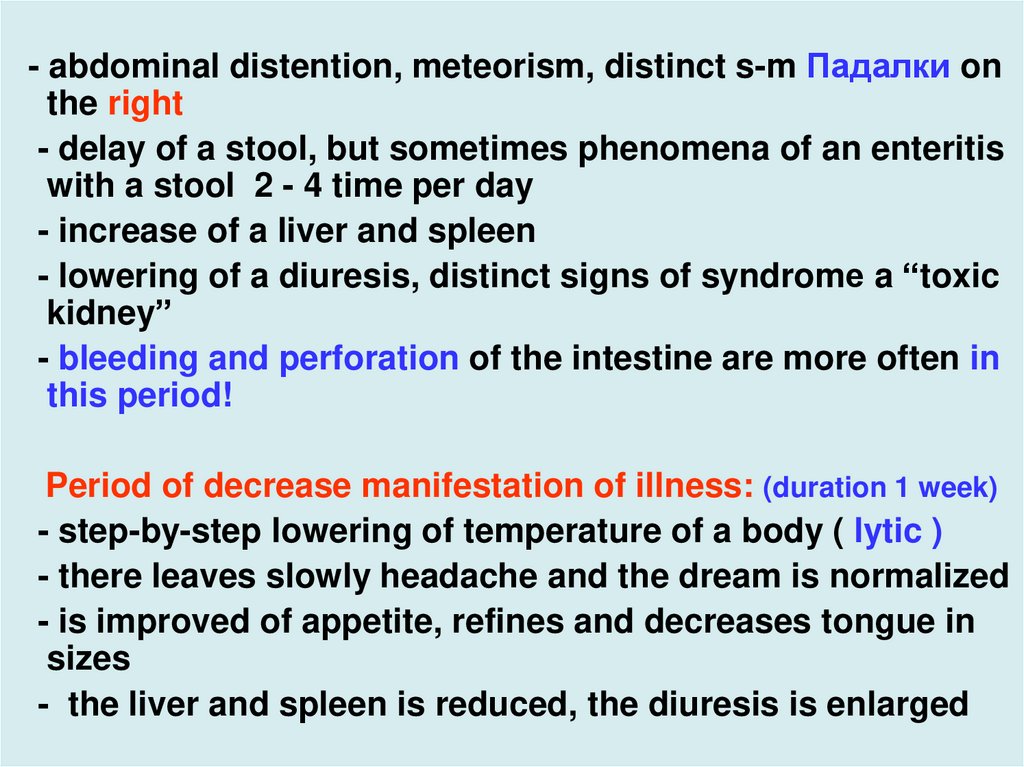
- abdominal distention, meteorism, distinct s-m Падалки onthe right
- delay of a stool, but sometimes phenomena of an enteritis
with a stool 2 - 4 time per day
- increase of a liver and spleen
- lowering of a diuresis, distinct signs of syndromе a “toxic
kidney”
- bleeding and perforation of the intestine are more often in
this period!
Period of decrease manifestation of illness: (duration 1 week)
- step-by-step lowering of temperature of a body ( lytic )
- there leaves slowly headache and the dream is normalized
- is improved of appetite, refines and decreases tongue in
sizes
- the liver and spleen is reduced, the diuresis is enlarged
29.
Period of convalescence: 2 - 4 weeks.- step-by-step restoration organs of the lost functions and
disappearance of a astheno-vegetative set of symptoms
The atypical forms of illness:
Abortive - the clinical pattern does not reach complete
development, the fever more often keeps 7 - 10 days, and
then is critically reduced, very seldom there is an
exanthema, fast disappearance of an intoxication and other
manifestations of illness
The erased form - "«out-patient" typhoid - intoxication the
inappreciable, subfebrile fever 2 - 7 days, is very rare an
exanthema, the changes of internal bodies are
inappreciable also their function is not broken, a working
capacity frequently is saved
30.
