Similar presentations:
Vulval and vaginal pathological conditions
1. Vulval and vaginal pathological conditions
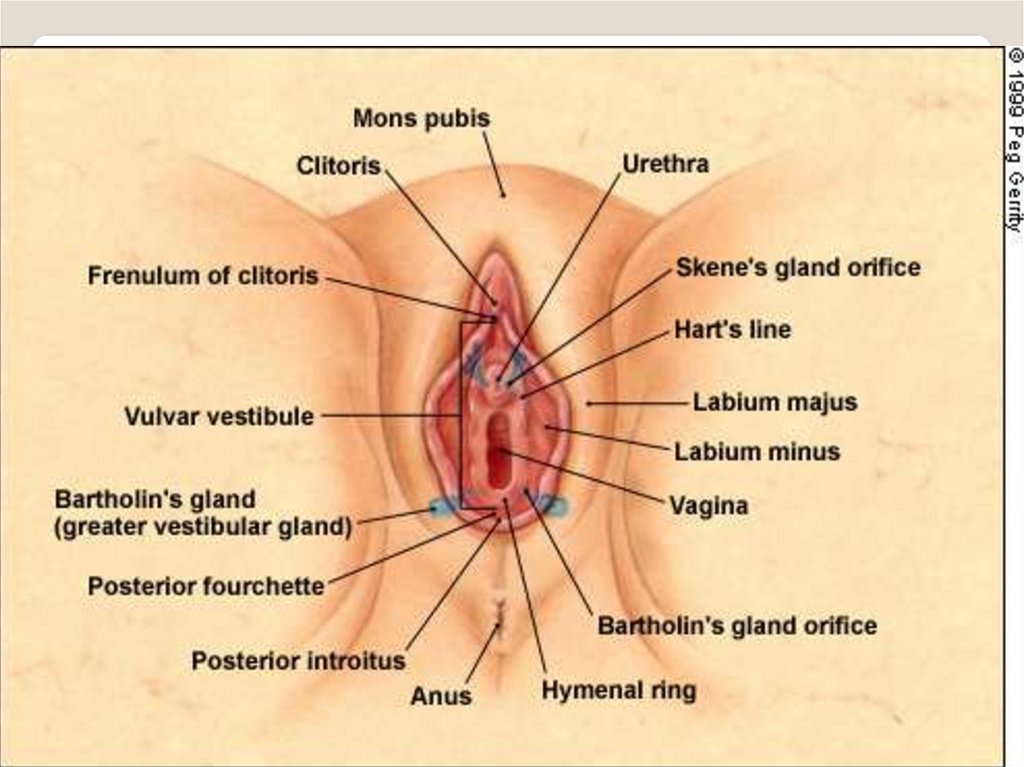
2. Vulval anatomy
The vulva (external genitalia ) includes:Mons pubis
clitoris
labia majora and minora
Perineum: a less hairy skin & subcutaneous tissue
area lying between the vaginal orifice & the anus &
covering the perineal body. Its length is 2-5 cm or
more. The urethra opens on to it.
Vestibule: a forecourt or a hall next to the
entrance. It is the area of smooth skin lying within
the L. minora & in front of the vaginal orifice.
Hymen.
3.
4. Non-neoplastic epithelial disorders
Classification:1. Lichen sclerosis.
2. Squamous cell hyperplasia (formerly:
hyperplastic dystrophy).
3. Other dermatoses.
- lichen planus.
- psoriasis.
- seborrhoeic dermatitis
- inflammatory dermatoses.
- ulcerative dermatoses.
5. Lichen sclerosus
Comprises 70% of benign epithelial disorders→ epithelial thinning, inflammation &
histological changes in the dermis.
Aetiology: unknown
Sx: Itching (commonest), vaginal soreness +
Dyspareunia. Burning and pain are uncommon.
Signs: crinkled skin, L. minora atrophy,
constriction of V. orifice, adhesions,
ecchymoses & fissures.
Dx: Biopsy is mandatory
Rx: - emollients, topical steroids.
- Testosterone: not effective than petroleum jelly
& → pruritus, pain & virilization.
