Similar presentations:
Arterial hypertension
1. Arterial hypertension
2. Definition
Arterial hypertension (WHO, 1999) is aconstantly increased systolic ( 140
mmHg) and/or diastolic BP ( 90 mmHg)
Secondary (symptomatic) AH is a
hypertension, the cause of which can be
revealed, therefore this is a syndrome of
the underlying primary disease
3. Definition
Hypertension is defined as values ≥140mmHg SBP and/or ≥90 mmHg DBP, based
on the evidence from RCTs that in patients
with these BP values treatment-induced BP
reductions are beneficial.
RCT - randomized controlled trials
4. Why do we take care of arterial hypertension?
“Silent killer of XXIcentury”
Major cardiovascular
risk factor, that directly
contributes to MI, CHF,
cerebrovascular
accidents, peripheral
arterial insufficiency,
and premature mortality
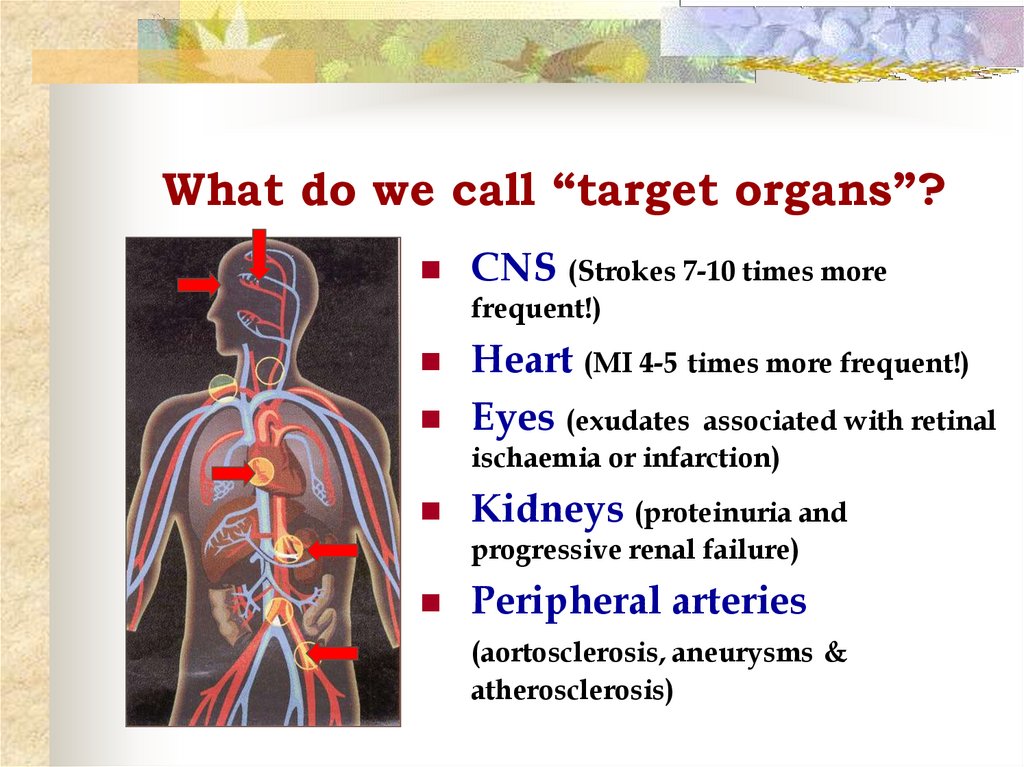
5. What do we call “target organs”?
CNS (Strokes 7-10 times morefrequent!)
Heart (MI 4-5 times more frequent!)
Eyes (exudates associated with retinal
ischaemia or infarction)
Kidneys (proteinuria and
progressive renal failure)
Peripheral arteries
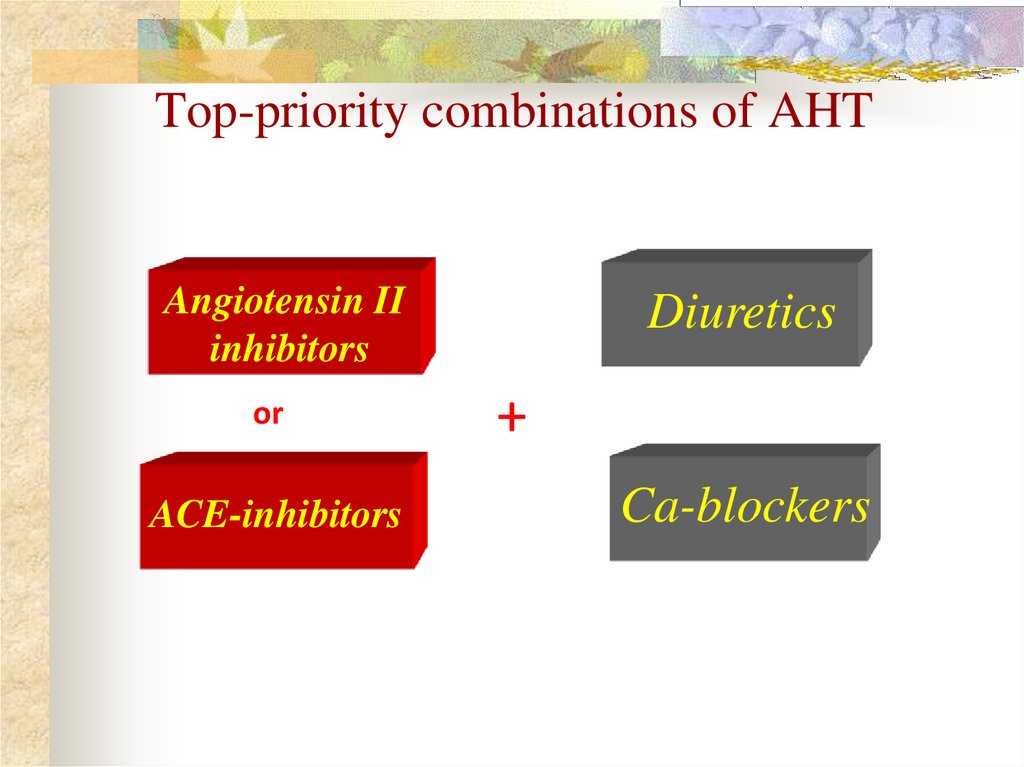
(aortosclerosis, aneurysms &
