Similar presentations:
Respiratory physiology
1.
• Respiratory Physiology2. Lecture Outline
• Basics of the Respiratory System– Functions & functional anatomy
Gas Laws
Ventilation
Diffusion & Solubility
Gas Exchange
– Lungs
– Tissues
• Gas Transport in Blood
• Regulation of Ventilation & Impacts on
– Gas levels, pH
3. Basics of the Respiratory System General Functions
• Exchange of gases• Directionality depends on gradients!
– Atmosphere to blood
– Blood to tissues
• Regulation of pH
– Dependent on rate of CO2 release
• Protection
• Vocalization
• Synthesis
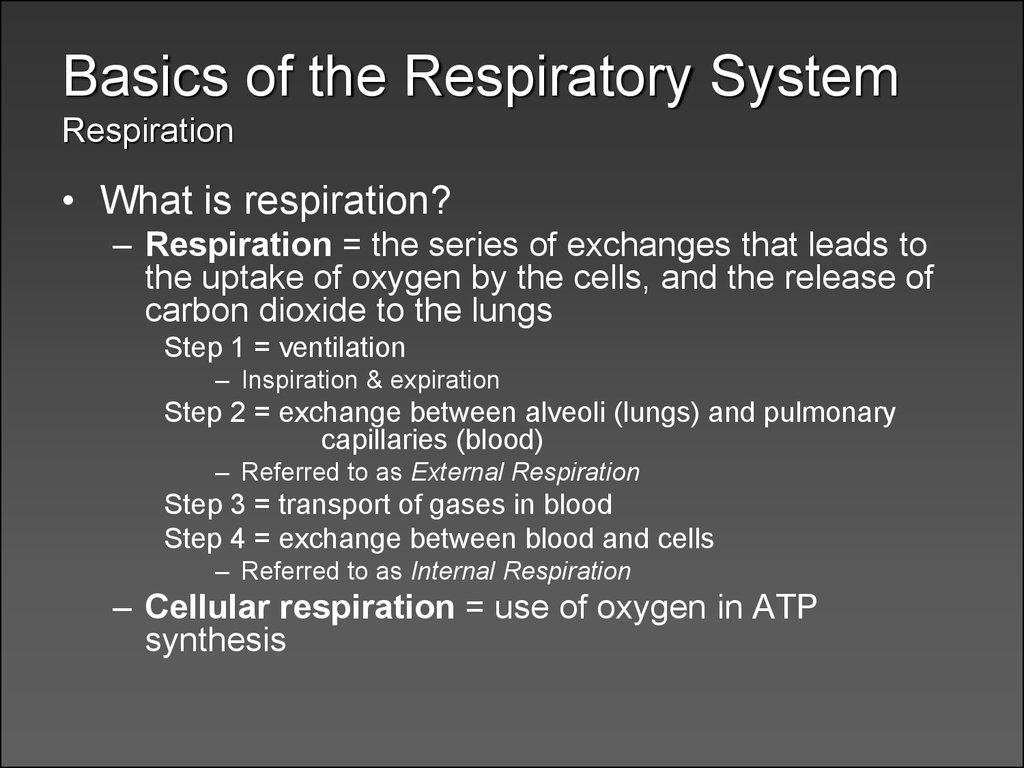
