Similar presentations:
Personality Disorders
1.
Personality Disorders2.
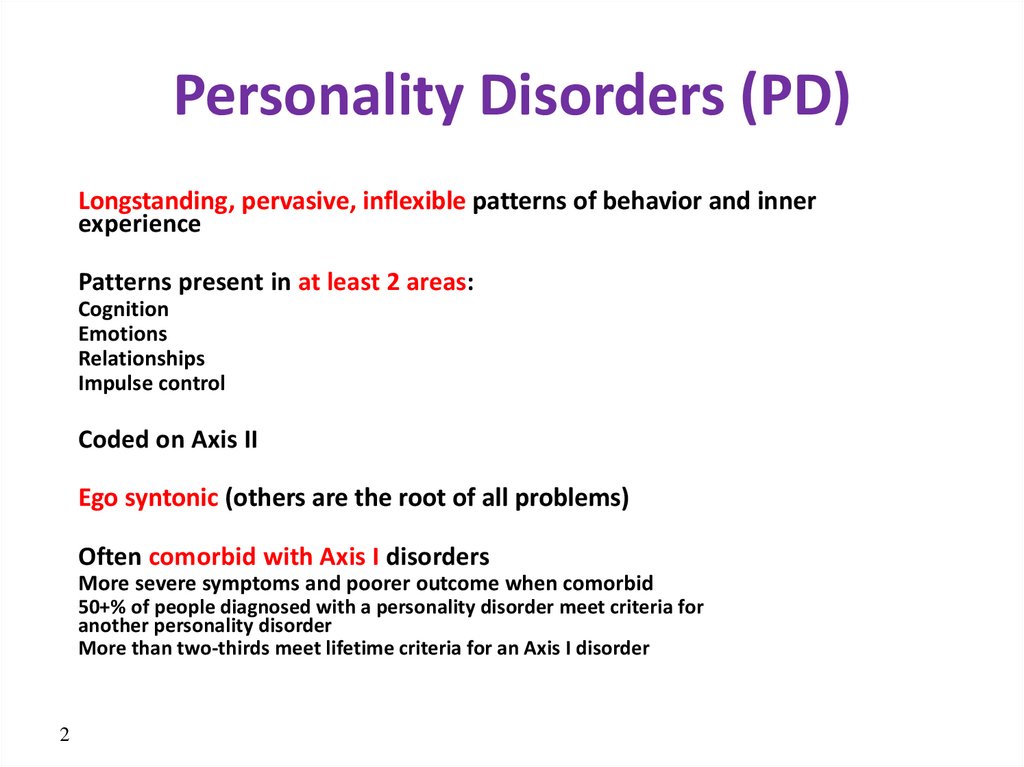
Personality Disorders (PD)Longstanding, pervasive, inflexible patterns of behavior and inner
experience
Patterns present in at least 2 areas:
Cognition
Emotions
Relationships
Impulse control
Coded on Axis II
Ego syntonic (others are the root of all problems)
Often comorbid with Axis I disorders
More severe symptoms and poorer outcome when comorbid
50+% of people diagnosed with a personality disorder meet criteria for
another personality disorder
More than two-thirds meet lifetime criteria for an Axis I disorder
2
3.
What is a personality??A generally consistent (but personal) style of
interacting with the world and other people
Our ‘character’ is reflected in how we think, what and
who we like, and how we respond to life
It is generally stable over time allows some
predictability
No trait or style is automatically indicative of disorder
or disease (don’t confuse eccentricity with disorder)
4.
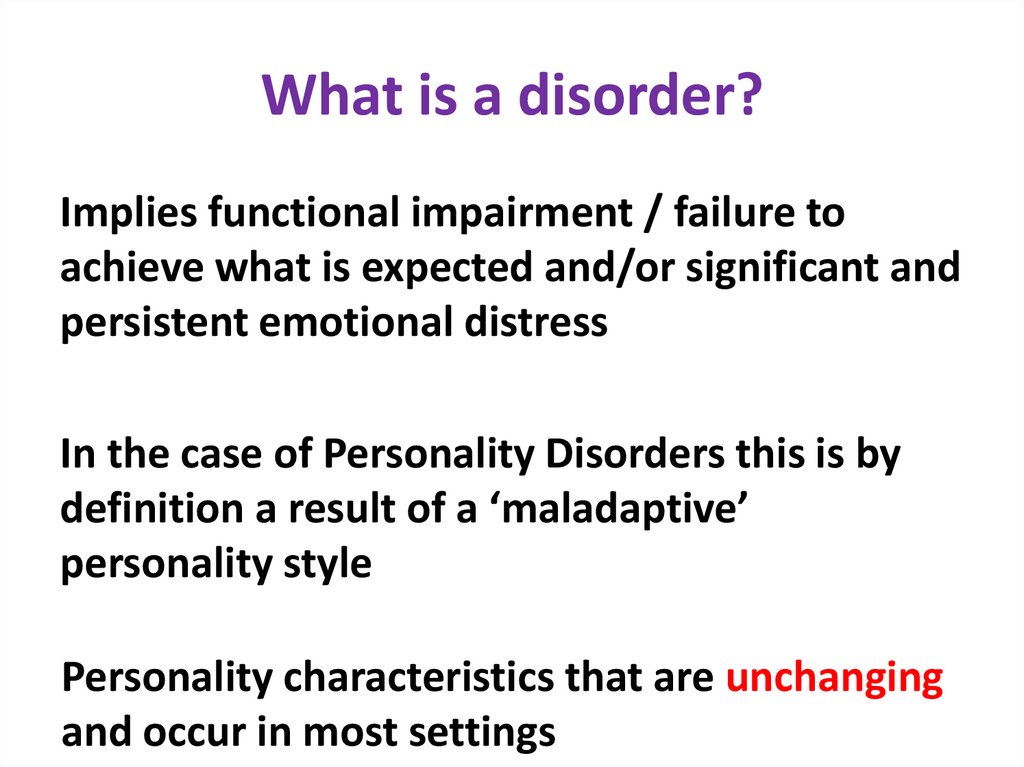
What is a disorder?Implies functional impairment / failure to
achieve what is expected and/or significant and
persistent emotional distress
In the case of Personality Disorders this is by
definition a result of a ‘maladaptive’
personality style
Personality characteristics that are unchanging
and occur in most settings
5.
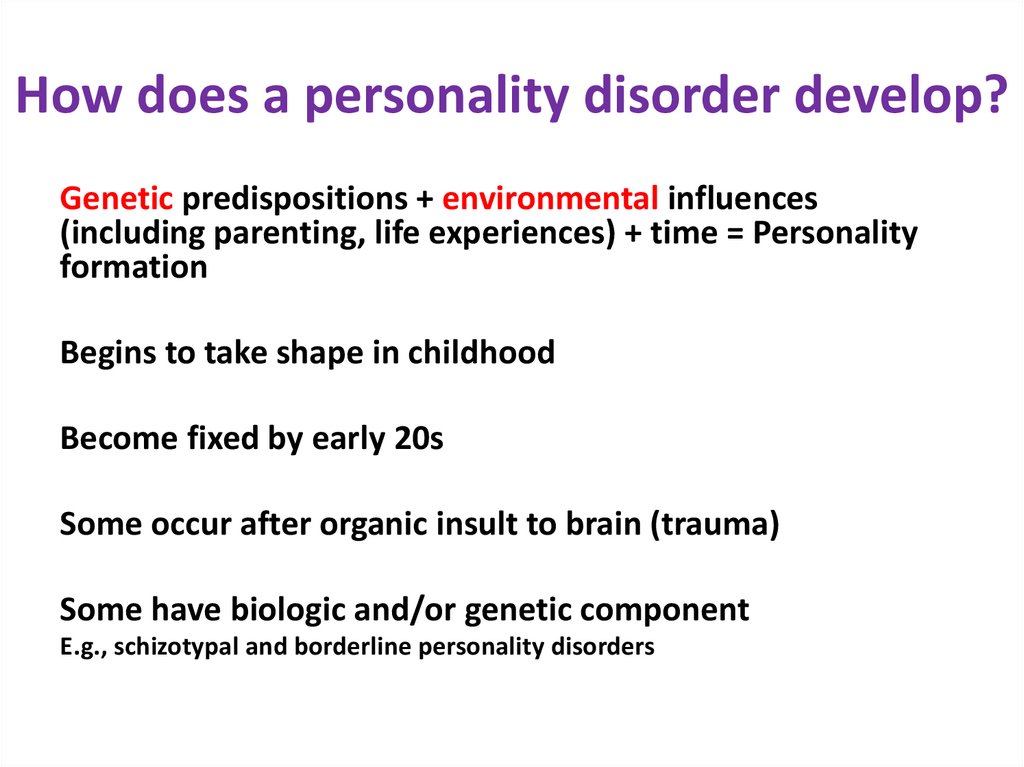
How does a personality disorder develop?Genetic predispositions + environmental influences
(including parenting, life experiences) + time = Personality
formation
Begins to take shape in childhood
Become fixed by early 20s
Some occur after organic insult to brain (trauma)
Some have biologic and/or genetic component
E.g., schizotypal and borderline personality disorders
6.