atherosclerosis)
6. Hypertension in the world
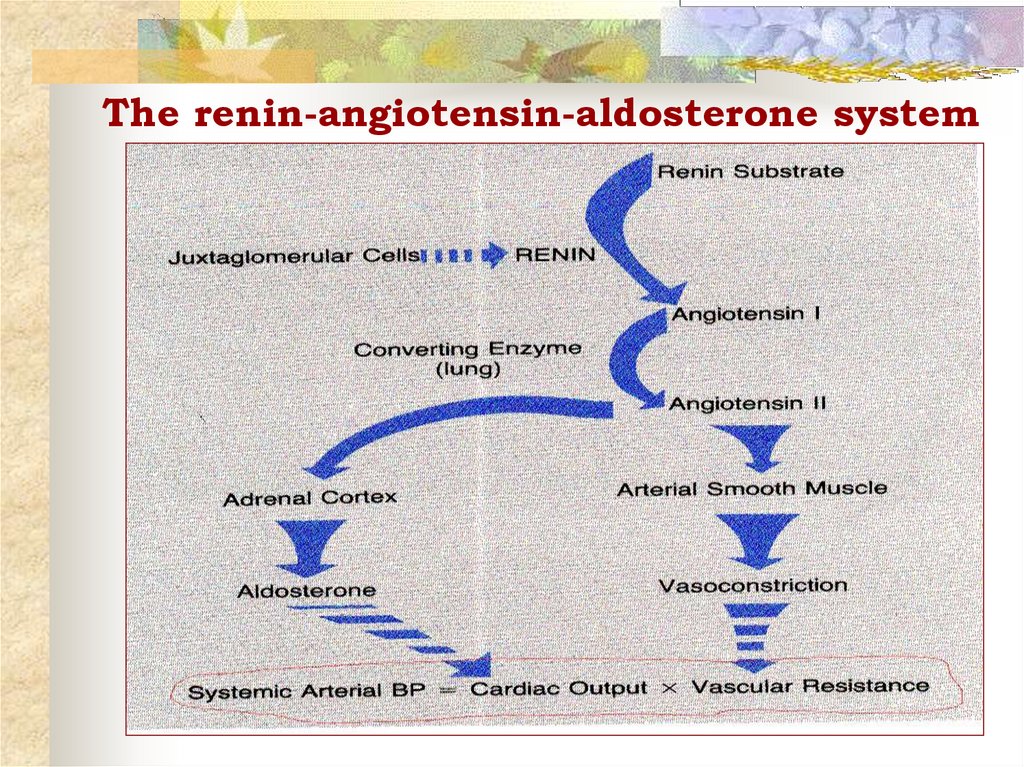
33% of the population in USA,43-44% in Russia,more than 41,5
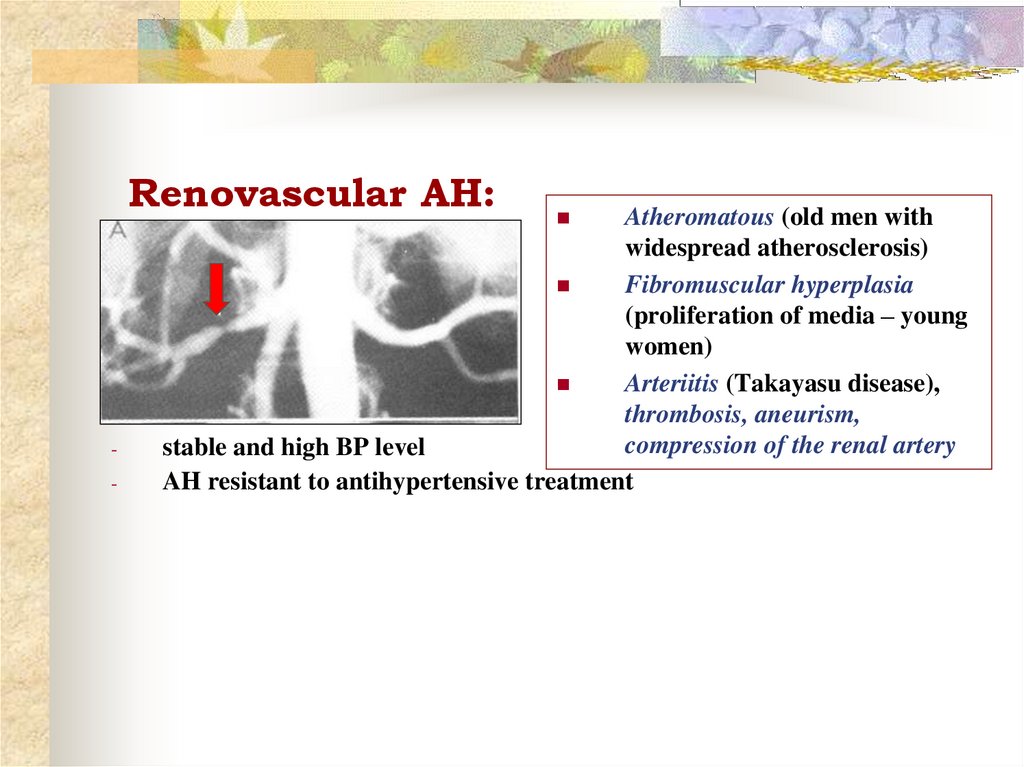
million.
7. Prevalence of hypertension
Overall the prevalence of hypertensionappears to be around 30–45% of the general
population, with a steep increase with ageing
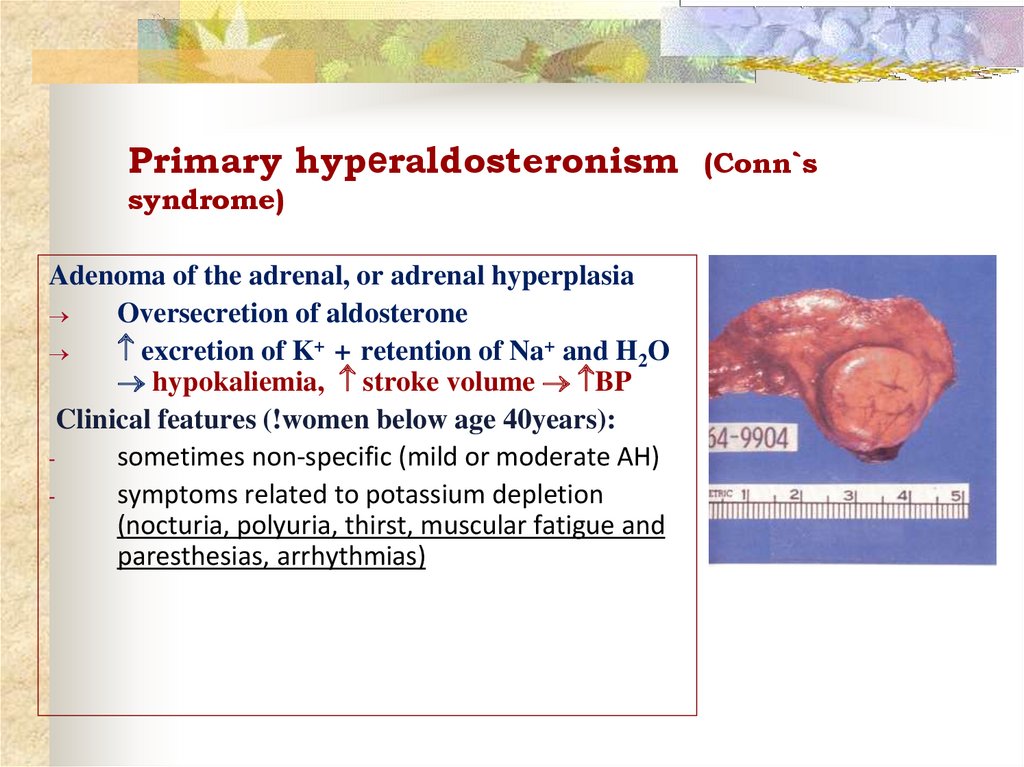
(>65 years – 60 – 70 % )
A close relationship between prevalence of
hypertension and mortality for stroke has
been reported. The incidence and trends of
stroke mortality in Europe have been analysed
by use of World Health Organization (WHO)
statistics.
8. Report of World Health Organization
In 2020 AD, 2.6 million Indians are predicted to diedue to coronary heart disease which constitutes 54.1 %
of all CVD deaths
The Sentinel Surveillance Project, documented 28%
overall prevalence of hypertension from 10 regions
of India in the age group 20-69.
9. Hypertension in Nigeria
Prevalence of hypertension 28.7%.Hypertension prevalence was
comparable in men and women
(29.9% versus 28.0%).
Hypertension was more
prevalent in semi-urban than
rural villagers (32.9% versus
24.1%).