- Surgery: avoided unless malignant changes
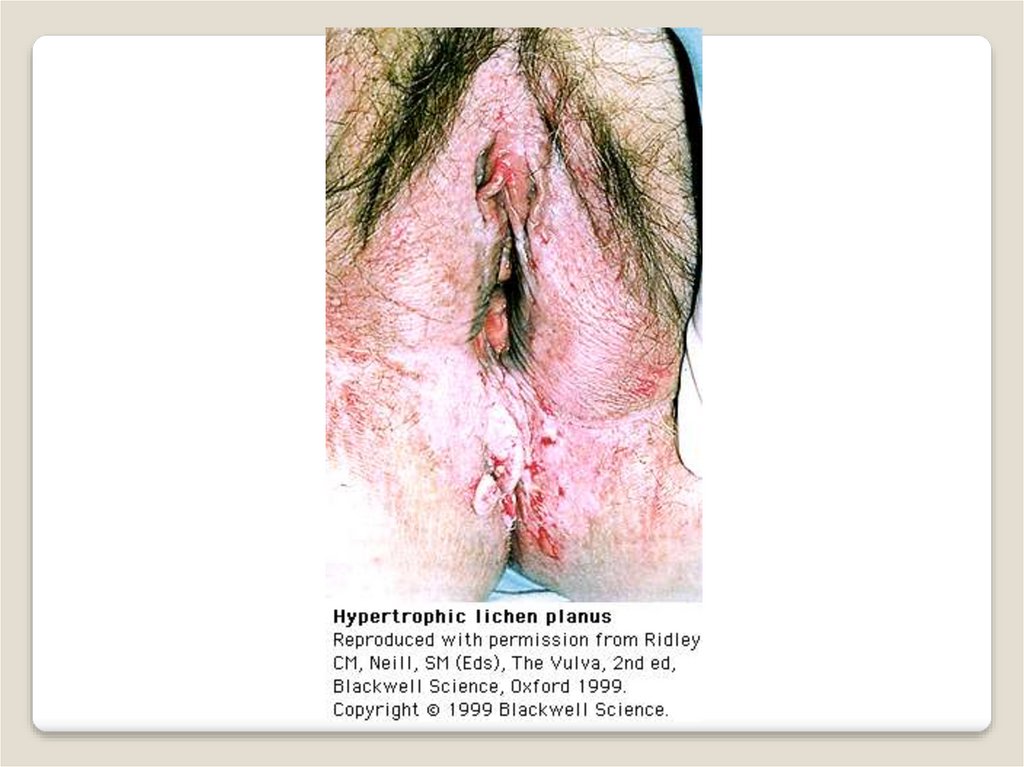
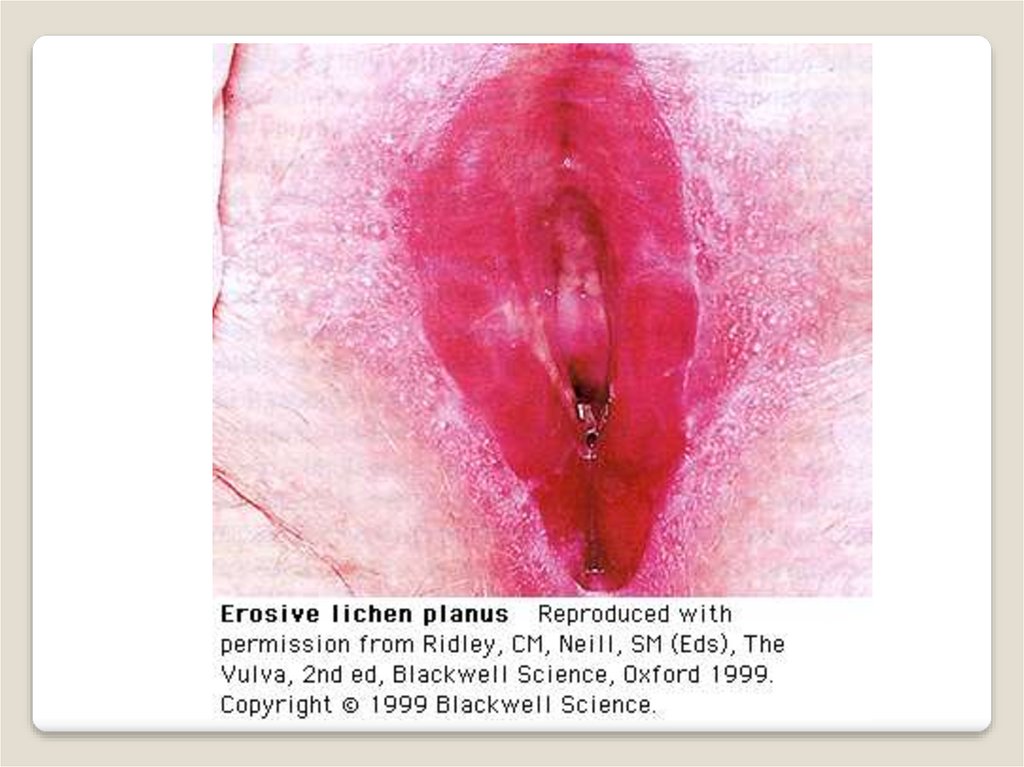
6. Lichen Planus
General Appearance◦ Erosive lesions at vestibule w/without
adhesions resulting in stenosis
◦ May have associated oral mucotaneous
lesions and desquamative vaginitis
◦ Patient c/o irritating vaginal , vulvar
soreness, intense burning, pruritus, and
dyspareunia w/post-coital bleeding
◦ Types: Papulosquamous
LP/Hypertrophophic LP /Errosive LP
7. Treatment
Intravaginal hydrocortisonesuppositories BID x 2m
Steroid creams (medium-high potency)
Vaginal estrogen cream if atrophic
epithelium present
Vaginal dilators for stenosis