4. Basics of the Respiratory System Respiration
• What is respiration?– Respiration = the series of exchanges that leads to
the uptake of oxygen by the cells, and the release of
carbon dioxide to the lungs
Step 1 = ventilation
– Inspiration & expiration
Step 2 = exchange between alveoli (lungs) and pulmonary
capillaries (blood)
– Referred to as External Respiration
Step 3 = transport of gases in blood
Step 4 = exchange between blood and cells
– Referred to as Internal Respiration
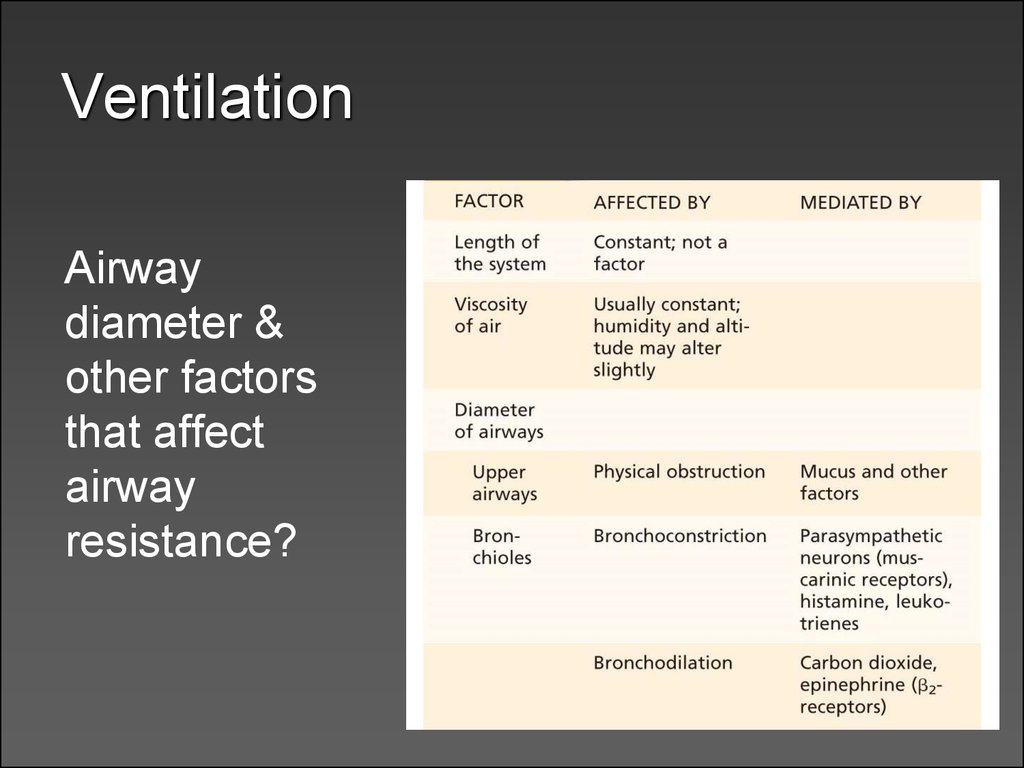
– Cellular respiration = use of oxygen in ATP
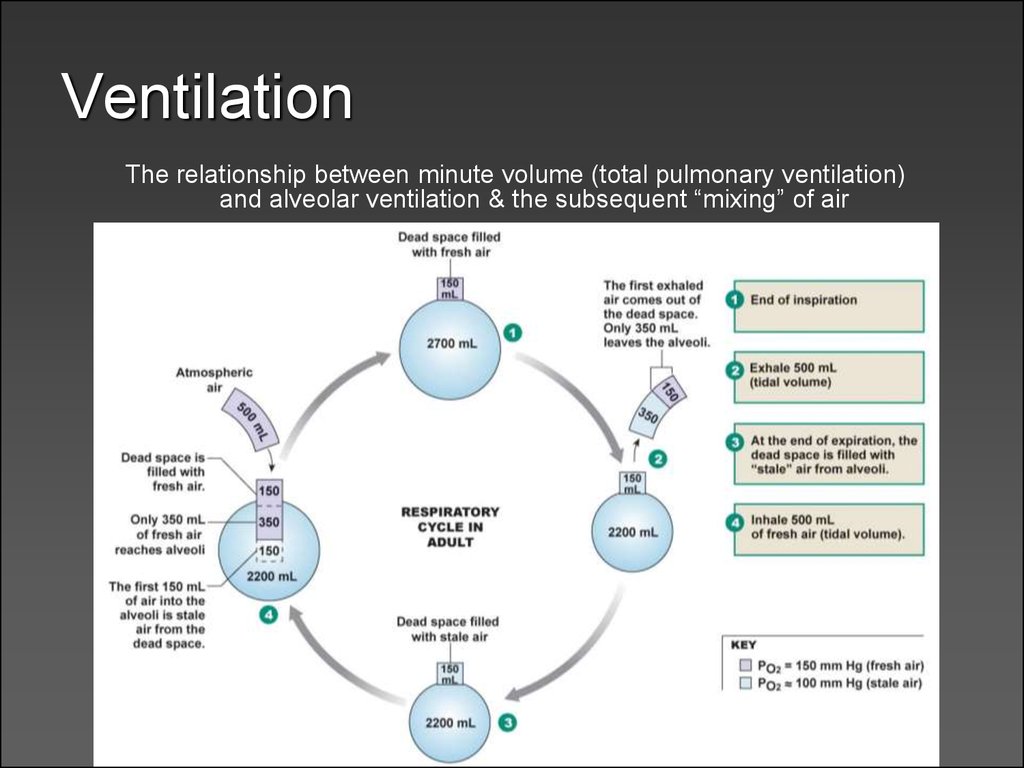
synthesis
5.