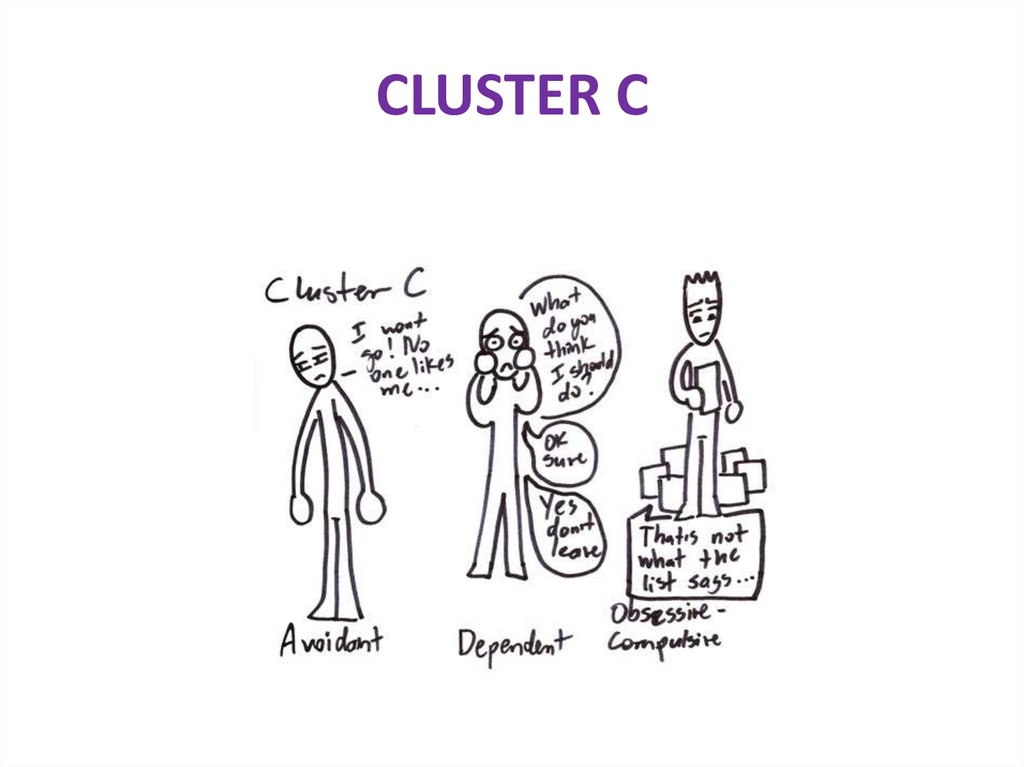
Classifying Personality DisordersClassifies in 3 clusters:
Cluster A Odd/Eccentric
Cluster B Dramatic/Erratic
Cluster C Anxious/Fearful
Gender bias
Certain diagnoses applied more often to men, others to
women
6
7.
Classification of Personality DisordersCluster A: Odd/Eccentric
Schizotypal Personality Disorder
Schizoid Personality Disorder
Paranoid Personality Disorder
Cluster B: Dramatic/Erratic
Histrionic Personality Disorder
Narcissistic Personality Disorder
Borderline Personality Disorder
AntiSocial Personality Disorder
Cluster C: Anxious/Fearful
Avoidant Personality Disorder
Dependent Personality Disorder
Obsessive-Compulsive Personality Disorder
8.
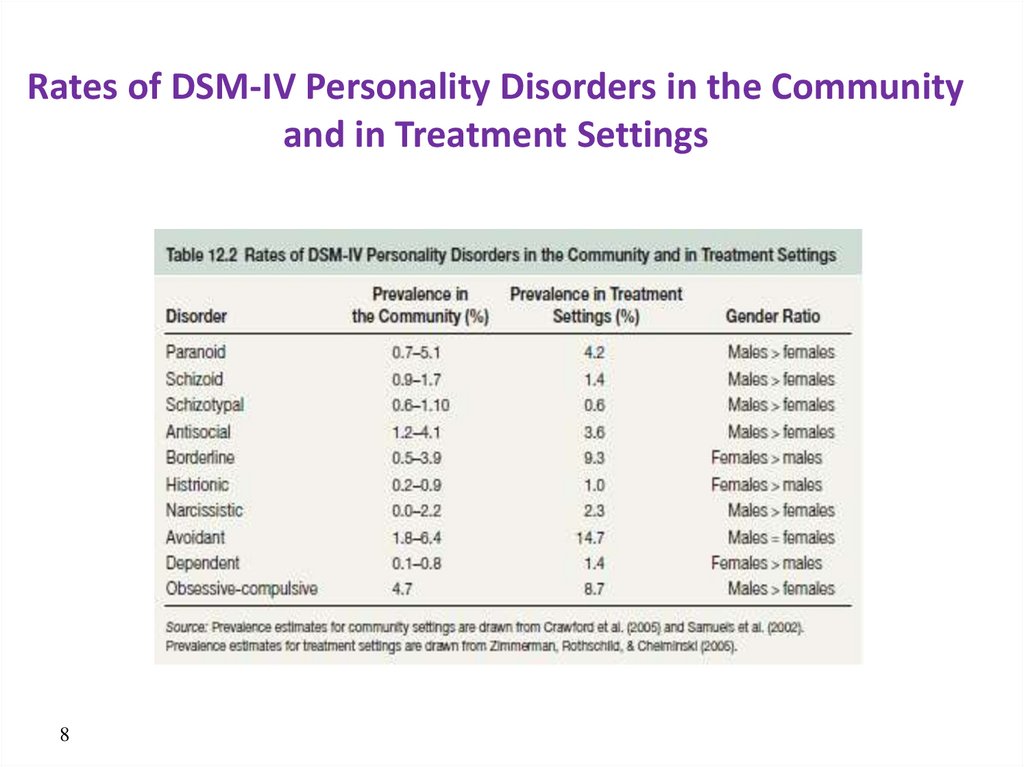
Rates of DSM-IV Personality Disorders in the Communityand in Treatment Settings
8
9.