Surgery for severe vaginal synechiae
Vulvar hygiene
Emotional support
8.
9.
10.
11. Vulvar Psoriasis
Physical Appearance◦ Red moist lesions w/without scales
Treatment: Topical corticosteroids
12.
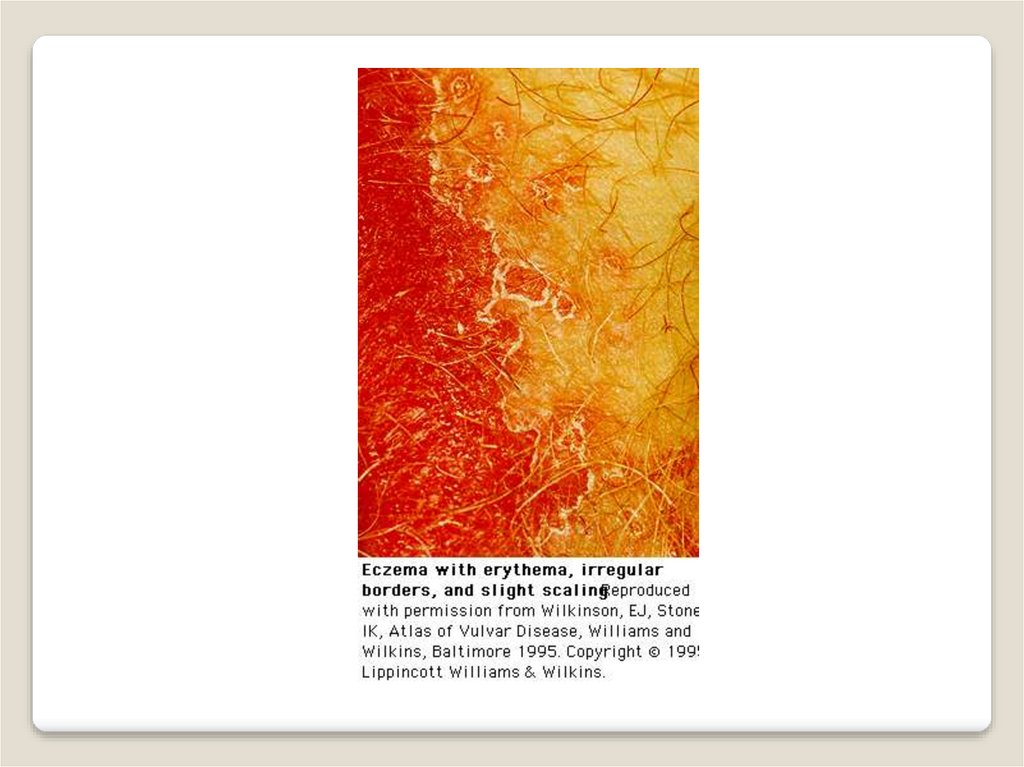
13. Squamous Cell Hyperplasia (Atopic Eczema/Neurodermatitis)
Physical AppearanceBenign epithelial thickening and hyperkeratosis
◦ Acute phase with red/moist lesions
◦ Causing pruritus leading to rubbing &
scratching
◦ Circumscribed, single or unifocal
◦ Raised white lesions on vulva or labia
majora and clitoris
Treatment: Sitz baths, lubricants, oral
antihistamines, Medium potency
topical steroid twice daily
14.