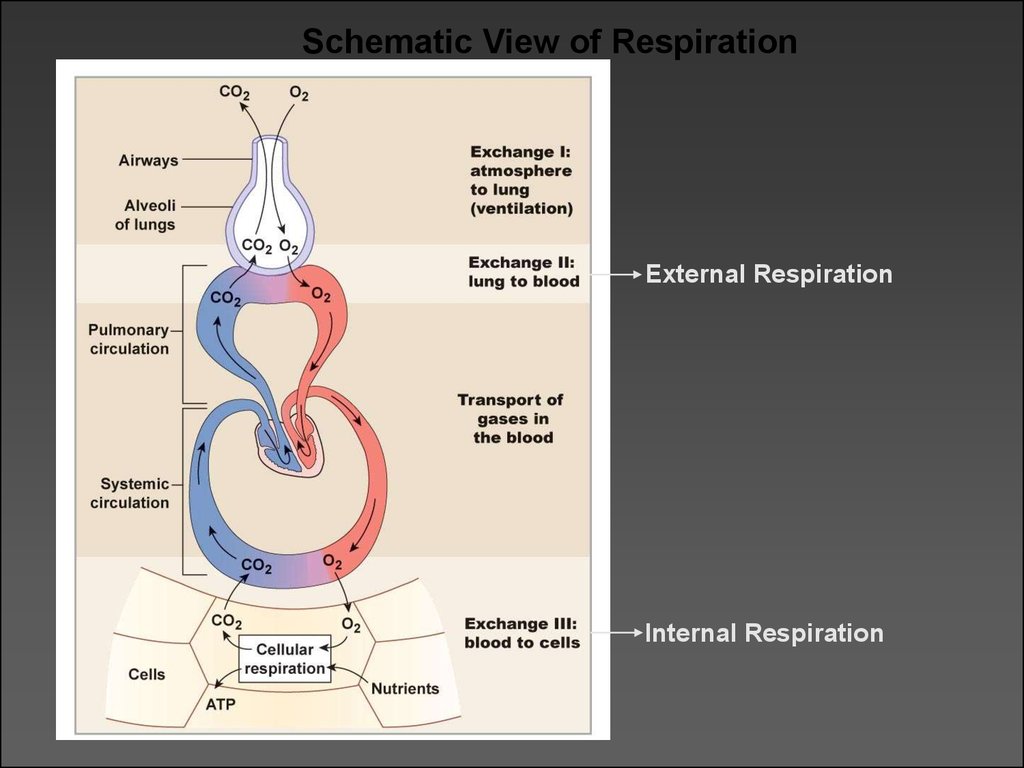
Schematic View of RespirationExternal Respiration
Internal Respiration
6. Basics of the Respiratory System Functional Anatomy
• What structural aspects must be considered in theprocess of respiration?
