Similar presentations:
Paediatric Anaesthesia
1. Paediatric Anaesthesia
2. Introduction
• Children are not smalladults!
• Different physiology,
anatomy and
pharmacology,
therefore they have
specific anaesthetic
requirements
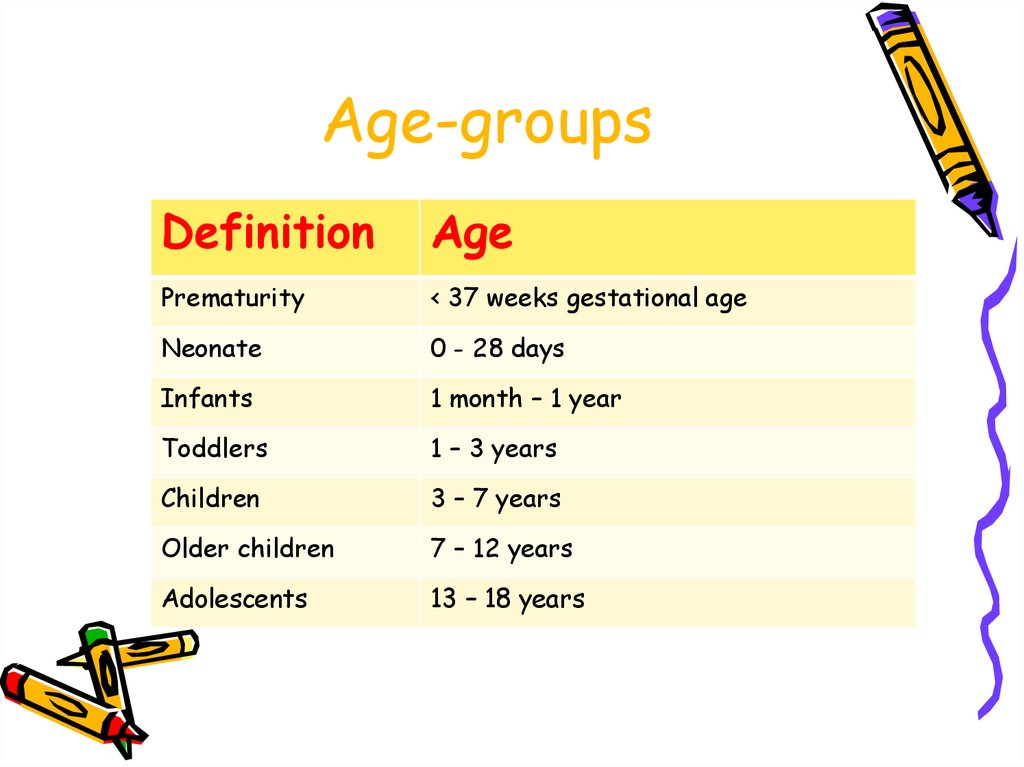
3. Age-groups
DefinitionAge
Prematurity
< 37 weeks gestational age
Neonate
0 - 28 days
Infants
1 month – 1 year
Toddlers
1 – 3 years
Children
3 – 7 years
Older children
7 – 12 years
Adolescents
13 – 18 years
4. Anatomy and physiology
5. CVS
• The differences are most marked in theneonate
– Non-compliant and poorly developed myocardium
– Fixed stroke volume ∴ CO is HR-dependent
– Vagal tone dominant at sino-atrial node→
bradycardias
– Immature baroreceptors
– Exclude congenital cardiac defects
6. Respiratory
• Anatomic differences• Obligate
nasal
breathing
under
•Large
floppy
head,
tongue
+6
months
epiglottis
• Small tidal volumes and rapid rate
•Narrowest
part of
the airway at
• O2 consumption:
6-9ml/kg/min
(adult 3-4ml/kg/min)
CRICOID
• ↓ed FRC++ cephalad
↓ed lung compliance
•Anterior
larynx
• Premature
neonates
are prone to
•Short
+ narrow
trachea
APNOEAS
•Prominent tonsils + adenoids
7. Haematology
• Blood volume: 90-100 ml/kg - adultlevel (80 ml/kg) by age 1
• At birth Hb 18-20 g/dL + 75% foetal
Hb
• Physiologic anaemia at 2-3 months
• Coagulation may be affected in
neonate because of immature hepatic
function and reduced levels of
Vitamin A, D, E, K.
8. Liver
• Immature at birth• Metabolism is slow ∴action of
anaesthetic drugs may be prolonged
• Low glycogen stores in neonates –
hypoglycaemia
9. Renal
• Renal function is immature at birth• Drug clearance may be affected
10. CNS
• Neonates + small children experiencePAIN!