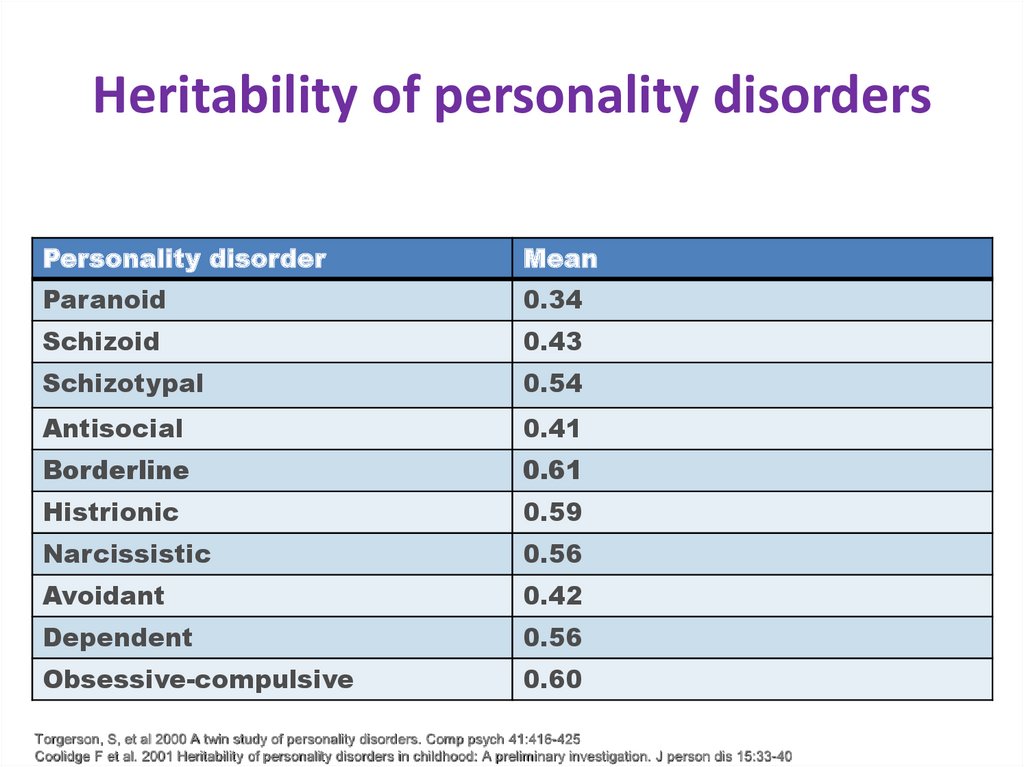
Heritability of personality disordersPersonality disorder
Mean
Paranoid
0.34
Schizoid
0.43
Schizotypal
0.54
Antisocial
0.41
Borderline
0.61
Histrionic
0.59
Narcissistic
0.56
Avoidant
0.42
Dependent
0.56
Obsessive-compulsive
0.60
Torgerson, S, et al 2000 A twin study of personality disorders. Comp psych 41:416-425
Coolidge F et al. 2001 Heritability of personality disorders in childhood: A preliminary investigation. J person dis 15:33-40
10.
CLUSTER A11.
Paranoid Personality DisorderA. pervasive pattern of distrust and suspiciousness of other such that their motives are
interpreted as malevolent beginning in early adulthood and indicated by four or more of the following:
-suspects, without sufficient basis, others are exploiting, deceiving, or harming him
-preoccupied with unjust doubts about loyalty of friends or associates
-won’t confide in others lest info be used against him
-reads hidden demeaning or threatening meanings into benign remarks or events
-bears a grudge, is unforgiving of slights
-perceives attacks on his character that others don’t and is quick to counterattack
-recurrent suspicions about fidelity of spouse or sexual partner
B. Does not occur exclusively within schizophrenia
12.
Characteristics of ParanoidPersonality Disorder
Aloof, emotionally cold
Unjustified suspiciousness, hostility
Hypersensitivity to slights, jealousy
Blames others when things go wrong
Rigid, unforgiving, sarcastic, litigious
No hallucinations or full blown delusions
Prevalence: 1-2%; M>F
Cormorbidity high for
Schizotypal
Borderline
Avoidant
Therapy, including meds, of little value – trusting relationship is key but hard to come
by b/o ‘self-fulfilling prophecy’
13.
Treatment of Paranoid Personality DisorderMedications
Pimozide (very selective, postsynaptic antidopaminergic agent used in
treating delusions
Effective in treating blaming, low tolerance for frustration,
hypersensitivity to criticism
Fluoxetine (effective in reducing suspiciousness)
CBT
Cognitive restructuring (for hypervigilance)
Relaxation training
Note: no longer considered an “untreatable” disorder
14.
Case 1- Paranoid Personality Disorder• U. is 40 y/o male. Recently divorced. Furiously hateful of his exwife, sure that she’d cheated on him. Although he was unable to
procure any proof of her cheating- he still believes in it. The exwife claims that she left U. because he has always been
emotionally cold, aloof, never supported her, always blaming her,
but U. keeps blaming her solely for the divorce, thinks that he’s
been a perfect husband while his ex has been a lying monster and
a cheater. Also, he distrusts his boss, always questions his secret
agenda, and is planning to sue him for disregarding the workers’
rights. U. always writes complaint letters to authorities, has sued
different authorities several times, he has only one close friend
and doesn’t fully trust this friend either. He looks quiet and
reserved to others, has little interest in other’s activities and
blames other people for his problems.
15.
Schizoid Personality DisorderA. Pervasive pattern of detachment from social relationships and restricted range of
emotions in interpersonal settings beginning in early adulthood and indicated by 4 or more:
-Almost always chooses solitary activities
-Has little interest in sex
-Takes pleasure in few if any, activities
-Lacks close friends or confidants (other than family)
-Appears indifferent to praise or criticism
-Neither desires nor enjoys close relationships, including family
-Shows emotional coldness, detachment, or flattened affect
B. Does not occur exclusively within schizophrenia
16.
Characteristics of SchizoidPersonality Disorder
Can perform well in solitary activities (computers, night watchman)
Limited emotional range, detached, daydream a lot
Experiences anhedonia
NO increased risk for schizophrenia but many may actually suffer from autismspectrum disease
Comorbidity high for
Schizotypal
Avoidant
Paranoid
“Loners” not necessarily schizoid, unless functioning impaired (traits vs
disorder)
Treatment of little help
Prevalence 2%; M>F
17.
Treatment for Schizoid Personality DisorderSSRIs
Fluoxetine
Behavioral
Social skills training
Group therapy
High dropout rate
18.
Case 2- Schizoid Personality Disorder• A. is a 50 y/o male. Never married. Works as a
night shift guard. Has no friends. Has never been
in a relationship and tells people he is not
interested in relationships because they are
“messy”, and that he doesn’t desire sex, so “why
bother?”. In his free time he likes walking alone
in the forest. He visits his elderly parents once in
a few months, and talks to his sister on the
phone 2 times a year. He states that he loves his
family but isn’t interested in people outside the
family. He has 8 cats and has recently adopted a
dog.
19.
Schizotypal Personality DisorderA. Pervasive pattern of social and interpersonal deficits, reduced capacity for close relationships, cognitive or
perceptual distortions, eccentric behavior beginning and early adulthood indicated by 5 or more of the following:
-Ideas of reference
-Odd beliefs or magical thinking
-Unusual perceptual experiences
– Superstitious
Telepathic
Illusions
Feels the presence of a force or person not actually present.
-Vague, metaphorical or stereotyped speech
-Suspiciousness or paranoid ideation
-Inappropriate or constricted affect
Odd/eccentric behavior or appearance
– Wears strange clothes
– Talks to self
-Lack of close friends or confidants
-Excessive social anxiety that does not diminish with familiarity
B. Does not occur exclusively during the course of schizophrenia
20.
SchizotypesFirst degree relatives of schizophrenics
– Often characterized by “negative” criteria (odd speech,
inappropriate affect social anxiety)
Individuals who meet criteria for Schizotypal PD
– Most often characterized by perceptual aberrations, magical
ideation, and paranoid thinking
fragile X syndrome in women
– 3% incidence; M=F
21.