10. Hypertension: Predisposing factors
Age > 60 yearsSex (men and postmenopausal women)
Family history of cardiovascular disease
Smoking
High cholesterol diet
Co-existing disorders such as diabetes,
obesity and hyperlipidaemia
High intake of alcohol
Sedentary life style
11. Structure of the diagnosis of AH
Primary (essential hypertension)or secondary (symptomatic)
Degree (according to BP level)
Stage (depends on impairment of
target-organs)
Stratification of risk for
individual
12. Structure of AH
94-95% constitute primary AH (essentialhypertension)
5-6% - secondary AH
1-2% others
4-5%
Renal parenchimal
diseases
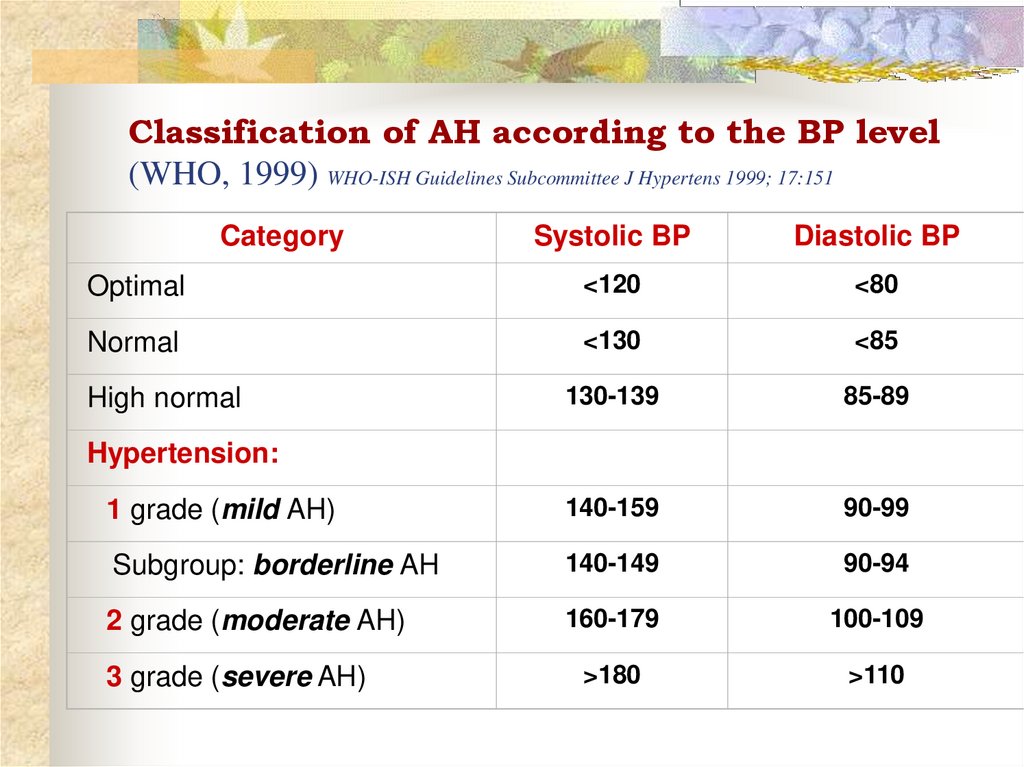
13. Classification of AH according to the BP level (WHO, 1999) WHO-ISH Guidelines Subcommittee J Hypertens 1999; 17:151
CategorySystolic BP
Diastolic BP
Optimal
<120
<80
Normal
<130
<85
130-139
85-89
1 grade (mild AH)
140-159
90-99
Subgroup: borderline AH
140-149
90-94
2 grade (moderate AH)
160-179
100-109
>180
>110
High normal
Hypertension:
3 grade (severe AH)
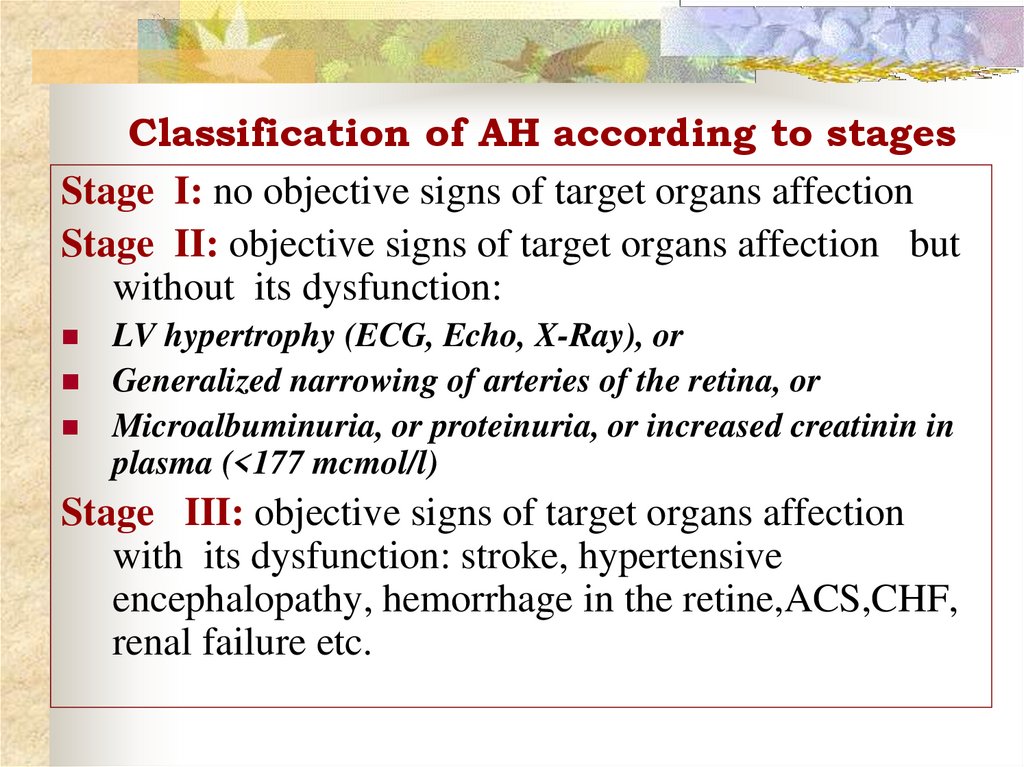
14. Classification of AH according to stages
Stage I: no objective signs of target organs affectionStage II: objective signs of target organs affection but
without its dysfunction:
LV hypertrophy (ECG, Echo, X-Ray), or
Generalized narrowing of arteries of the retina, or
Microalbuminuria, or proteinuria, or increased creatinin in
plasma (<177 mcmol/l)
Stage III: objective signs of target organs affection
with its dysfunction: stroke, hypertensive
encephalopathy, hemorrhage in the retine,ACS,CHF,
renal failure etc.
15. Assessment of total cardiovascular risk
The concept is based on the fact that only asmall
fraction of the hypertensive
population has an elevation of BP alone,
with the majority exhibiting additional
CVrisk factors.
16. Assessment of total cardiovascular risk
Estimation of total CV risk is easy in particular subgroupsof patients,such as those with antecedents of established
cardiovascular disease (CVD), diabetes,CHDor with
severely elevated single risk factors. In all of these
conditions, the total CV risk is high or very high, calling
for intensive CV risk-reducing measures. However, a large
number of patients with hypertension do not belong to any
of the above categories and the identification of those at
low, moderate, high or very high risk requires the use of
models to estimate total CV risk, so as to be able to adjust
the therapeutic approach accordingly
17. Assessment of total cardiovascular risk
The classification in low, moderate, highand very high risk is retained in the current
guidelines and refers to the 10-year risk of
CV mortality as defined by the 2012 ESC
prevention guidelines . The factors on
which the stratification is based are
summarized in next page.