• Drug dosages are often reduced in
neonates
• MAC is normal or ↓ed in neonates, but
MAC ↑ed in older children
• Propofol dose increased in children
11. Thermoregulation
• Hyperthermia– Rare
– Children more prone to MH
• Hypothermia is a big concern
• Neonates and small babies have large
heads with a big surface area and large
organs close to the skin
– Significant heat loss occurs in theatre if not
actively prevented
12. Pre-operative Assessment
13. History
Complete medical + surgical
Time of last meal – NB
Medication
Allergies
Any previous reaction to anaesthesia or
FHx of problems
• Road-to-Health Cards
• Congenital abnormalities or syndromes
14. Examination
• Airway assessment is tricky• Routine general examination
• Exclude Upper or Lower Respiratory
Tract Infections (common!)
15. Pre-op plan + Premed
• Discussion with child and parents– If child is old enough to understand,
involve them and show them anaesthetic
apparatus to allay anxiety
• Verbal consent
• Premedication
– Not for children
under 6 months –
1 year old
16. Premedication
• Tailored to the child and the case• Simple re-assurance and explanation may
be sufficient
• Drugs (all per os)
–
–
–
–
–
Midazolam
Vallergan forte (trimeprazine)
Droperidol
Ketamine
Stopayne syrup (paracetamol, codeine and
phenergan)
17. Nil per os
• 6 hours – solid food or formula milk• 4 hours – breast milk
• 2 hours – clear fluid or juice
• Clear fluids are encouraged at Red
Cross until 2 hours
pre –op
– Prevents thirsty,
irritable,
hypoglycaemic child
18. Preparation of the Paediatric Theatre
19. Paediatric Equipment
Breathing circuits
Paediatric Ventilators
Face masks
Oropharyngeal airways
Laryngoscopes
Endotracheal Tubes
Introducer
• Magill’s Forceps
• LMA’s
• IV access cannulas,
CVPs and arterial
lines
• IVFluid + giving sets
• Nasogastric tubes +
urinary catheters
• Temperature probes
• Warming equipment
• Monitors
20. Breathing Circuits
• Jackson-Rees modification of theAyre’s t-piece
– Light-weight with no valves
– Reservoir bag
– FGF: 2-3x MV in spontaneous ventilation
• Paediatric circle
21. Airway equipment
• Paediatric specifications and sizesto meet the different anatomical needs
–
–
–
–
–
–
Facemasks
OPAs
Laryngoscopes
Suction catheters
Introducers + Magill's Forceps
LMAs
• ETTs
– Size range: 2.0 mm – 6.5 mm i.d.
– Uncuffed WHY?
– Size: 4 + age / 4 = i.d. ETT (mm)
22. Warming Equipment
Forced air warmer – “BAIR hugger”
Overhead radiant heaters
Ambient theatre temperature 22° C
Heated underblankets
Warm IV fluid
Paediatric HMEF (heat moisture exchange
filters)
• Hats, gamjees, plastic sheets to insulate
“Prevention is better than cure”
when it comes to HYPOTHERMIA
23. The Actual Anaesthetic
24. Induction
• Choice: inhalational vs. intravenous• At RXH: majority INHALATIONAL
– Preferable to young children to getting
a drip first!
• If EMLA or Ametop cream available,
IV Induction is a good option
• Older children can be given a choice
• Muscle Relaxation not used routinely
for intubation
25.
26. Maintenance
• Choice: inhalational or intravenous• NB Points in paeds:
–
–
–
–
Drug doses in mg/kg
Monitoring and vigilance
Temperature control
IV Fluids → 4:2:1 rule for maintenance;
plus remember rehydration for preexisting deficits and replacement of
ongoing losses
27. Analgesia
• Babies & children may not expresspain clearly, but they do feel pain
• Multi-modal approach
– Simple analgesics: paracetamol (PR, IV)
– NSAIDs: voltaren (diclofenac) (PR)
• Not for babies < 1 year
– Opiates: fentanyl, morphine, Valoron
(tilidene) drops
– Ketamine
– Regional procedures
• Caudals or epidurals
• Blocks (multiple)
• Wound infiltration with local anaesthesia
28. Emergence & Recovery
Emergence & Recovery• Potential for many complications at
this point
– Obstructed airway
– laryngospasm
• Recovery
– Recovery position
– Monitoring
• Discharge criteria
Awake and maintaining airway
Normal vital signs
Pain free
No PONV
No surgical complications
29. Guidelines for Referral
• Doctors not familiar withanaesthetising children should not do so
• No child under age of 3 should be
anaesthetised by a MO without senior
supervision
• Must have paediatric equipment,
otherwise refer to a centre that does
• Refer
–
–
–
–
Sick kiddies
Anticipated Airway problems
Organ failure
Syndromic – often have multiple congenital abnormalities (CVS!)

















 medicine
medicine