Etiology and Treatment• Etiology
– Similar to that of schizophrenia
– Genetic predisposition
– Children of mothers who had flu during 2nd trimester had higher schizotypy
scores (Venables, 1996)
– May be related to dysregulation of dopamine and other amines
– Individuals with schizotypal PD show structural brain findings similar to
those found in schizophrenia:
Cognitive and neuropsychological deficits
Enlarged ventricles
Less temporal gray matter
• Treatment
– Drugs proven more effective than psychotherapies
– Low-dose antipsychotics
22.
Case 3- Schizotypal PersonalityDisorder
• L. is a 21 y/o female. She earns her money by
working as a medium and predicting future with
Tarot. She wears odd colorful clothes that she
makes herself. She has very few friends and
states that she also has several invisible friends
from other dimensions, whose presence she can
feel always and who protect her. Her speech is
odd and difficult to understand. She giggles
inappropriately in social situations. Her brother
has been recently diagnosed with Schizophrenia.
23.
CLUSTER B24.
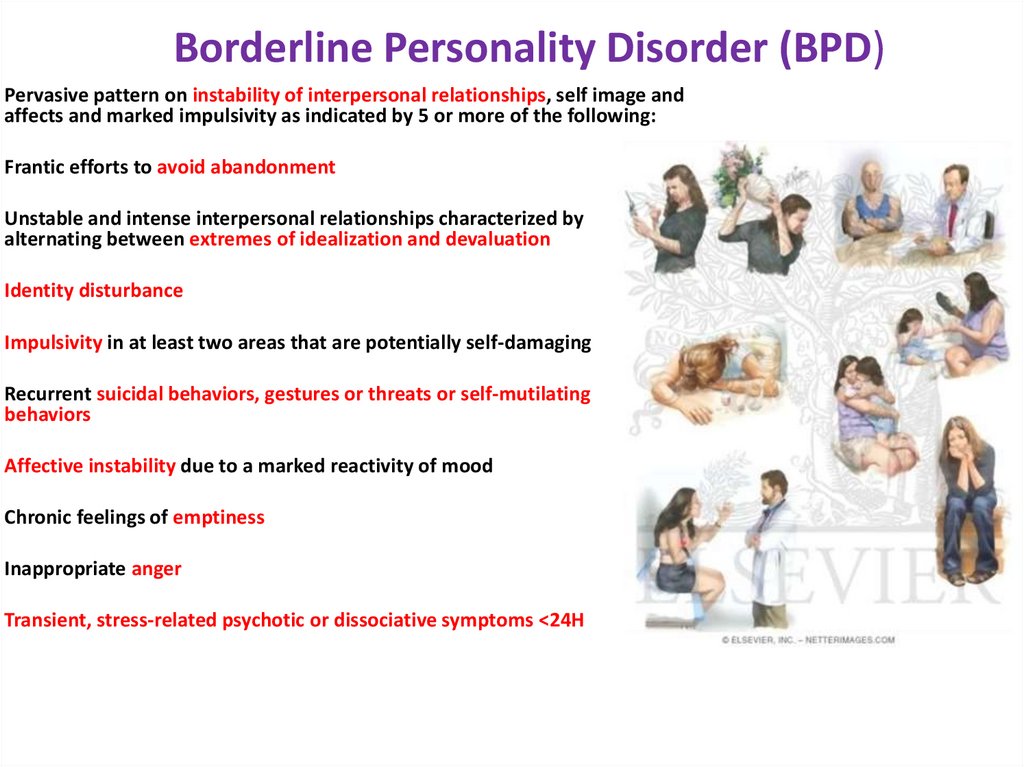
Borderline Personality Disorder (BPD)Pervasive pattern on instability of interpersonal relationships, self image and
affects and marked impulsivity as indicated by 5 or more of the following:
Frantic efforts to avoid abandonment
Unstable and intense interpersonal relationships characterized by
alternating between extremes of idealization and devaluation
Identity disturbance
Impulsivity in at least two areas that are potentially self-damaging
Recurrent suicidal behaviors, gestures or threats or self-mutilating
behaviors
Affective instability due to a marked reactivity of mood
Chronic feelings of emptiness
Inappropriate anger
Transient, stress-related psychotic or dissociative symptoms <24H
25.
Borderline Personality Disorder (BPD)Onset during adolescence or early adulthood
Prognosis poor within 10 years of diagnosis
Later in life, most no longer meet diagnostic criteria (Paris, 2002)
“Borderline Burnout”
Comorbidity high with PTSD= complex PTSD, MDD,
substance-related, and eating disorders
Comorbidity predicts symptoms 6 years later
Suicide rates high, Self-mutilation also a problem
25
26.
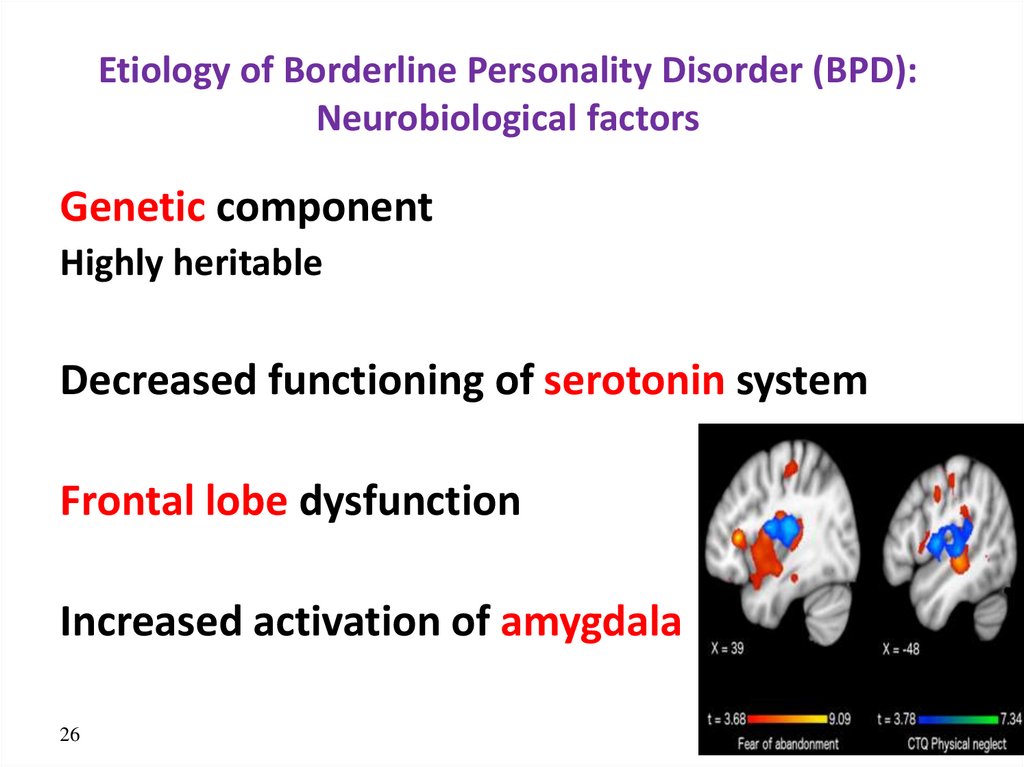
Etiology of Borderline Personality Disorder (BPD):Neurobiological factors
Genetic component
Highly heritable
Decreased functioning of serotonin system
Frontal lobe dysfunction
Increased activation of amygdala
26
27.
Etiology of Borderline Personality Disorder (BPD):Social Environmental Factors
• Parental separation
• Verbal, physical, sexual and emotional abuse
during childhood
27
28.