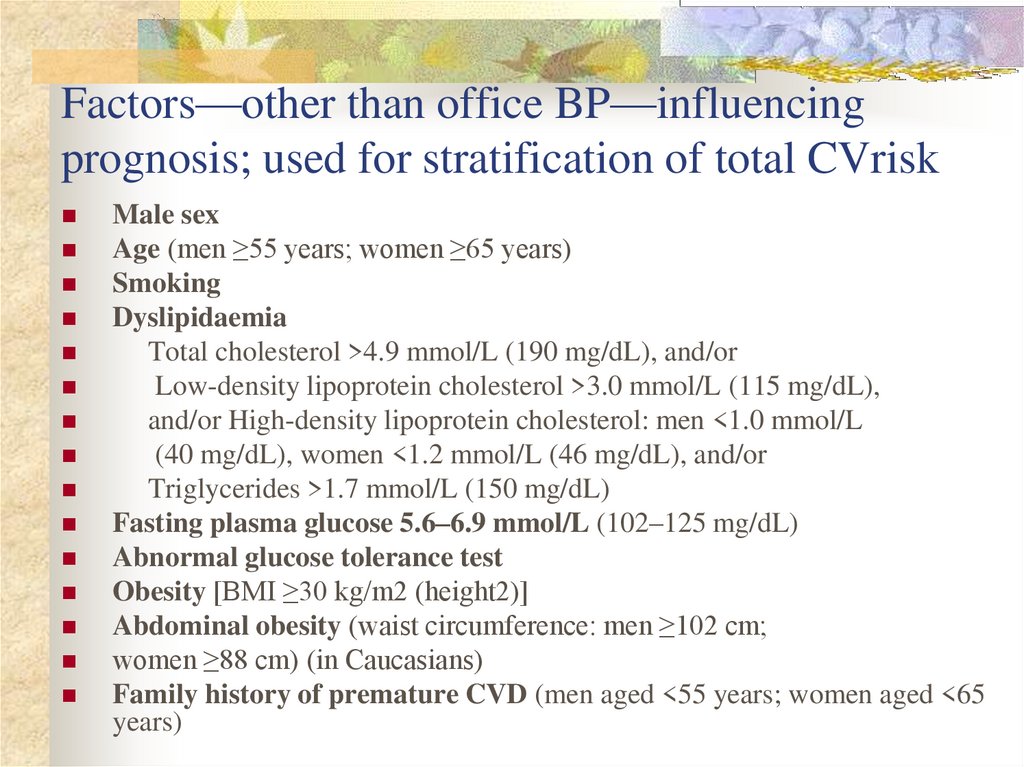
18. Factors—other than office BP—influencing prognosis; used for stratification of total CVrisk
Male sexAge (men ≥55 years; women ≥65 years)
Smoking
Dyslipidaemia
Total cholesterol >4.9 mmol/L (190 mg/dL), and/or
Low-density lipoprotein cholesterol >3.0 mmol/L (115 mg/dL),
and/or High-density lipoprotein cholesterol: men <1.0 mmol/L
(40 mg/dL), women <1.2 mmol/L (46 mg/dL), and/or
Triglycerides >1.7 mmol/L (150 mg/dL)
Fasting plasma glucose 5.6–6.9 mmol/L (102–125 mg/dL)
Abnormal glucose tolerance test
Obesity [BMI ≥30 kg/m2 (height2)]
Abdominal obesity (waist circumference: men ≥102 cm;
women ≥88 cm) (in Caucasians)
Family history of premature CVD (men aged <55 years; women aged <65
years)
19. Factors—other than office BP—influencing prognosis; used for stratification of total CVrisk
Asymptomatic organ damage:Pulse pressure (in the elderly) ≥60 mmHg
Electrocardiographic LVH (Sokolow–Lyon index >3.5
mV;RaVL >1.1 mV; Cornell voltage duration product >244
mV*ms), or
Echocardiographic LVH [LVM index: men >115 g/m2;women
>95 g/m2 (BSA)]
Carotid wall thickening (IMT >0.9 mm) or plaque
Carotid–femoral PWV >10 m/s
Ankle-brachial index <0.9
CKD with eGFR 30–60 mL/min/1.73 m2 (BSA)
Microalbuminuria (30–300 mg/24 h), or albumin–creatinine ratio
(30–300 mg/g; 3.4–34 mg/mmol) (preferentially on morning spot
urine)
20. Factors—other than office BP—influencing prognosis; used for stratification of total CVrisk
Diabetes mellitus:Fasting plasma glucose ≥7.0 mmol/L (126 mg/dL) on two
repeated
measurements, and/or HbA1c >7% (53 mmol/mol), and/or
Post-load plasma glucose >11.0 mmol/L (198 mg/dL)
Established CV or renal disease:
Cerebrovascular disease: ischaemic stroke; cerebral
haemorrhage; transient ischaemic attack
CHD: myocardial infarction; angina; myocardial
revascularization with PCI or CABG
Heart failure, including heart failure with preserved EF
Symptomatic lower extremities peripheral artery disease
CKD with eGFR <30 mL/min/1.73m2 (BSA); proteinuria (>300
mg/24 h).
Advanced retinopathy: haemorrhages or exudates, papilloedema