– The conduction portion
– The exchange portion
– The structures involved with
ventilation
• Skeletal & musculature
• Pleural membranes
• Neural pathways
• All divided into
– Upper respiratory tract
• Entrance to larynx
– Lower respiratory tract
• Larynx to alveoli (trachea
to lungs)
7. Basics of the Respiratory System Functional Anatomy
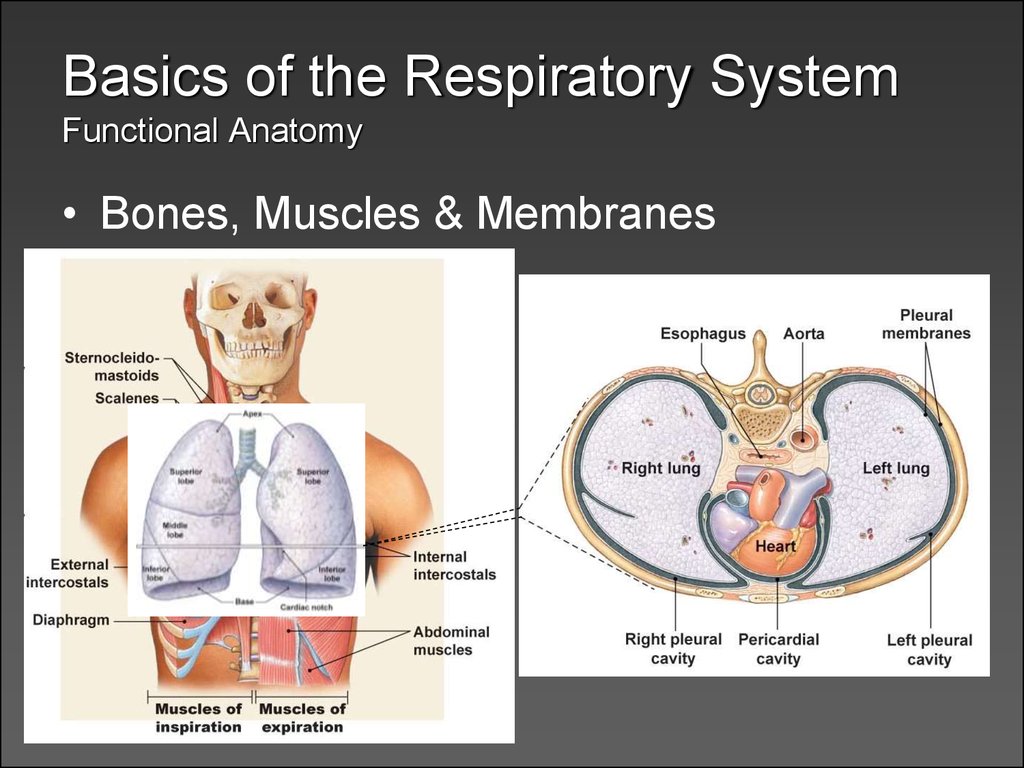
• Bones, Muscles & Membranes8. Basics of the Respiratory System Functional Anatomy
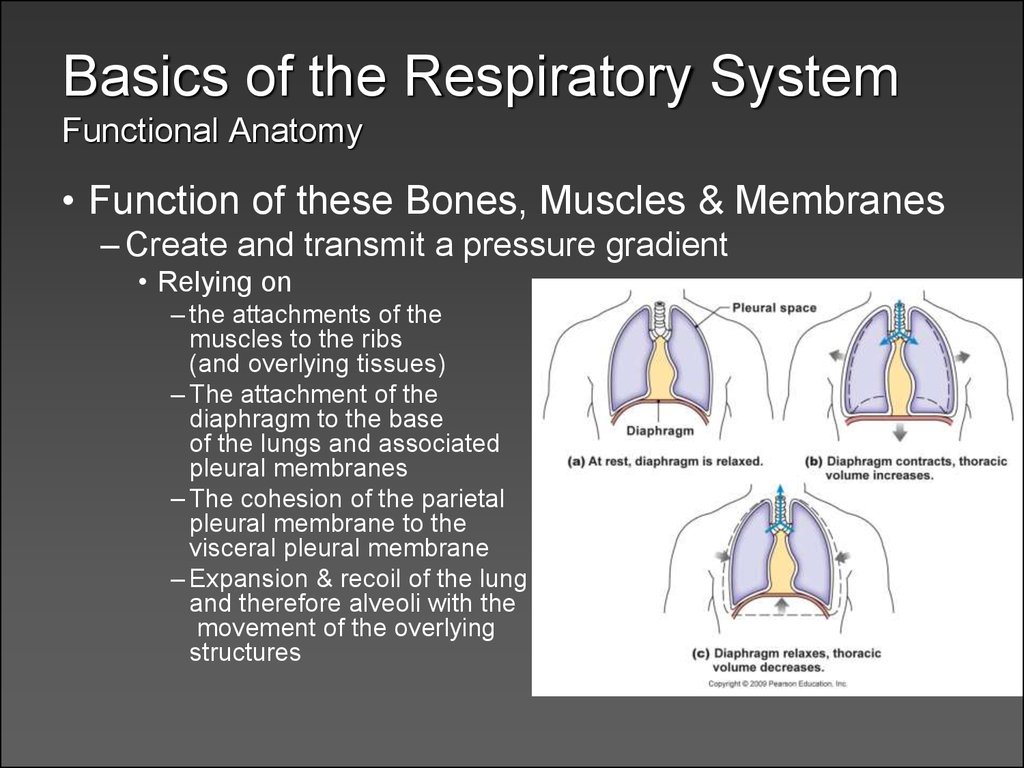
• Function of these Bones, Muscles & Membranes– Create and transmit a pressure gradient
• Relying on
– the attachments of the
muscles to the ribs
(and overlying tissues)
– The attachment of the
diaphragm to the base