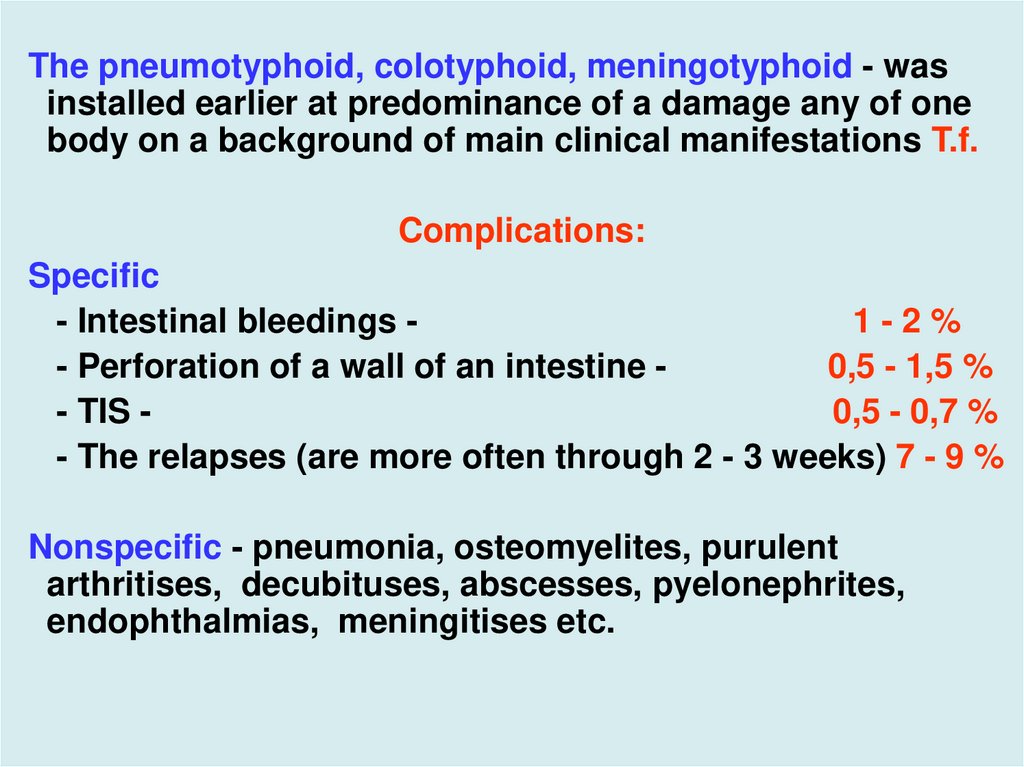
The pneumotyphoid, colotyphoid, meningotyphoid - wasinstalled earlier at predominance of a damage any of one
body on a background of main clinical manifestations T.f.
Complications:
Specific
- Intestinal bleedings 1-2%
- Perforation of a wall of an intestine 0,5 - 1,5 %
- TIS 0,5 - 0,7 %
- The relapses (are more often through 2 - 3 weeks) 7 - 9 %
Nonspecific - pneumonia, osteomyelites, purulent
arthritises, decubituses, abscesses, pyelonephrites,
endophthalmias, meningitises etc.
31.
32.
S. carriage- is taped for 3- 5 % convalescents, is more often for the
persons with prior diseases of a gall bladder
- if the carriage is prolonged more than 3 months, more
often it remains chronic
- virulent S. passing for carriers daily on GIT - not damaging
its !
Differential diagnosis:
Typhoid shoud be considered in any patient with
unexplained fever, especialy if there is a history of recent
foreign travel to endemic areas!
33.
Ricketsiosesmalaria
brucellosis
listerosis
atypical pneumonias
sepsis
miliary tuberculosis
ornithosis
lymphogranulomatosis
pseudotuberculosis
yersiniosis
tularemia (pulmonary or septic)
rhreumatic fever
hepatitis
lymphoma
mononucleosis
medicinal illness etc.
34.
Laboratory diagnosis - diagnosis confirms by:- coprocytogram- leukocytosis (90 % from them monocytes)
-WBC – leukopenia of 3000 to 4000 cells + eosinopenia , relative
lymphocytosis and thrombocytopenia
- positive immunofluorescence test with Vi- antigene
(express - method)
- inoculation 10 - 20 mls of blood (all period of a fever)
-positive a bloodculture - in 1st week 70 – 90%
but in 3rd week of disease only 30- 40%
-positive a coproculture - in 1st week - 10 -15 %
- in 3rd –4th, weeks -75%,
- in 8th week -10%
- and after 1 year onset of illness - 3%)
35.
- positive a urineculture – parallels the frequencycoproculture
- positive sputumculture - at clinic of a pneumonia or
bronchitis
- positive bileculture - during convalescence
after 8th day of illness
- HA or IHA with O and Н by antigenes (titer 1:200)
- with Vi by an antigene ( titer 1:160 ) but for carriers titer
1:5.
Investigation repeats after 10 days - increasing of titer
fourfold confirms diagnosis!!
- positive enzymlinked immunosorbent assay (ELISA)
- positive PCR
36.