21.
22. MEASUREMENT OF BLOOD PRESSURE
Use a machine that has been validated,well maintained and properly calibrated
Measure sitting BP routinely, with
additional standing BP in elderly and
diabetics
Remove tight clothing from the arm
Support arm at level of the heart
Lower mercury slowly (2 mm per
second)
Read BP to the nearest 2 mmHg
Use phase V (disappearance of
sounds) to measure diastolic BP
Take two measurements at each visit
23. Types of measurement:
Office BPHome BP
Daily monitoring
of BP!!!
24. ‘White coat‘ hypertension?
Up to 13-15% ofapparent hypertension
in the clinic may
'normal BP' when it is
recorded by automated
used in their own home
25. Classification of secondary AH
1. Renal:Renal parenchymal,
Renovascular
Anephric
2. Endocrinological:
Cushing`s syndrome and disease
Primary aldosteronism
Pheochromacytoma
Primary hypothyroidism
Hyperthyroidism
Acromegaly
Hyperparathyroidism
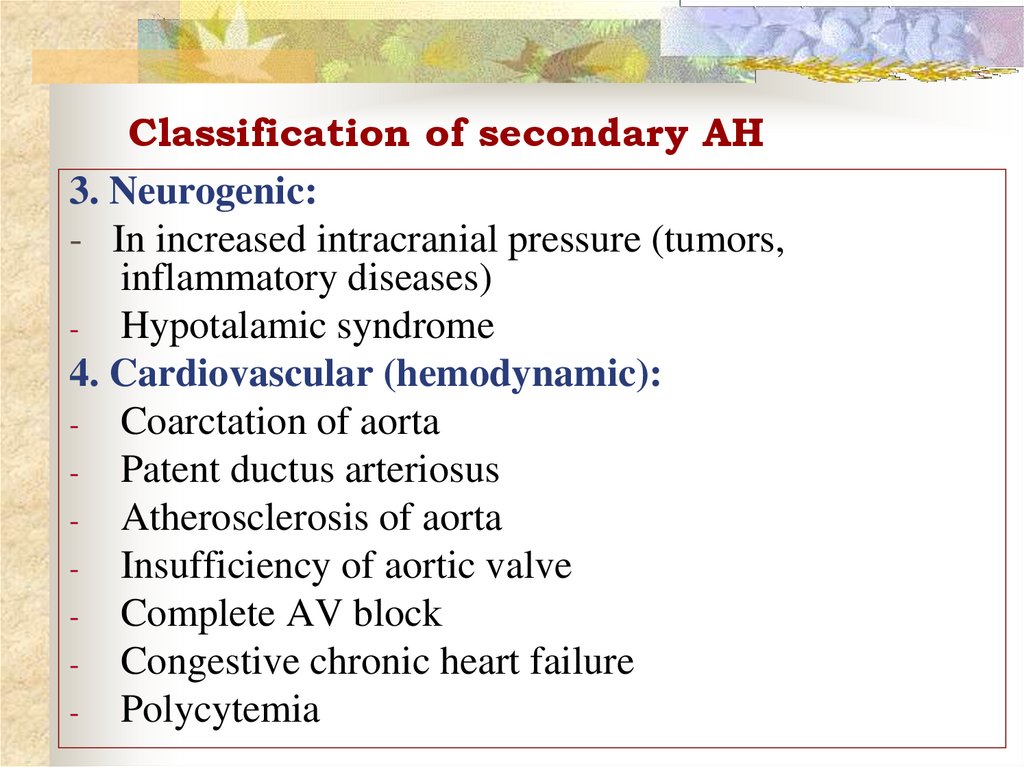
26. Classification of secondary AH
3. Neurogenic:- In increased intracranial pressure (tumors,
inflammatory diseases)
- Hypotalamic syndrome
4. Cardiovascular (hemodynamic):
- Coarctation of aorta
- Patent ductus arteriosus
- Atherosclerosis of aorta
- Insufficiency of aortic valve
- Complete AV block
- Congestive chronic heart failure
- Polycytemia
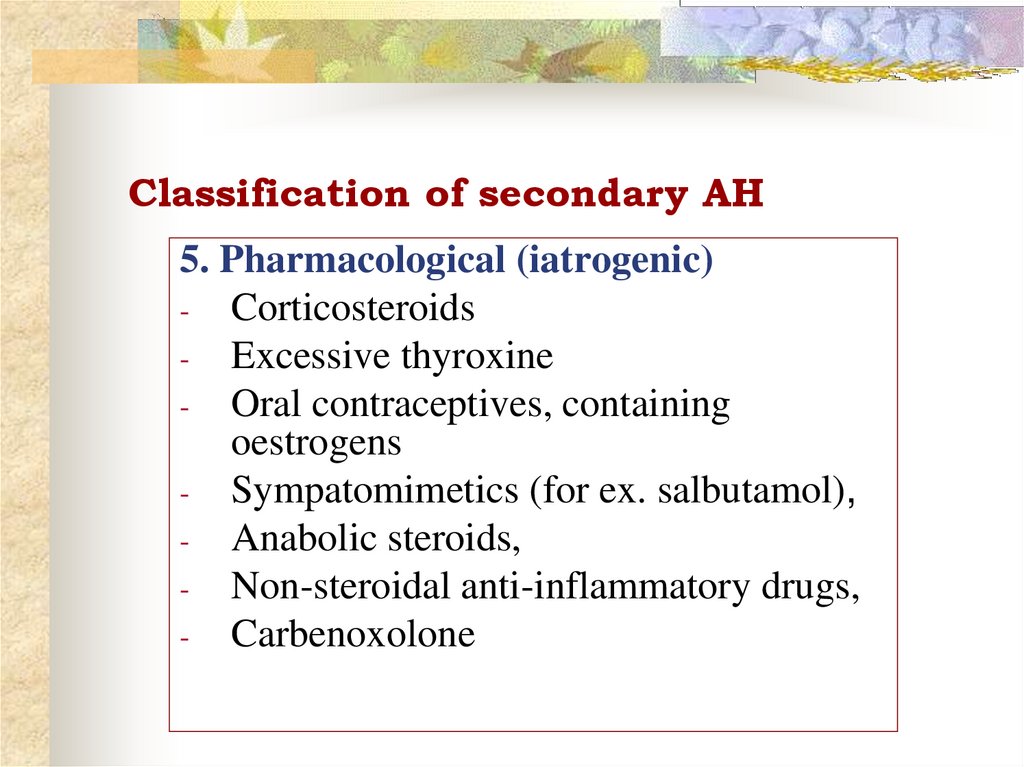
27. Classification of secondary AH
5. Pharmacological (iatrogenic)- Corticosteroids
- Excessive thyroxine
- Oral contraceptives, containing
oestrogens
- Sympatomimetics (for ex. salbutamol),
- Anabolic steroids,
- Non-steroidal anti-inflammatory drugs,
- Carbenoxolone
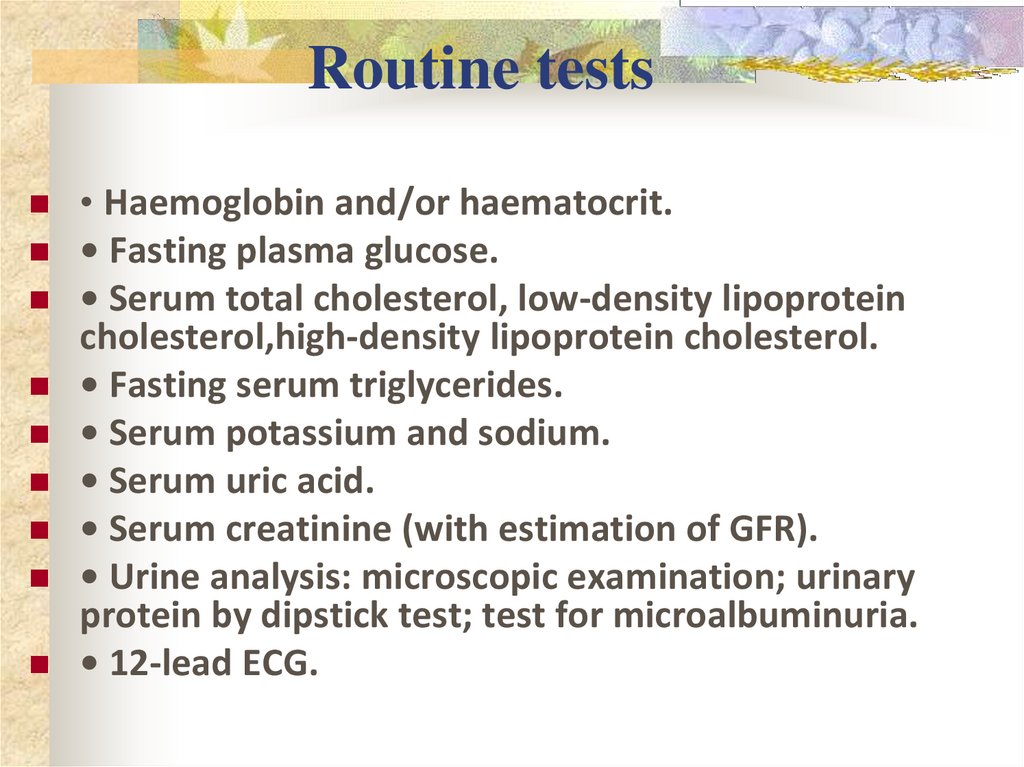
28. Routine tests
• Haemoglobin and/or haematocrit.• Fasting plasma glucose.
• Serum total cholesterol, low-density lipoprotein
cholesterol,high-density lipoprotein cholesterol.
• Fasting serum triglycerides.
• Serum potassium and sodium.
• Serum uric acid.
• Serum creatinine (with estimation of GFR).
• Urine analysis: microscopic examination; urinary
protein by dipstick test; test for microalbuminuria.
• 12-lead ECG.