Borderline PD: Management• Beware of idealization, be realistic about
treatment targets as well as risks and side effects
• Treat presenting pathology
• BUT: Know what you are dealing with, avoid “red
herrings” eg. “depression” “voices in the head”
• Be honest, consistent and non-judgmental
29.
Borderline PD: TreatmentPsychotherapy (Mainstay) :
DBT : suicide and affective dysregulation
Transference-based psychotherapy
Mentalization-based psychotherapy
Schema-focussed therapy
General Principles
Focus on patient-therapist relationship in the “here and now”
Educate patients to recognise their affective reactions and what
triggers them
30.
Borderline PD: TreatmentPharmacotherapy (adjunct)
Cochrane Review (2010):SSRI’s not recommended for as first
choice for affective dysregulation & impulsivity, nor low
dose antipsychotics for cognitive-perceptual symptoms
SSRI only for MDD
Affective dysregulation: topiramate, valproate, lamotrigine,
aripiprazole, olanzapine & haloperidol
Impulsive-behavioural: lamotrigine & topiramate, omega-3
fats, flupenthixol; aripiprazole
Cognitive-perceptual: olanzapine, aripiprazole
Self mutilation and suicidal behaviour: none. Olanzapine
unfavourable effect
31.
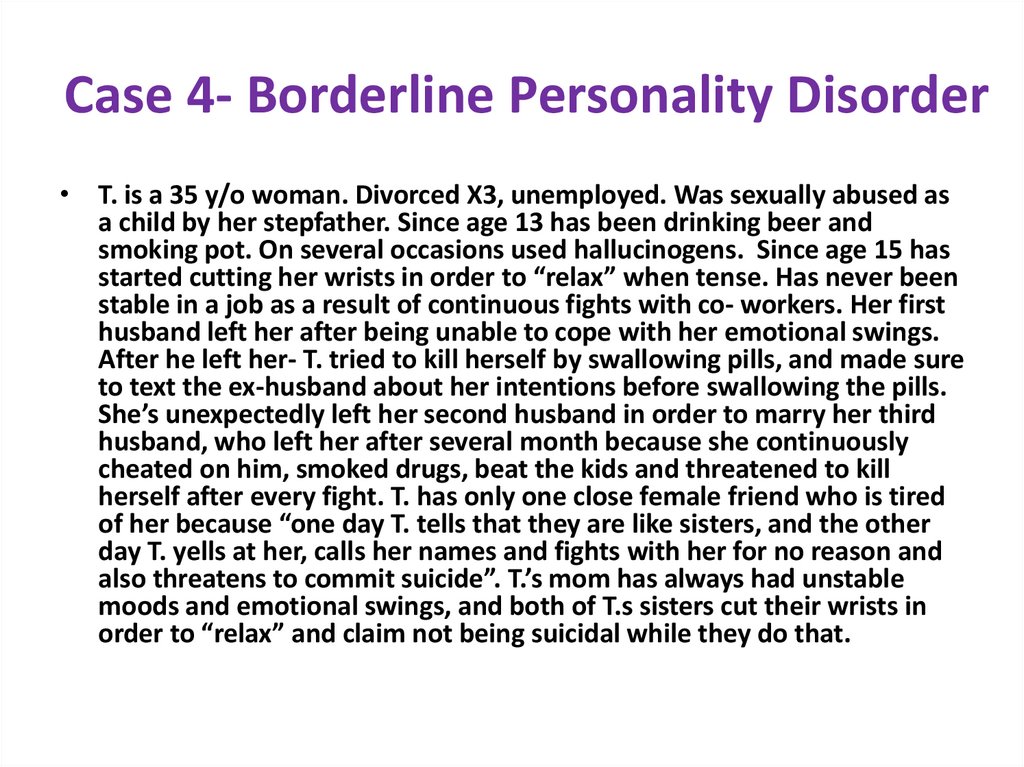
Case 4- Borderline Personality Disorder• T. is a 35 y/o woman. Divorced X3, unemployed. Was sexually abused as
a child by her stepfather. Since age 13 has been drinking beer and
smoking pot. On several occasions used hallucinogens. Since age 15 has
started cutting her wrists in order to “relax” when tense. Has never been
stable in a job as a result of continuous fights with co- workers. Her first
husband left her after being unable to cope with her emotional swings.
After he left her- T. tried to kill herself by swallowing pills, and made sure
to text the ex-husband about her intentions before swallowing the pills.
She’s unexpectedly left her second husband in order to marry her third
husband, who left her after several month because she continuously
cheated on him, smoked drugs, beat the kids and threatened to kill
herself after every fight. T. has only one close female friend who is tired
of her because “one day T. tells that they are like sisters, and the other
day T. yells at her, calls her names and fights with her for no reason and
also threatens to commit suicide”. T.’s mom has always had unstable
moods and emotional swings, and both of T.s sisters cut their wrists in
order to “relax” and claim not being suicidal while they do that.
32.
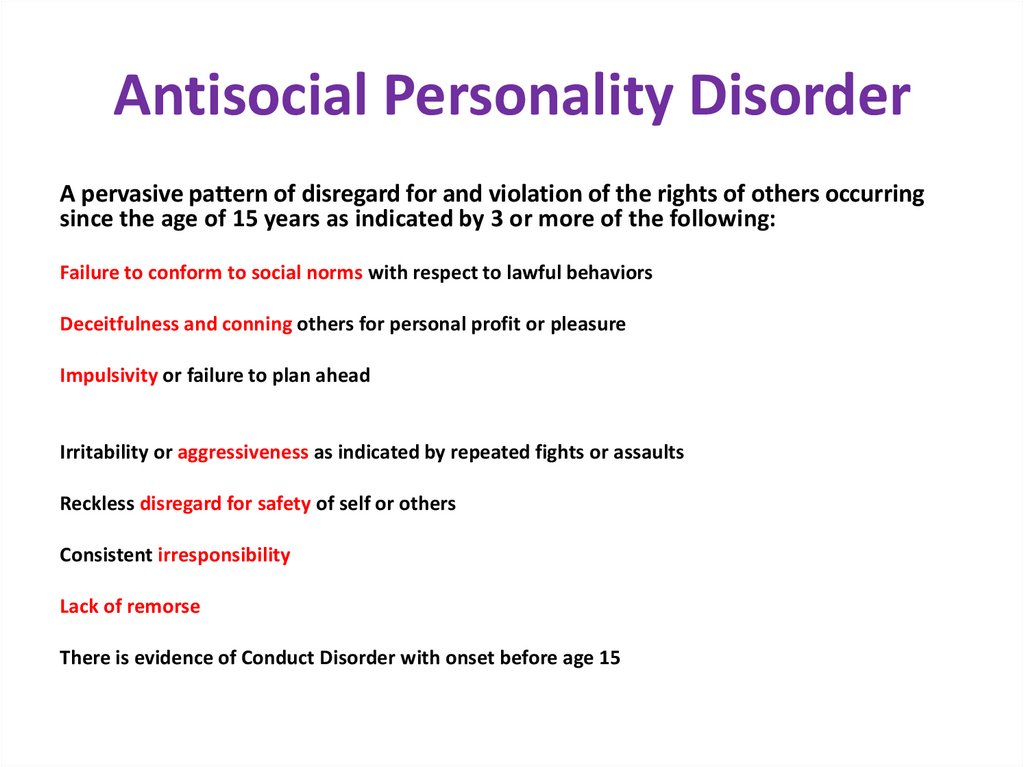
Antisocial Personality DisorderA pervasive pattern of disregard for and violation of the rights of others occurring
since the age of 15 years as indicated by 3 or more of the following:
Failure to conform to social norms with respect to lawful behaviors
Deceitfulness and conning others for personal profit or pleasure
Impulsivity or failure to plan ahead
Irritability or aggressiveness as indicated by repeated fights or assaults
Reckless disregard for safety of self or others
Consistent irresponsibility
Lack of remorse
There is evidence of Conduct Disorder with onset before age 15
33.