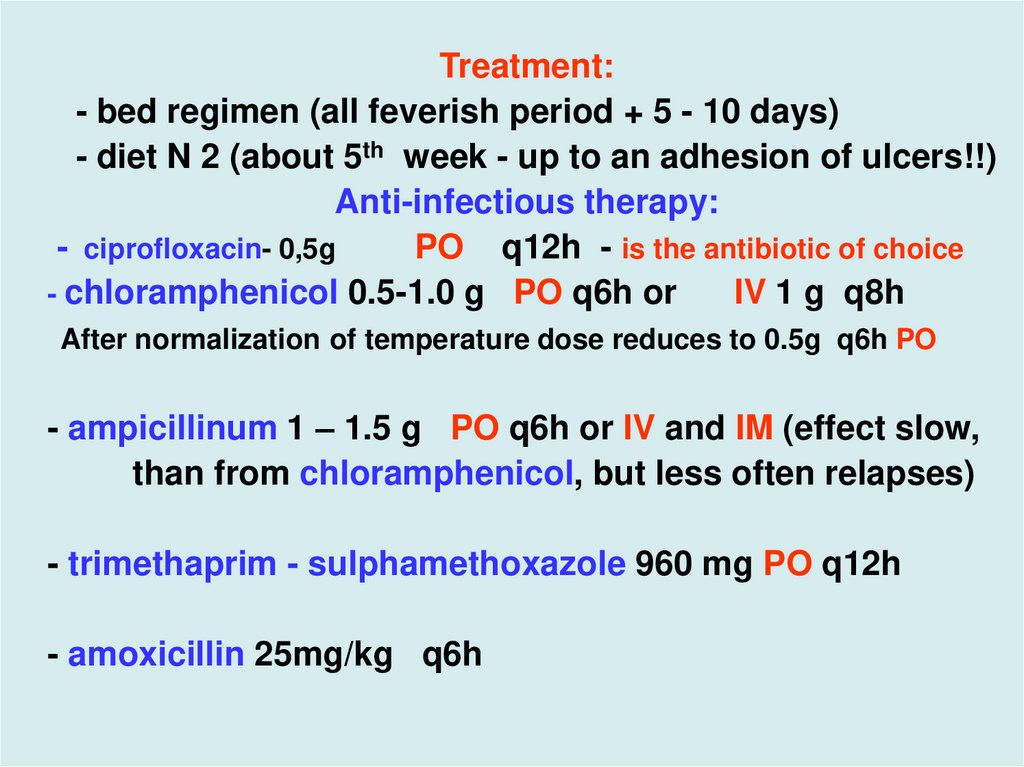
Treatment:- bed regimen (all feverish period + 5 - 10 days)
- diet N 2 (about 5th week - up to an adhesion of ulcers!!)
Anti-infectious therapy:
- ciprofloxacin- 0,5g
PO q12h - is the antibiotic of choice
- chloramphenicol 0.5-1.0 g PO q6h or
IV 1 g q8h
After normalization of temperature dose reduces to 0.5g q6h PO
- ampicillinum 1 – 1.5 g PO q6h or IV and IM (effect slow,
than from chloramphenicol, but less often relapses)
- trimethaprim - sulphamethoxazole 960 mg PO q12h
- amoxicillin 25mg/kg q6h
37.
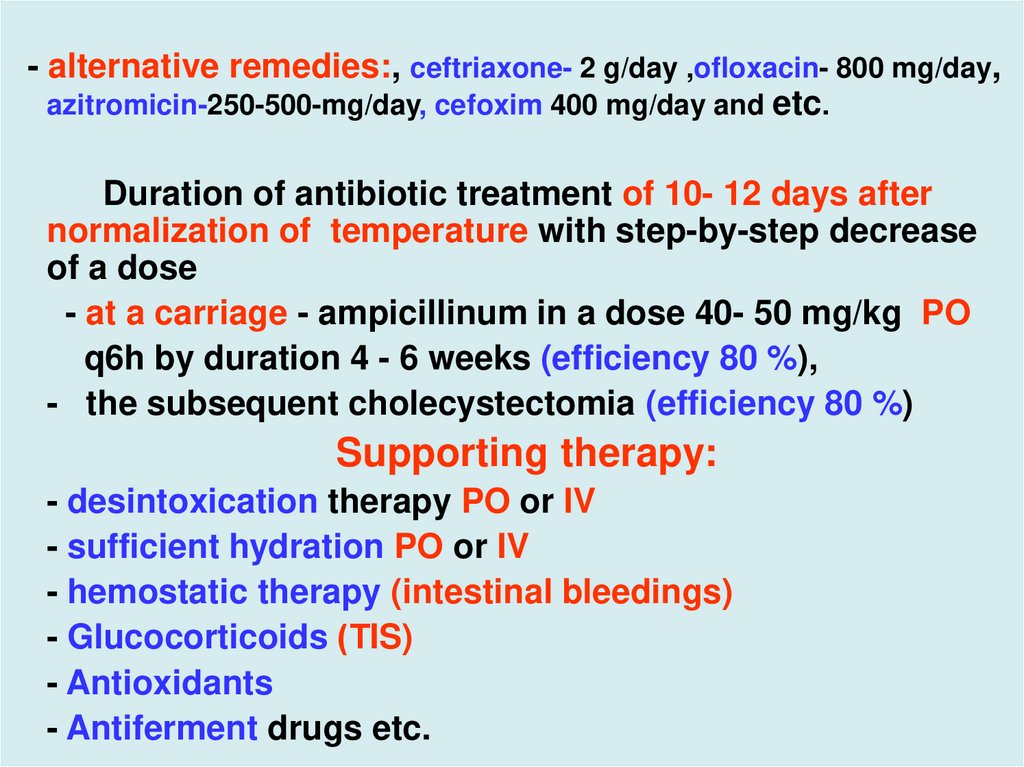
- alternative remedies:, ceftriaxone- 2 g/day ,ofloxacin- 800 mg/day,azitromicin-250-500-mg/day, cefoxim 400 mg/day and etc.