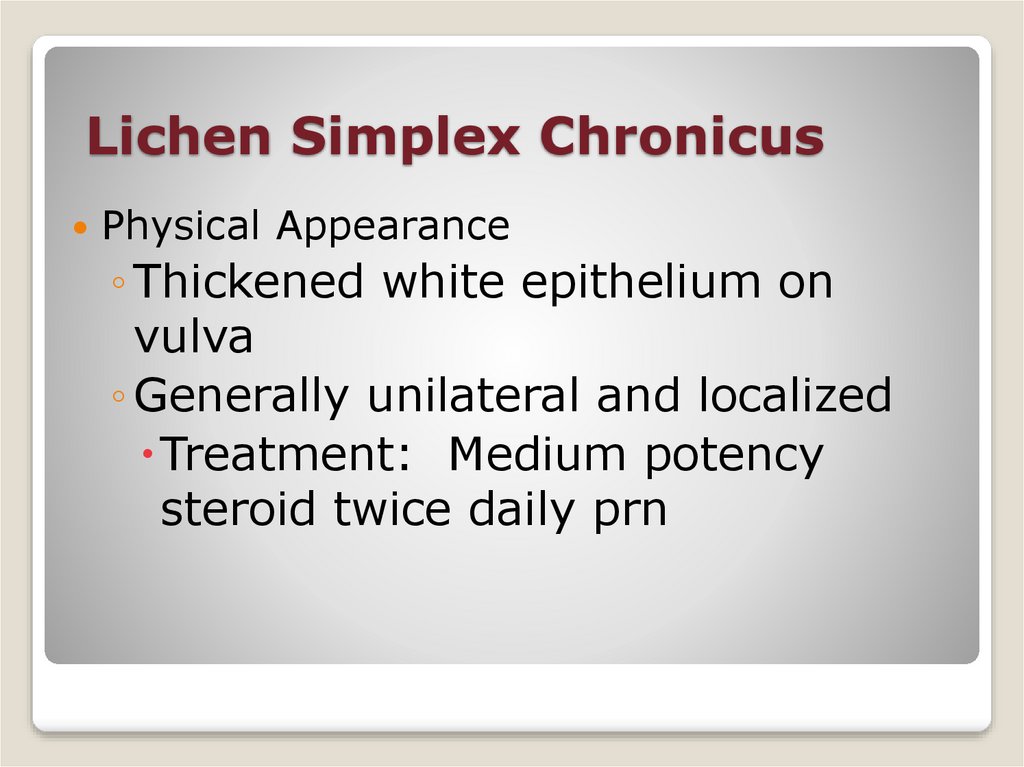
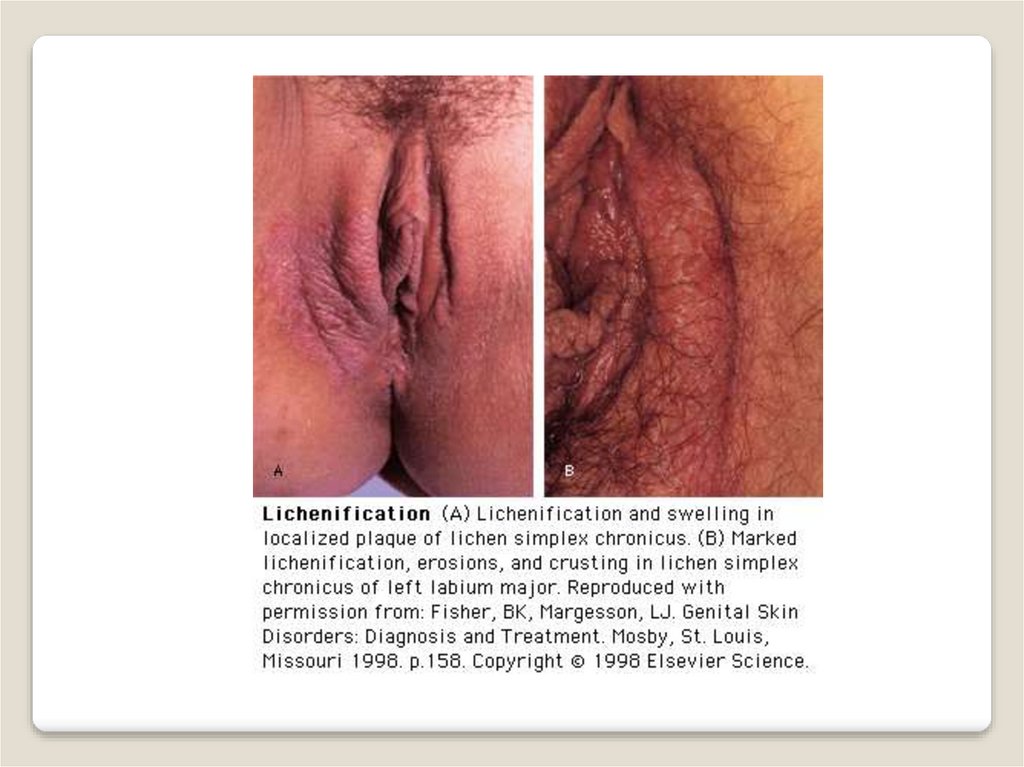
15. Lichen Simplex Chronicus
Physical Appearance◦ Thickened white epithelium on
vulva
◦ Generally unilateral and localized
Treatment: Medium potency
steroid twice daily prn
16.
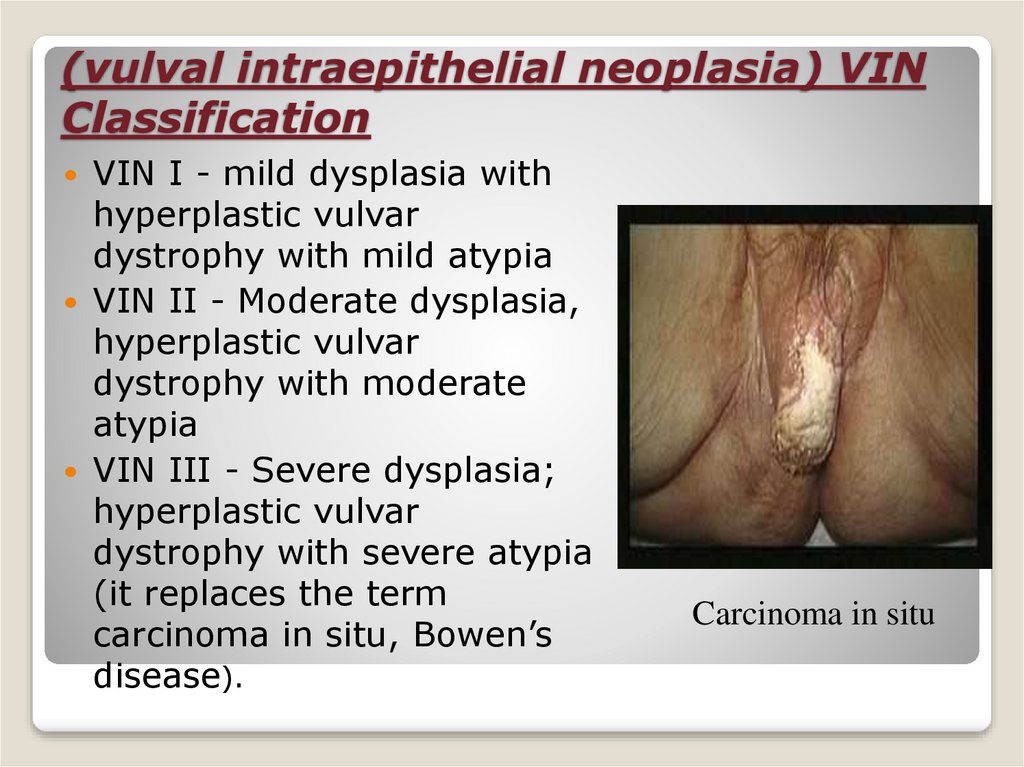