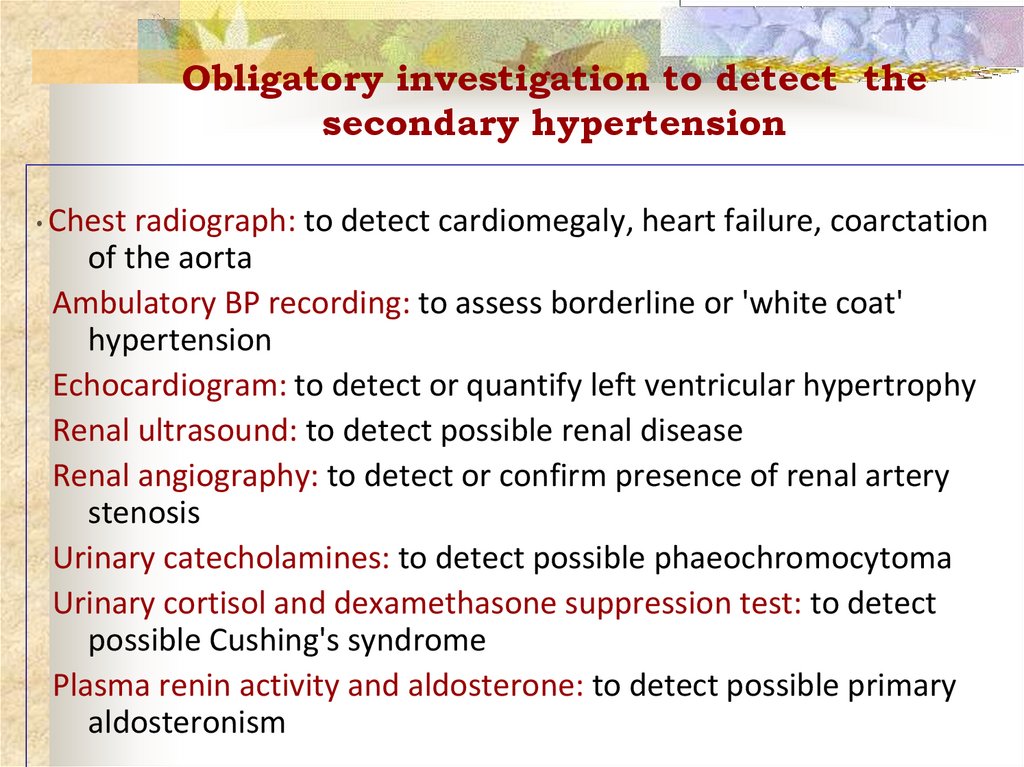
29. Obligatory investigation to detect the secondary hypertension
• Chestradiograph: to detect cardiomegaly, heart failure, coarctation
of the aorta
Ambulatory BP recording: to assess borderline or 'white coat'
hypertension
Echocardiogram: to detect or quantify left ventricular hypertrophy
Renal ultrasound: to detect possible renal disease
Renal angiography: to detect or confirm presence of renal artery
stenosis
Urinary catecholamines: to detect possible phaeochromocytoma
Urinary cortisol and dexamethasone suppression test: to detect
possible Cushing's syndrome
Plasma renin activity and aldosterone: to detect possible primary
aldosteronism
30. Life style modifications
Lose weight, if overweightLimit alcohol intake
Increase physical activity
Reduce salt intake
Stop smoking
Limit intake of foods rich in fats
and cholesterol
31. Principles of treatment
1. Etiological: elimination of causes2. Non-pharmacological treatment: weight reduction, stop alcogol
and tobacco smoking, restriction of the sodium intake
3. Pathogenetic pharmacotherapy:
Long-term, lifelong administration of antihypertensive drugs
Long-acting drugs 1-2 times a day
Combined prescription of 2-3 preparations
β-blockers
Diuretics
Ca-blockers
ACE-inhibitors
Angiotensin II inhibitors
32. Treatment strategies
1) Treatment is permanent and continuous2) Begin treatment with a minimal dose and
gradually increase to reduce blood pressure
3) Gradually decrease of blood pressure
4) The choice of the drug taking accordingly
hemodynamics, coronary insufficiency,
arrhythmias, CVD risk factors, target organs
damage, concomitant diseases
5) Stepwise therapy
6) Rational combinations
7) Prolonged drugs use
33. Top-priority combinations of AHT
Angiotensin IIinhibitors
or
ACE-inhibitors
Diuretics
+
Ca-blockers
34. Renal parenchymal AH:
-chronic glomerulonephritis,
pyelonephritis,
polycystic renal disease,
diabetic nephropathy,
congenital diseases of kidneys,
vasculitis in systemic connective tissue diseases,
amyloidosis of kidneys,
renal tumors:
Manifestations:
-
-
pain in the loin,
intoxication and fever,
dysuria (frequent micturition, nocturia),
renal edemas, nephrotic syndrome,
symptoms of chronic renal failure,
35. Diagnostics of renal parenchymal diseases
urinary syndrome (proteinuria, leucocyturia, hematuria,cylindruria, bacteriuria),
testing of the renal function (glomerular filtration rate,
isotopic renography),
instrumental diagnostics (excretory urography, USI of
kidneys, radionuclide renoscintigraphy, MRI, biopsy)
Pathogenesis: involvement of the RAA
system
36. The renin-angiotensin-aldosterone system
37. Renovascular AH:
-Atheromatous (old men with
widespread atherosclerosis)
Fibromuscular hyperplasia
(proliferation of media – young
women)
Arteriitis (Takayasu disease),
thrombosis, aneurism,
compression of the renal artery
stable and high BP level
AH resistant to antihypertensive treatment
38. Diagnostics and treatment of renovascular desease
Auscultation: murmur in the paraumbilical regionRenal arteriogram
Doppler-echocardiography of the renal vessels !!!!
CT
Renin level in renal vein
Treatment: Surgical revascularization (Renal
percutaneous transluminal angioplasty)
Therapeutic (long-term antihypertensive
drugs)
39. Pheochromacytoma
Rare tumor of chromaffin cells (adrenal medulla of the kidneys orthe sympathetic ganglia in the abdomen or the chest) hypersecretion of
norepinephrine and epinephrine Arterial hypertension with crises
Clinical features:
Paroxismal sweating, flushing, palpitation
Orthostasis ( BP in the supine position, BP when standing up)
Weight loss
Intermittent or sustained hypertension
Fast reduction of symptoms by phentolamin
40. Diagnostics and treatment of Pheochromacytoma
Diagnosis:1.
2.
3.
4.
Elevated urinary excretion of vanillylmandelic acid
(VMA) and metanephrine
Hyperglycemia, glucosuria
USI of kidneys
CT, MRI
Treatment: Surgical removal of the tumor +
phentolamin, β-blockers
41. Primary hypеraldosteronism (Conn`s syndrome)
Primary hypеraldosteronismsyndrome)
Adenoma of the adrenal, or adrenal hyperplasia
Oversecretion of aldosterone
excretion of K+ + retention of Na+ and H2O
hypokaliemia, stroke volume BP
Clinical features (!women below age 40years):
sometimes non-specific (mild or moderate AH)
symptoms related to potassium depletion
(nocturia, polyuria, thirst, muscular fatigue and
paresthesias, arrhythmias)
(Conn`s
42. Diagnostics and treatment of Conn`s syndrome
Diagnosis:1.
Hypokaliemia (<3,5 μmol/l), Na+ in serum
2.
Renin, Aldosterone in plasma
3.