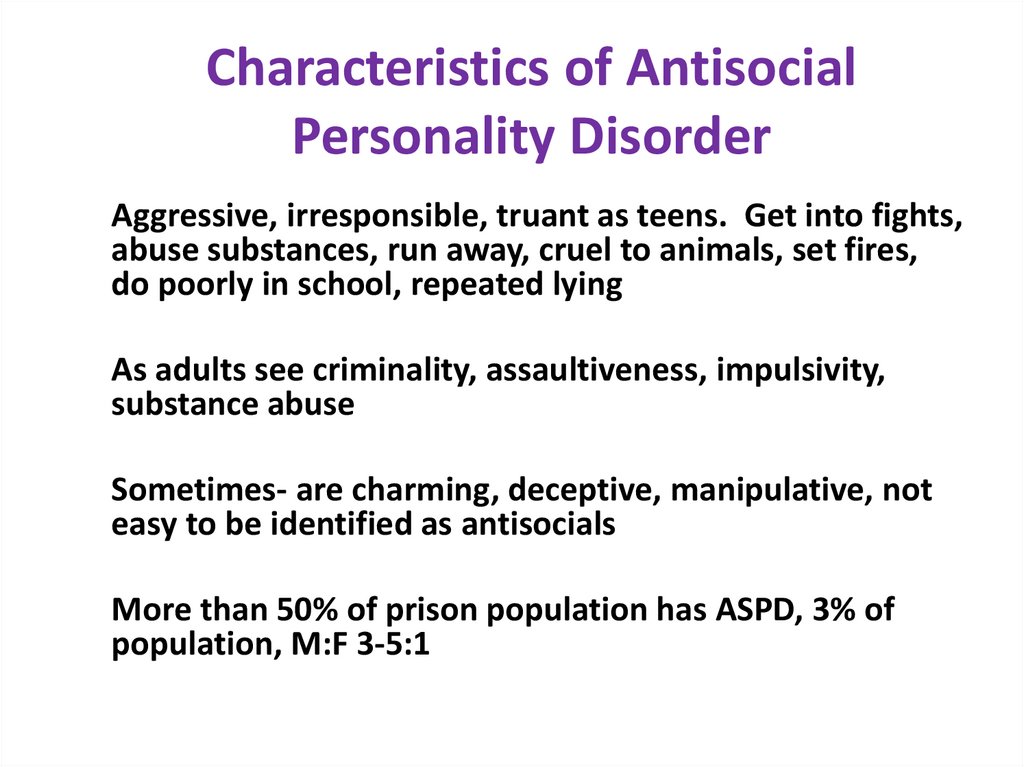
Characteristics of AntisocialPersonality Disorder
Aggressive, irresponsible, truant as teens. Get into fights,
abuse substances, run away, cruel to animals, set fires,
do poorly in school, repeated lying
As adults see criminality, assaultiveness, impulsivity,
substance abuse
Sometimes- are charming, deceptive, manipulative, not
easy to be identified as antisocials
More than 50% of prison population has ASPD, 3% of
population, M:F 3-5:1
34.
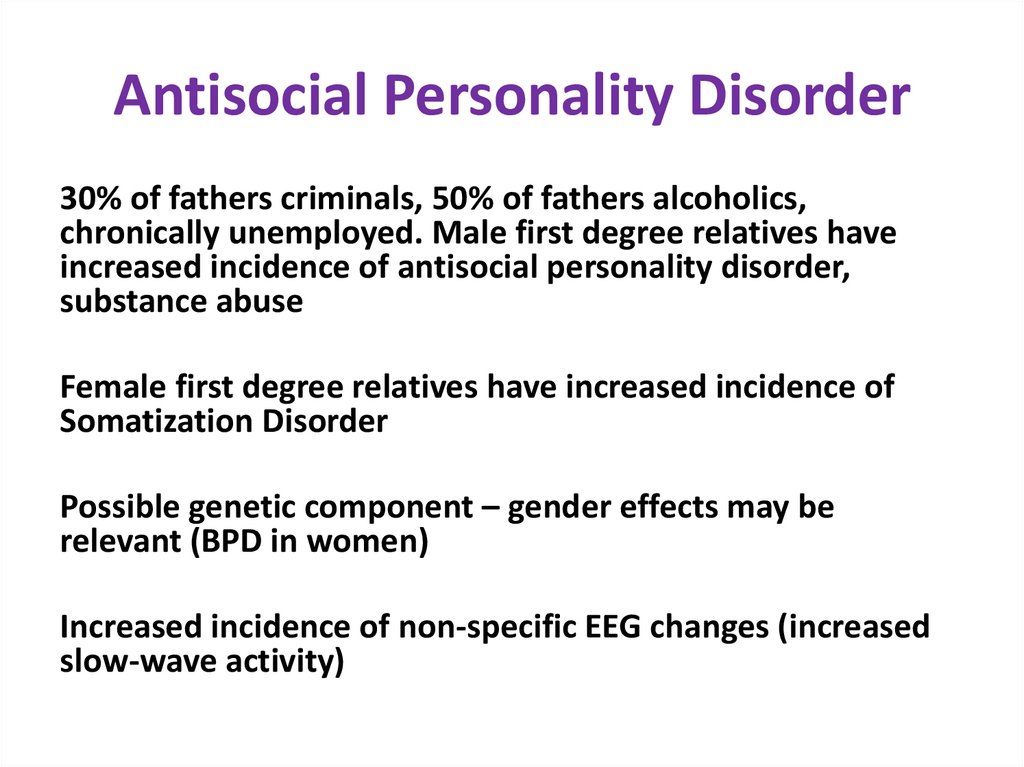
Antisocial Personality Disorder30% of fathers criminals, 50% of fathers alcoholics,
chronically unemployed. Male first degree relatives have
increased incidence of antisocial personality disorder,
substance abuse
Female first degree relatives have increased incidence of
Somatization Disorder
Possible genetic component – gender effects may be
relevant (BPD in women)
Increased incidence of non-specific EEG changes (increased
slow-wave activity)
35.
Antisocial Personality Disorder• Substance abuse most common
comorbid disorder
• More common among lower SES
groups
• More than 50% of prison population
has ASPD, 3% of population, M:F 3-5:1
35
36.
Etiology of Antisocial Personality Disorder• Genetics
– Antisocial behavior heritable
• Estimates as high as .96
– Genetic risk for APD, psychopathy,
conduct disorder, and substance
abuse related.
• Family environment
– Lack of warmth, negativity, and
parental inconsistency predict APD
– Poverty, exposure to violence
– Family environment interacts with
genetics
36
37.
Case 5- Anticosial Personality Disorder A• N. is 20 y/o man. He is currently in prison for
robbery. This is his fifth imprisonment. He
explains that he prefers robbing to holding a job,
and feels absolutely no remorse. His father was
an alcoholic and drug addict and has been
executed for double murder. N. himself was a
“problematic child” who was truant from school,
picked fights, stole from shops, was cruel to
animals and started using marihuana since age
10. N. states that after serving his current
punishment he intends to continue his chosen
life path of a criminal because “he likes it”.
38.
Case 6- Antisocial Personality Disorder B• T. is a 41 y/o lady. She is a second wife of a famous gynecologist and a
mother to a 3 y/o girl, she is a president of a volunteer organization and
actively volunteers on many occasions. She is always charming, pleasant
and polite. One day, out of the blue, her husband discovers that T.
actually steals the donations to the organization she heads, that their
mutual daughter is actually not his but his brother’s, with whom T. has
been having an affair for several years, and that T. has several ID cards
and several passports, with different names and addresses. When the
husband confronts T. an all of these- she pulls a gun out of her purse and
coldly threatens to kill him, his parents and the child if he discloses the
truth to anyone. Terrified, the husband keeps silence, especially after T.
beats him with a chair. After a few months T. disappears, leaving the
daughter and taking all of the gynecologist’s money, and rumors tell
she’s run away abroad. The husband asks the police for help, but shortly
after that he gets arrested after T. files a false complaint that he sexually
abuses his patients.