17. (vulval intraepithelial neoplasia) VIN Classification
VIN I - mild dysplasia withhyperplastic vulvar
dystrophy with mild atypia
VIN II - Moderate dysplasia,
hyperplastic vulvar
dystrophy with moderate
atypia
VIN III - Severe dysplasia;
hyperplastic vulvar
dystrophy with severe atypia
(it replaces the term
carcinoma in situ, Bowen’s
disease).
Carcinoma in situ
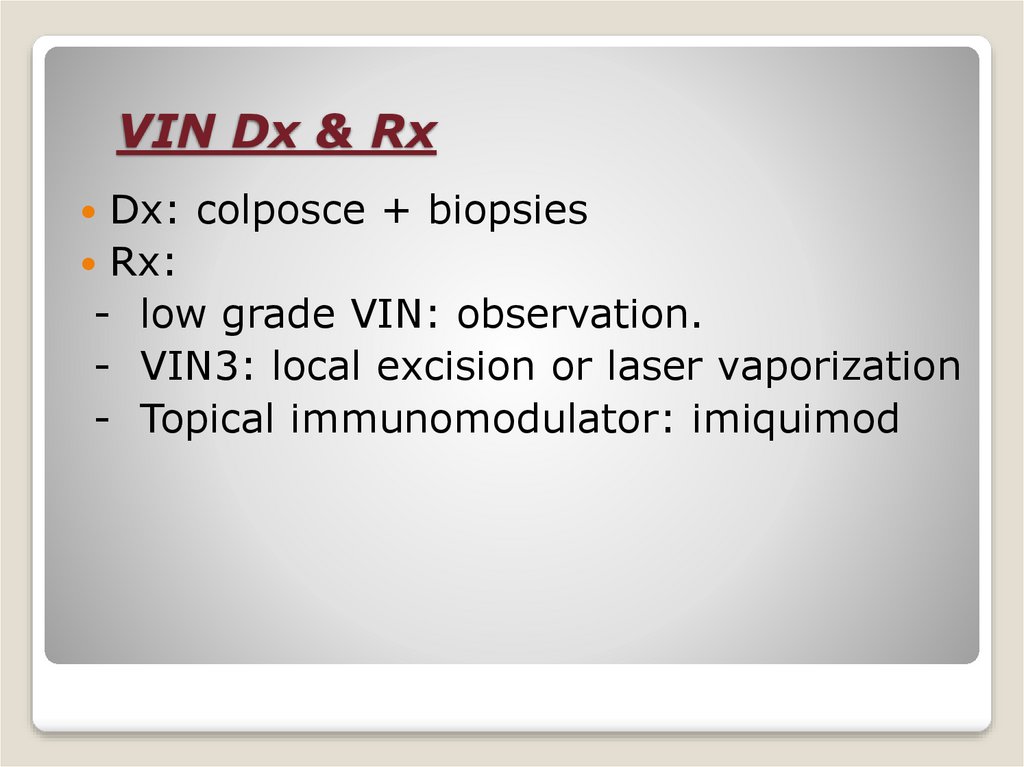
18. VIN Dx & Rx
VIN Dx & RxDx: colposce + biopsies
Rx:
- low grade VIN: observation.
- VIN3: local excision or laser vaporization
- Topical immunomodulator: imiquimod