Duration of antibiotic treatment of 10- 12 days after
normalization of temperature with step-by-step decrease
of a dose
- at a carriage - ampicillinum in a dose 40- 50 mg/kg PO
q6h by duration 4 - 6 weeks (efficiency 80 %),
- the subsequent cholecystectomia (efficiency 80 %)
Supporting therapy:
- desintoxication therapy PO or IV
- sufficient hydration PO or IV
- hemostatic therapy (intestinal bleedings)
- Glucocorticoids (ТIS)
- Antioxidants
- Antiferment drugs etc.
38.
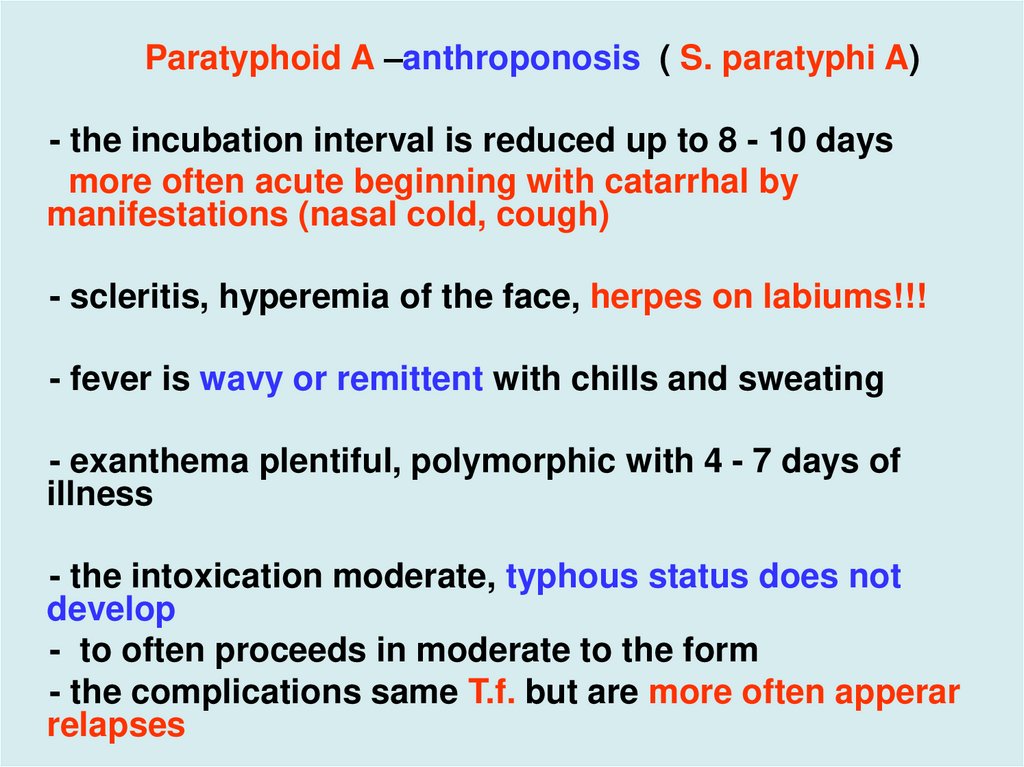
Paratyphoid A –anthroponosis ( S. paratyphi A)- the incubation interval is reduced up to 8 - 10 days
more often acute beginning with catarrhal by
manifestations (nasal cold, cough)
- scleritis, hyperemia of the face, herpes on labiums!!!