39.
Histrionic Personality DisorderA pervasive pattern of excessive emotionality and attention seeking, beginning in early adulthood
and indicated by 5 or more:
Uncomfortable in situations where not the center of attention
Interaction with others is often characterized by inappropriate sexual behavior
Rapidly shifting and shallow expression of emotions
Consistently uses physical appearance to draw attention to self
Style of speech that is impressionistic and lacking in detail
Shows self-dramatization, theatricality, and exaggerated emotion
Is suggestible and easily influenced by others or circumstances
Considers relationships to be more intimate than they actually are
40.
Etiology/Treatment ofHistrionic Personality Disorder
Etiology
• Unknown but may include
– Genetic contribution
– Childhood incidents
– May be associated with low self-esteem
Treatment
• Usually present for treatment due to depression
• Sertraline (for impulsivity and depression symptoms)
41.
Case 7- Histrionic Personality Disorder• L. is a 37 y/o actress. She always wears tons of
makeup and short colorful dresses. Every person
she meets immediately becomes an object of
her attention and is proclaimed to be her new
best friend, she tells everyone every single detail
of her life with great drama and exaggeration,
and if people refuse to listen to her- she bursts
into tears and hysterical sobbing, falls to ground
and becomes a subject of ridicule. She explains
that she doesn’t mind to be laughed at as long
as people pay attention to her.
42.
Narcissistic Personality DisorderA pervasive pattern of grandiosity, need for admiration, and lack of empathy, beginning
in early adulthood and indicated by 5 or more of the following:
– Grandiose sense of self-importance
– Preoccupied with fantasies of success, power, beauty, or ideal love
– Believes he is “special” and should only affiliate with high-status people or things
– Requires excessive admiration
– Has sense of entitlement
– Is interpersonally exploitive (takes advantage of others)
– Lacks empathy
– Is often envious of others and believes others are envious of him
– Shows arrogant, haughty behaviors or attitudes
43.
Characteristics of NarcissisticPersonality Disorder
• <1% of general population; M>F
• Become enraged at criticism
• Fragile self-esteem, prone to depression
• Their behavior produces interpersonal difficulties, rejection, loss,
occupational problems, which they can’t handle
• Chronic, difficult to treat
• Aging is handled poorly
• Treatment: psychotherapy; poor prognosis
44.
Treatment for Narcissistic PD• SSRIs for depression
•CBT
• cognitive restructuring (for ego concerns)
45.
Case 8- Narcissistic PersonalityDisorder
• A .is a 57 y/o surgeon. He has a successful private
practice, owns a yacht and wears very expensive
clothes a an exclusive wrist watch. His friends are
famous doctors like himself, businessmen, politicians.
He treats his coworkers with disregard, openly claims
that he’s is better than anyone else in every single
aspect, is cruel to interns and residents and is
perceived as an arrogant person. Lately he’s noticed
that his hair is turning grey and that that he’s gained a
little weight, and since that has become moody and
continuously broods over getting old.
46.
CLUSTER C47.
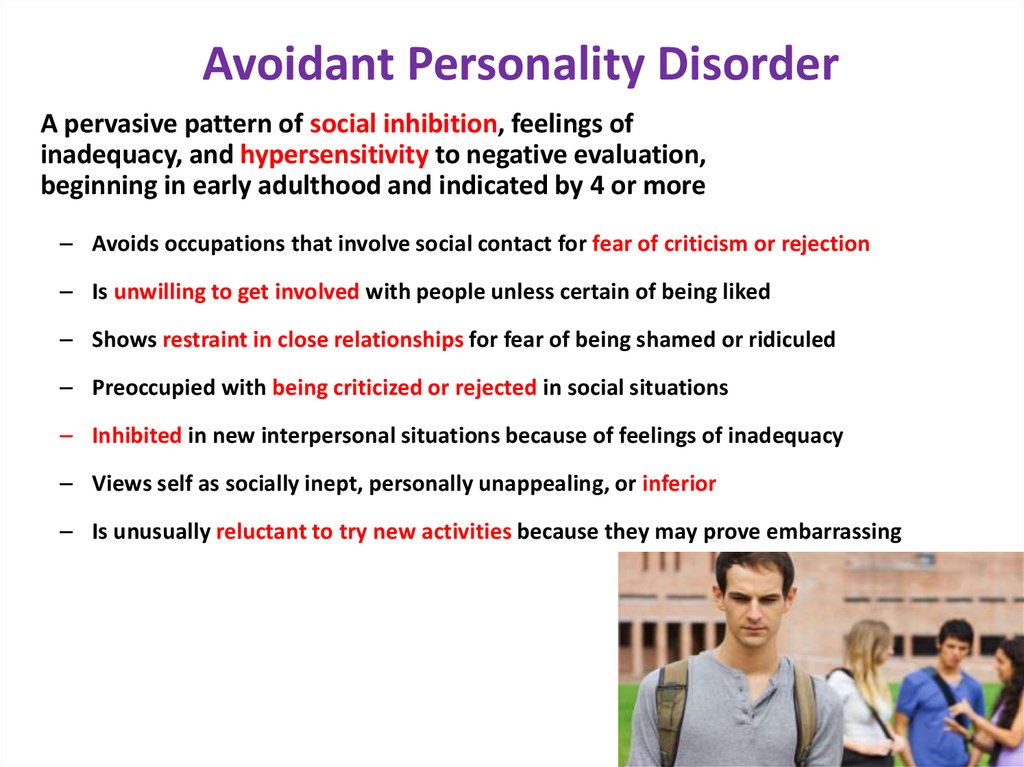
Avoidant Personality DisorderA pervasive pattern of social inhibition, feelings of
inadequacy, and hypersensitivity to negative evaluation,
beginning in early adulthood and indicated by 4 or more
– Avoids occupations that involve social contact for fear of criticism or rejection
– Is unwilling to get involved with people unless certain of being liked
– Shows restraint in close relationships for fear of being shamed or ridiculed
– Preoccupied with being criticized or rejected in social situations
– Inhibited in new interpersonal situations because of feelings of inadequacy
– Views self as socially inept, personally unappealing, or inferior
– Is unusually reluctant to try new activities because they may prove embarrassing
48.
Characteristics of AvoidantPersonality Disorder
• They have “an inferiority complex”
• 0.5-1.0%; M=F
• Often take jobs “on the sidelines,” shy and eager to please
• Subject to depression, anxiety, anger, phobic avoidance
• Unlike schizoid, long for relationships
• Treatment: Group or individual psychotherapy, SSRIs
• Diagnosis overlaps greatly with Social Phobia
49.
Treatment of Avoidant Personality Disorder• SSRIs
• CBT
– Graduated exposure
– Social skills training
– Systematic desensitization
– CBT has been found effective in changing
behavior but does not improve loneliness
50.
Case 9- Avoidant Personality Disorder• S. is a 19 y/o male student. He is always shy,
turns red in social settings, always alone in the
university. When asked why he doesn’t socializelooks sad and explains that he wants to make
friends so badly, but he’s sure that people will
reject him because he is a loser. He has been in
love with his neighbor for the past 4 years, but
has never even tried to talk to her and is not
sure she is aware of his existence. Every time he
meets the neighbor, he turns red and runs away.
51.