Identification of a tumor by USI, CT or adrenal
scintiscan (I131)
Treatment of hyperplasia: Antihypertensive therapy
including spironolactone (the aldosterone antagonist)
Treatment of adenoma: resection of the adrenal tumor
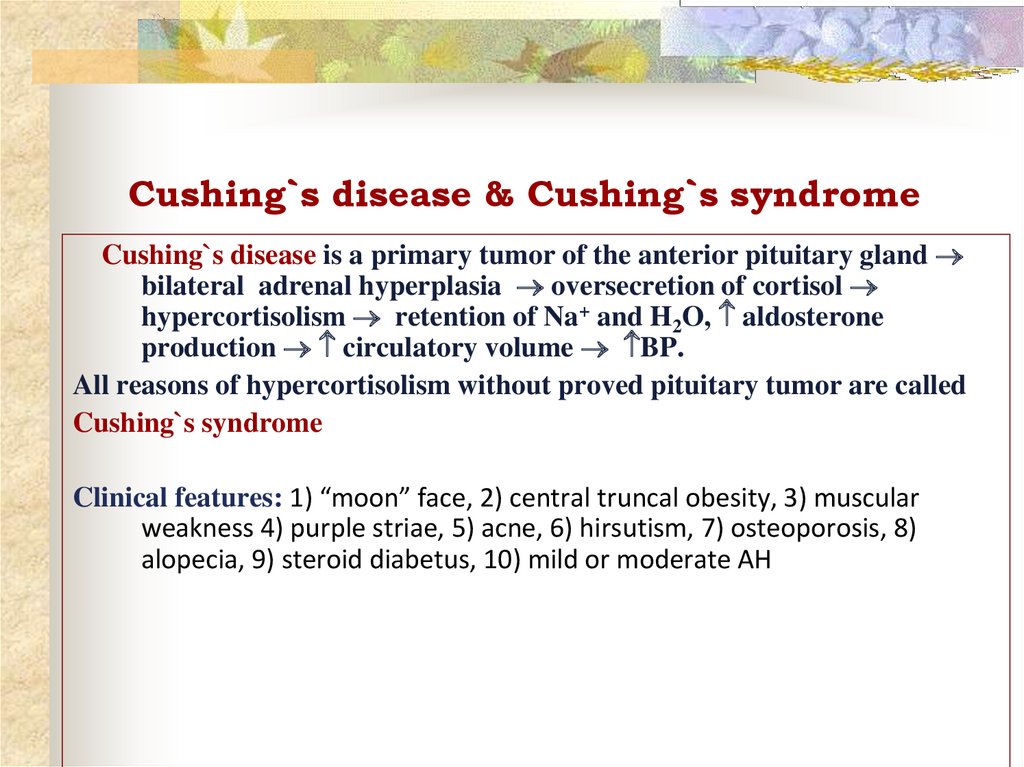
43. Cushing`s disease & Cushing`s syndrome
Cushing`s disease & Cushing`s syndromeCushing`s disease is a primary tumor of the anterior pituitary gland
bilateral adrenal hyperplasia oversecretion of cortisol
hypercortisolism retention of Na+ and H2O, aldosterone
production circulatory volume BP.
All reasons of hypercortisolism without proved pituitary tumor are called
Cushing`s syndrome
Clinical features: 1) “moon” face, 2) central truncal obesity, 3) muscular
weakness 4) purple striae, 5) acne, 6) hirsutism, 7) osteoporosis, 8)
alopecia, 9) steroid diabetus, 10) mild or moderate AH
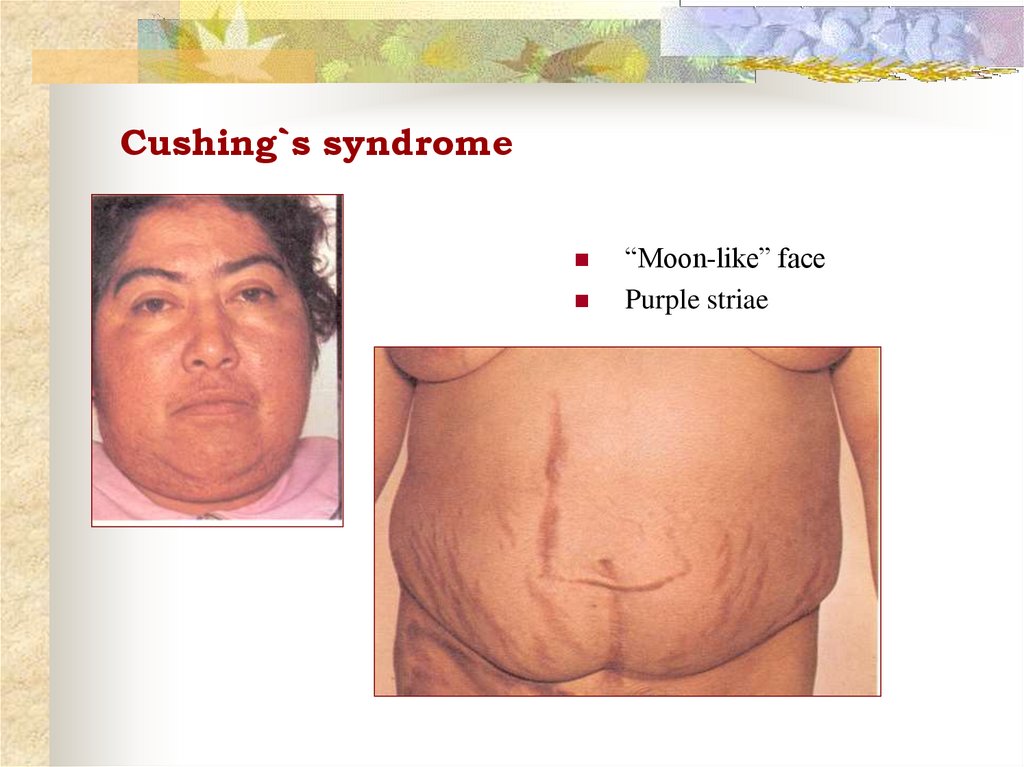
44. Cushing`s syndrome
“Moon-like” facePurple striae
45. Diagnostics and treatment of Cushing`s disease
Diagnosis:1.
ACTH and Cortisol level in the blood
2.
Visualization of the tumor: X-Ray tomography, CT of
the pituitary and adrenal glands
3.
Hyperglycemia, glucosuria
Treatment: microresection of the tumor, chemotherapy, if no
– metyrapone (inhibitor of synthesis)
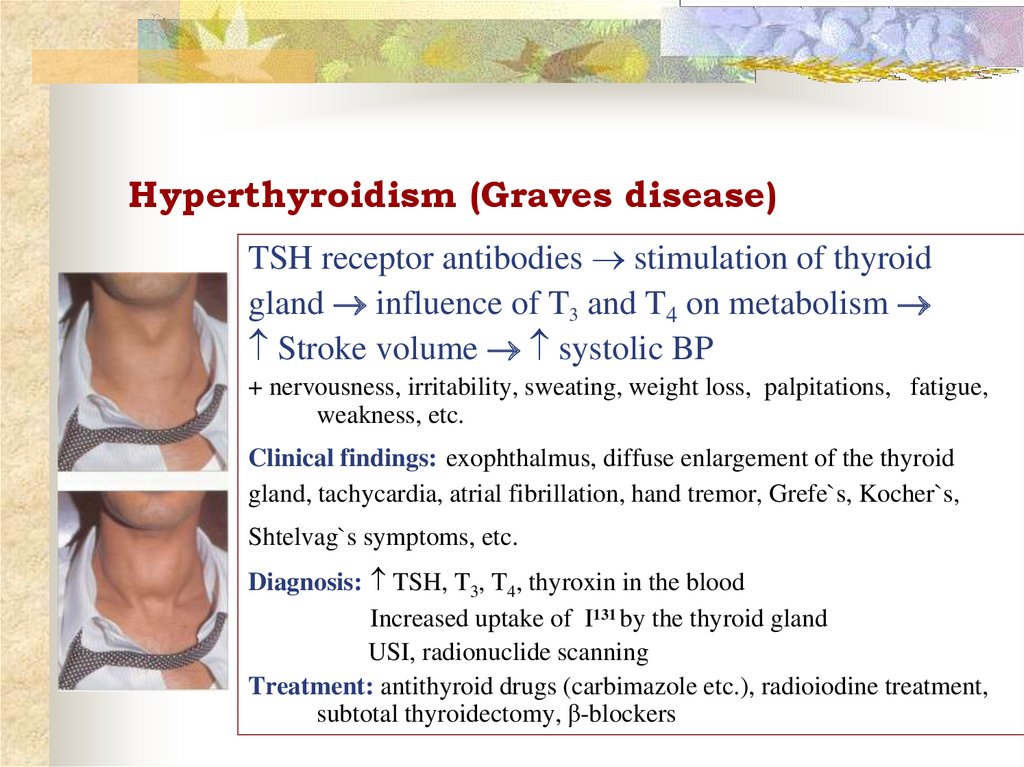
46. Hyperthyroidism (Graves disease)
TSH receptor antibodies stimulation of thyroidgland influence of T3 and T4 on metabolism
Stroke volume systolic BP
+ nervousness, irritability, sweating, weight loss, palpitations, fatigue,
weakness, etc.