- fever is wavy or remittent with chills and sweating
- exanthema plentiful, polymorphic with 4 - 7 days of
illness
- the intoxication moderate, typhous status does not
develop
- to often proceeds in moderate to the form
- the complications same T.f. but are more often apperar
relapses
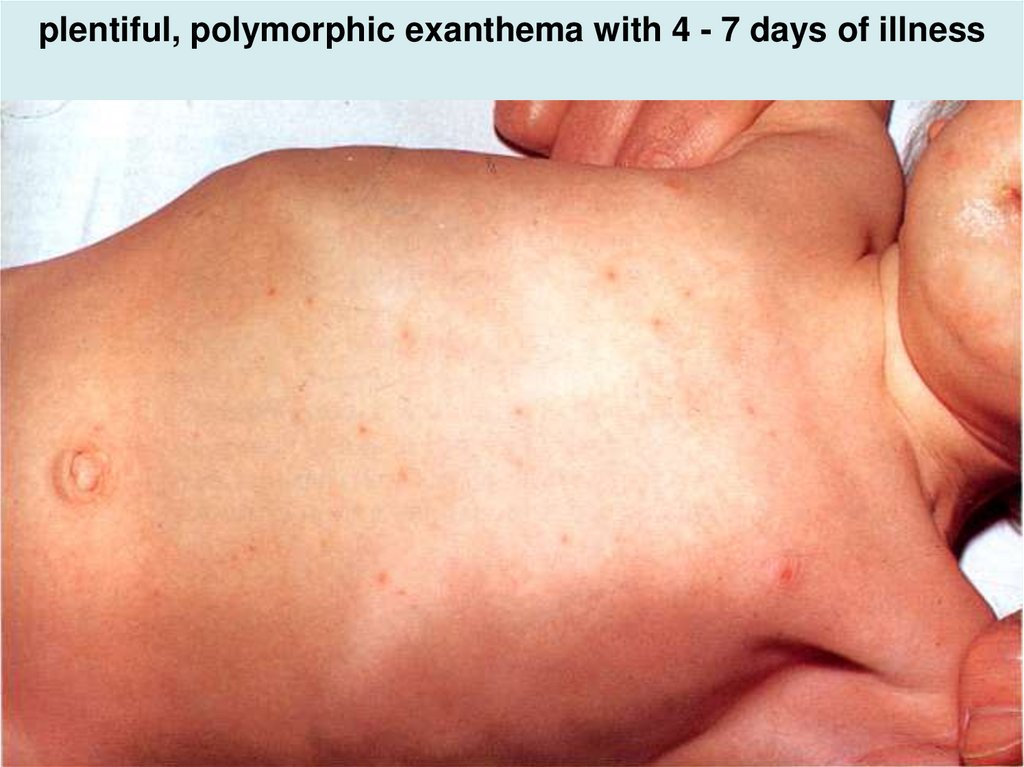
39. plentiful, polymorphic exanthema with 4 - 7 days of illness
40.
Paratyphoids B and C- zoonosis (animal and bird)S. schotmulleri, S. hirschfeldii
- incubation 5 - 10 days
- acute beginning,chills, myalgia, sweating
- moderate intoxication
- frequently phenomena of a gastroenteritis by duration 3 5 days
- the fast uprise of temperature, but it wavy and is shorter
than at T.f.
- exanthema polymorphic, plentiful with 4 - 7 days
- often give complications of septic character
(meningocephalitis, septicopyemia etc.)
- in WBC is more often a neutrophilic leukocytosis
41.
The rules of discharing of the infectious patient from ahospital
- for 21 days of normal temperature
- 3 negative coprocultures and 1 bileculture, which start to
take away from the patient after 2 days after cancellation
of antibiotics
Prophylaxis: immunity after T.f. is often intensive but the
reinfections appear in 20 - 25 %
The vaccines do not create 100 % of protection, therefore
them will using:
- at close family contact to the carrier S.
- during flashouts T.f.
- before visiting endemic areas on T.f.
42.
More important for prophylaxis T.f.:- keeping of rules of personal hygiene
- control by preparation and storage of nutrition
- the registration, sanitation and discharge from operation
of carriers of the decree groups population
- careful clearing of the drynking water
- desinfection of the sewers
- constant medical control for decree groups population




















 medicine
medicine