Dependent Personality DisorderA pervasive and excessive need to be taken care of that leads to submissive and clinging behavior and fears of separation,
beginning in early adulthood:
–
Difficulty making everyday decisions without excessive among of advice
–
Needs others to assume responsibility for most major areas of life
–
Has difficulty expressing disagreement because of fear of loss of approval
–
Has difficulty initiating projects or doing things on his own
–
Volunteers to do unpleasant tasks to obtain nurturance and support from others
–
Feels uncomfortable or helpless when alone
–
Urgently seeks new relationship as a source of care and support when one ends
–
Is unrealistically preoccupied with fears of being left alone to care
52.
Characteristics of DependentPersonality Disorder
• Persons with chronic physical illness in childhood may be
more prone to the disorder
• Lack of self confidence
• Excessive reliance on others
• Behavior focused on maintaining relationships
• May stay with an abusive, unfaithful or alcoholic partner
rather than face being alone
• Treatment: Psychotherapy, often successful
• Prevalence: very common; M=F
53.
TreatmentCBT
cognitive restructuring (for self-esteem concerns)
coping and social skills training
SSRIs
54.
Case 10- Dependent PersonalityDisorder
• M. is a 25 y/o woman. She is a housewife and fully
depends on her husband. She never leaves home without
her husband’s permission, and is always accompanied by
him. Her husband drinks alcohol and beats M. on a daily
basis. Once she was beaten so hard that she ended up
hospitalized for rib fractures. She told in the hospital that
“she’d fallen from stairs”, but no one believed and social
worker was invited to assess domestic violence. M.
admitted to the SW that her husband is violent, but
refused to leave him and go to an asylum because “I’m
not worth a lot without him”. When the SW suggested
calling the police- M. refused again and told her that “If
my husband goes to jail, I’ll be lost and no one will take
care of me.”
55.
Criteria for Obsessive-Compulsive PDA pervasive pattern of preoccupation with orderliness, perfectionism, and mental and interpersonal
control at the expense of flexibility, openness, and efficiency, beginning in early adulthood and indicated
by 4 or more:
– Preoccupied with details, rules, lists, order to the extent that the major point of an activity is lost
– Shows perfectionism that interferes with task completion
– Is excessively devoted to work to the exclusion of leisure activity and friendships
– Is overconscientious and scrupulous about matters of morality, ethics, and values
– Is unable to discard worn-out or worthless objects even with no sentimental value
– Is reluctant to delegate tasks or work with others unless they do it his way
– Adopts a miserly spending style toward self and others; hoards
– Shows rigidity and stubbornness
56.
Characteristics of CompulsivePersonality Disorder
Prevalence unknown, more common and in oldest children; M=F
Backgrounds: harsh discipline
Stiff, formal and rigid demeanor, constricted affect. Formal, serious, may lack a sense of humor
Indecisive b/c afraid of making a mistake, ruminate concerning decisions
Do well with routines and poorly with changes
Unable to compromise in interpersonal relationships
More likely to seek treatment than those with other personality disorders
Does not have the obsessions/compulsions of OCD
Most frequently comorbid with Avoidant PD
57.
TreatmentCBT
cognitive restructuring (for dichotomous thinking)
coping skills training
SSRIs
58.
Case 11- Obsessive- CompulsivePersonality Disorder
• D. is a 46 y/o male bank director. He is rigid,
perfectionist, hard working, detail- loving, extremely
efficient, he seldom allows his staff do important
things because he trusts only himself with these. He
spends long hours at work and has very little time for
his family. His wife complains that he’s never gone on
a vacation with his family, ever. While at home, he is
stubborn, criticizes his wife and kids, demands that
they keep order and keep up to his very high moral
standards, and also never throws away old clothes
and shoes because he “may need these one day”.
59.
Exercise• What are the personality disorders that are
Cluster A?
• paranoid personality disorder
schizoid personality disorder
schizotypal personality disorder
60.
Exercise• If you FEEL like you don't want to interact with a person, what
cluster are the probably categorized in?
• Cluster A
• What type of personality disorder is most likely to try to "test"
you?
• paranoid
• If a person has gone to see two or three doctors before they come
to see you, what type of Cluster A personality disorder might they
have?
• paranoid
• Is paranoid personality disorder more common in men or women?
• Men
61.
ExerciseWhat type of personality disorder tends to be aloof and unemotional?
schizoid
How will a schizoid personality disorder behave toward a physician?
will act uninterested
What type of personality disorder will have very limited emotional
response?
schizoid
What type of personality disorder will have no desire for sexual
relationships?
schizoid
Is schizoid or schizotypal personality disorder on the spectrum of
schizophrenia?
schizotypal
What type of personality disorder will often engage in erratic and odd
functions in speech or manner of dress?
schizotypal
What chromosomal abnormality is associated with schizotypal
personality disorder?
fragile X syndrome in women
62.
ExerciseWhich cluster is most commonly seen?
Cluster B
What are the Cluster B personality disorders?
antisocial personality disorder
histrionic personality disorder
borderline personality disorder
narcissistic personality disorder
What is the key component of human interaction with someone with antisocial personality disorder?
they LOVE to interact with people - motive is always for personal gain
What are the core behaviors of antisocial personality disorder?
deceit, impulsivity and manipulation
What two personality disorders go hand in hand but are commonly diagnosed based on gender?
antisocial = males
borderline = females
63.
Exercise• What type of personality disorder is satisfied through negative attention
(also positive)?
• histrionic
• What type of personality disorder depends on other people to tell them
how to feel, they lack an internalized sense of self worth?
• histrionic
• What type of personality disorder is emotionally shallow and lacks
intimacy?
• histrionic
64.
Exercise• What is the most studied personality disorder?
• borderline
• What type of personality disorder deeply fears rejection
and abandonment but will try to reject and destroy a
relationship?
• borderline
• What type of personality disorder is linked to substance
dependence and self- mutilation?
• borderline
65.
Exercise• What type of personality disorder react to criticism with
rage and stress?
• narcissistic
• What will make a narcissistic person envious?
• when they believe that someone is more special than they
are
• If you do not give someone with narcissistic personality
disorder attention, what will they think about you?
• think that you do not understand how special they are
• What is of utmost importance for someone with
narcissistic personality disorder?
• physical appearance
66.
ExerciseWhat type of personality disorder will tend to be a perfectionist?
obsessive compulsive personality disorder
Is O/C personality disorder more common in men or women?
men
What type of personality disorder will expect perfect care from a
practitioner?
OCPD
What type of personality disorder is characterized by excessive
need for caring and nurturing?
dependent
How does someone with dependent personality disorder make
decisions?
they don’t
What type of personality disorder may be prone to being abused?
dependent
67.
Exercise• What type of personality disorder will avoid
interpersonal contacts?
• avoidant
• What is the motivation for an avoidant
personality disordered individual to avoid
interpersonal contacts?
• fear of criticism and rejection
• What type of personality disorder will not apply
for certain jobs or take certain risks?
• avoidant
68.
Exercise• 60 yo male referred by wife for depression
• Past Hx: negative
Soc Hx: Fired due to poor peer relationships and starting conflicts, suing
job for discrimination and slander
• paranoid
• 40 yo female brought in by paramedics unconscious, OD on diazepam
Past Hx: Husband's death 2 weeks ago, treated for anxiety in 20s.
Soc Hx: Married 22 yrs, never employed, no children, or close relatives.
• dependent
• 35 year old male brought in by police for trespassing and assault
Past Hx: 2 suicide attempts, treatment for depression,
methamphetamine abuse
Social: Unemployed writer/actor. Divorced. Recent breakup with 18 y.o.
girlfriend/victim. 2 year prison term for embezzlement.
• borderline, antisocial
69.
Take home points• Personality disorders are common and more
common in your practice then the general
population
• Identifying personality disordered patients informs
how best to approach them
• Don’t forget to screen for comorbid diagnoses
• Ask for help if you are feeling overwhelmed!

















 psychology
psychology