Clinical findings: exophthalmus, diffuse enlargement of the thyroid
gland, tachycardia, atrial fibrillation, hand tremor, Grefe`s, Kocher`s,
Shtelvag`s symptoms, etc.
Diagnosis: TSH, T3, T4, thyroxin in the blood
Increased uptake of I131 by the thyroid gland
USI, radionuclide scanning
Treatment: antithyroid drugs (carbimazole etc.), radioiodine treatment,
subtotal thyroidectomy, β-blockers
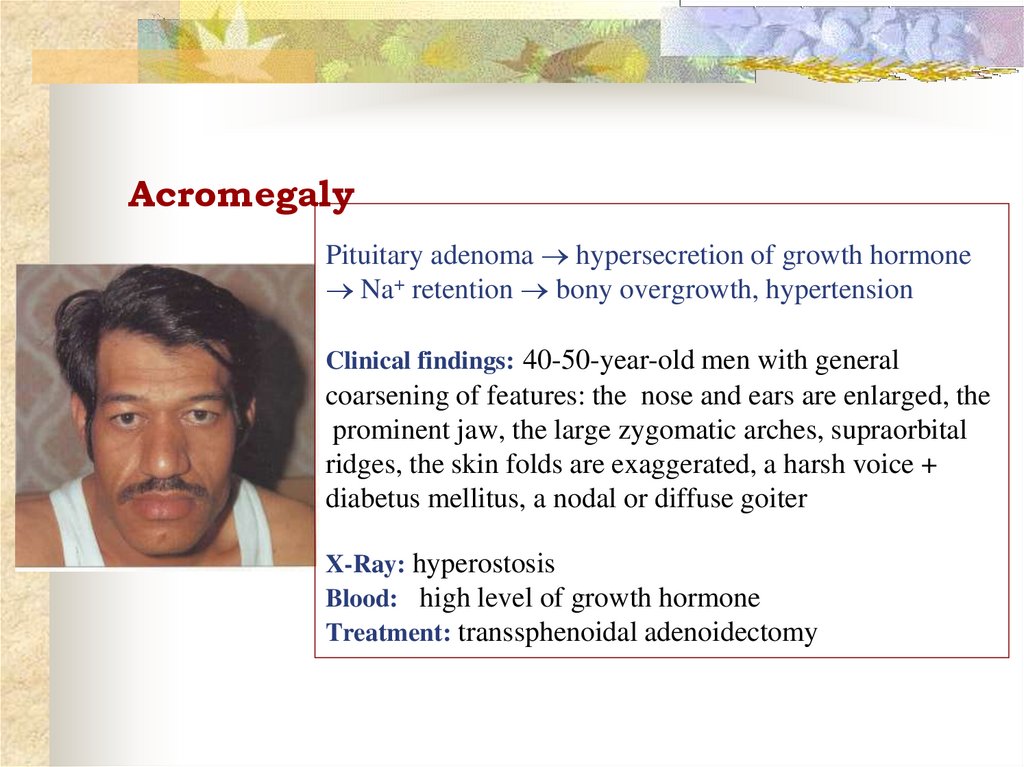
47. Acromegaly
Pituitary adenoma hypersecretion of growth hormoneNa+ retention bony overgrowth, hypertension
Clinical findings: 40-50-year-old men with general
coarsening of features: the nose and ears are enlarged, the
prominent jaw, the large zygomatic arches, supraorbital
ridges, the skin folds are exaggerated, a harsh voice +
diabetus mellitus, a nodal or diffuse goiter
X-Ray: hyperostosis
Blood: high level of growth hormone
Treatment: transsphenoidal adenoidectomy
48. Cardiovascular (hemodynamic) AH:
1. Atherosclerosis of the aorta ( regidity of aorta)- elderly and senile age
- systolic AH (BP=180/80 mmHg)
- systolic murmur (aortic stenosis)
- signs of a general atherosclerosis: X-Ray, angiography, Echocardiography,
MRI
2. Aortic insufficiency (rheumatism, infective endocarditis, syphiis):
- dizziness, syncope, heart pains
- BP=140/10 mmHg
- rough diastolic murmur over the 2nd intercostal space on the right
- Echo-, Doppler echocardiography
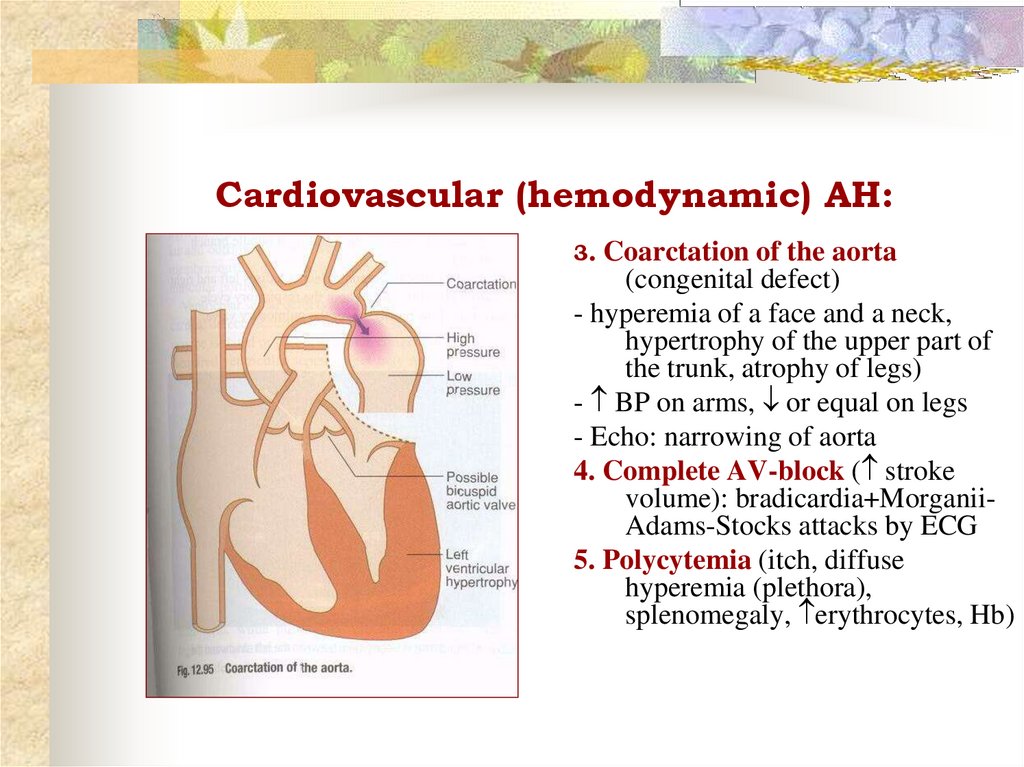
49. Cardiovascular (hemodynamic) AH:
3.Coarctation of the aorta
(congenital defect)
- hyperemia of a face and a neck,
hypertrophy of the upper part of
the trunk, atrophy of legs)
- BP on arms, or equal on legs
- Echo: narrowing of aorta
4. Complete AV-block ( stroke
volume): bradicardia+MorganiiAdams-Stocks attacks by ECG
5. Polycytemia (itch, diffuse
hyperemia (plethora),
splenomegaly, erythrocytes, Hb)
50. Neurogenic AH
Traumas of a skull,meningitis, encephalitis,
cerebral atherosclerosis,
tumors
Severe headaches, dizziness,
epilepsy
Signs of organic injuries of
CNS, mental disorders
Ophtalmoscopy,
X-Ray of a skull, EEG, CT, MRA