of the lungs and associated
pleural membranes
– The cohesion of the parietal
pleural membrane to the
visceral pleural membrane
– Expansion & recoil of the lung
and therefore alveoli with the
movement of the overlying
structures
9. Basics of the Respiratory System Functional Anatomy
• Pleural Membrane Detail– Cohesion between parietal and visceral layers
is due to serous fluid in the pleural cavity
• Fluid (30 ml of fluid) creates an attraction between
the two sheets of membrane
• As the parietal membrane expands due to
expansion of the thoracic cavity it “pulls” the
visceral membrane with it
– And then pulls the underlying structures which expand as
well
• Disruption of the integrity of the pleural membrane
will result in a rapid equalization of pressure and
loss of ventilation function = collapsed lung or
pneumothorax
10. Basics of the Respiratory System Functional Anatomy
• The Respiratory Tree– connecting the external environment to the
exchange portion of the lungs
– similar to the vascular component
– larger airway = higher flow & velocity
• small cross-sectional area
– smaller airway = lower flow & velocity
• large cross-sectional area
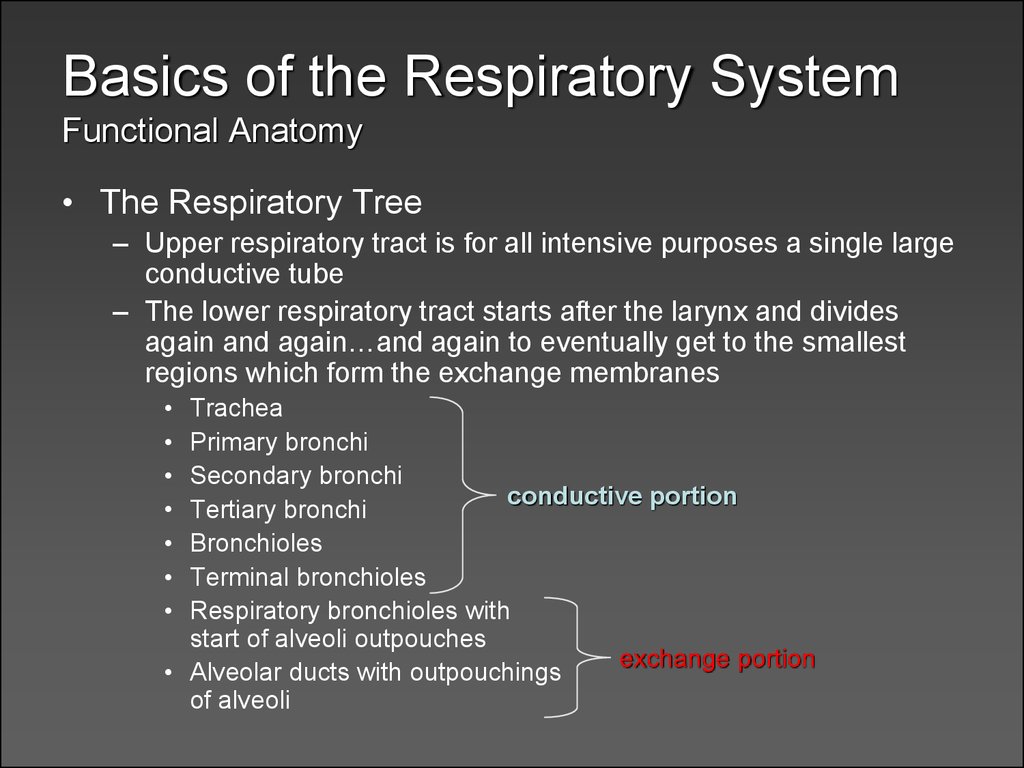
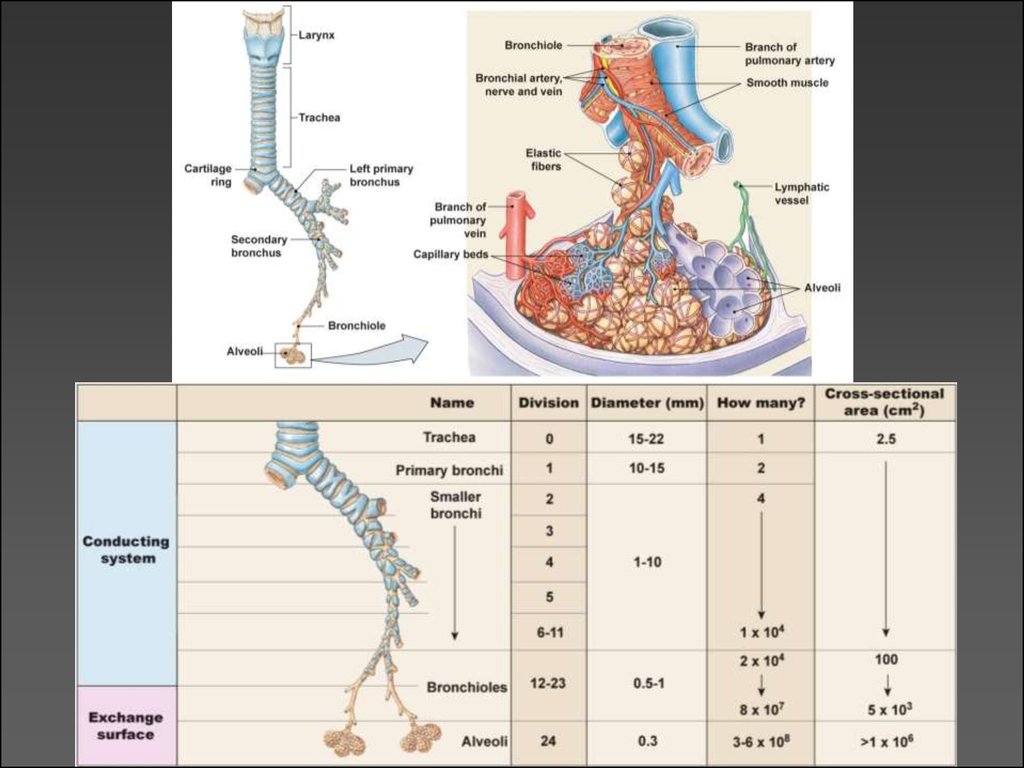
11. Basics of the Respiratory System Functional Anatomy
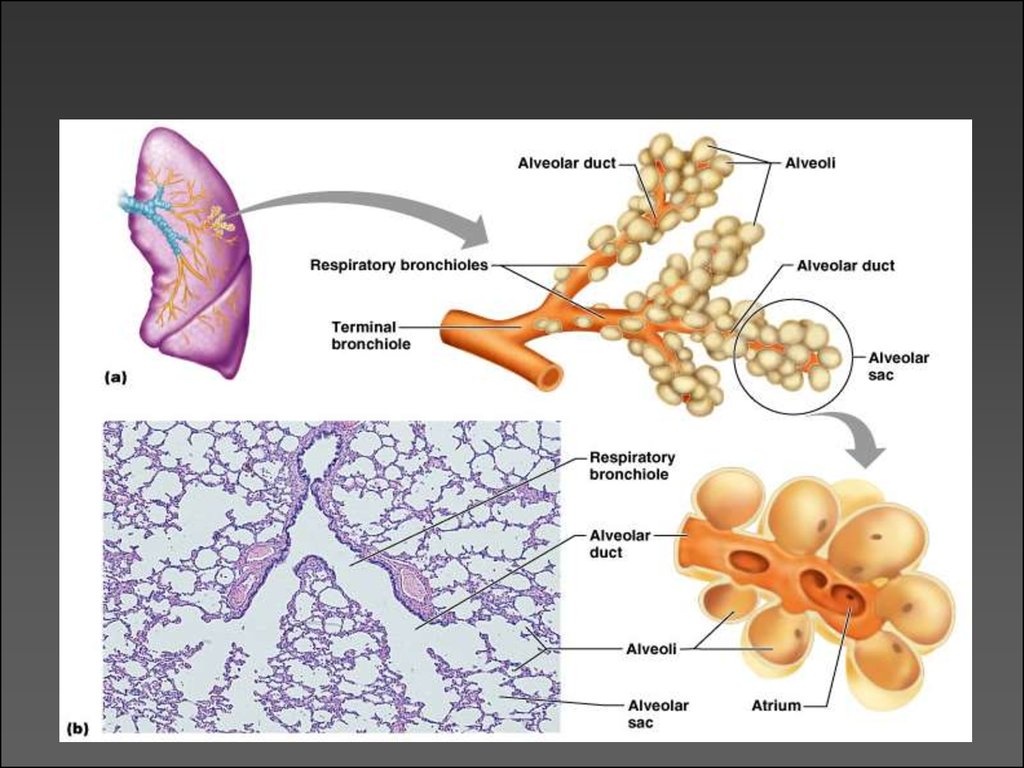
• The Respiratory Tree– Upper respiratory tract is for all intensive purposes a single large
conductive tube
– The lower respiratory tract starts after the larynx and divides
again and again…and again to eventually get to the smallest
regions which form the exchange membranes
Trachea
Primary bronchi
Secondary bronchi
conductive portion
Tertiary bronchi
Bronchioles
Terminal bronchioles
Respiratory bronchioles with
start of alveoli outpouches
exchange portion
• Alveolar ducts with outpouchings
of alveoli
12.
13.
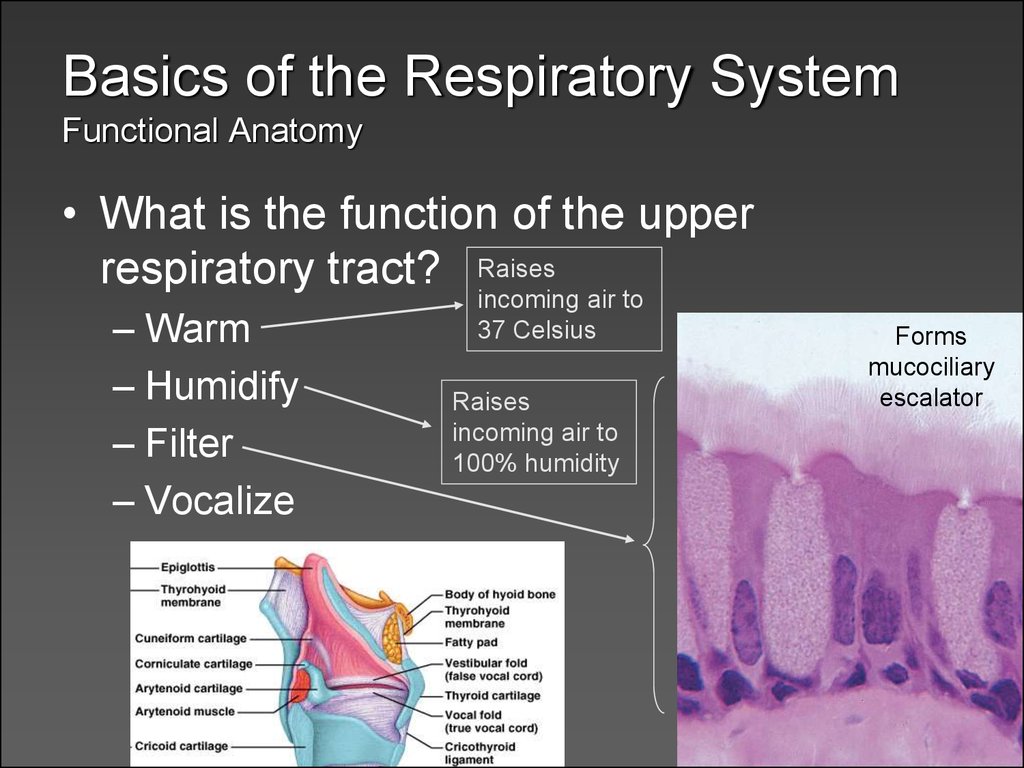
14. Basics of the Respiratory System Functional Anatomy
• What is the function of the upperrespiratory tract? Raises
– Warm
– Humidify
– Filter
– Vocalize
incoming air to
37 Celsius
Raises
incoming air to
100% humidity
Forms
mucociliary
escalator
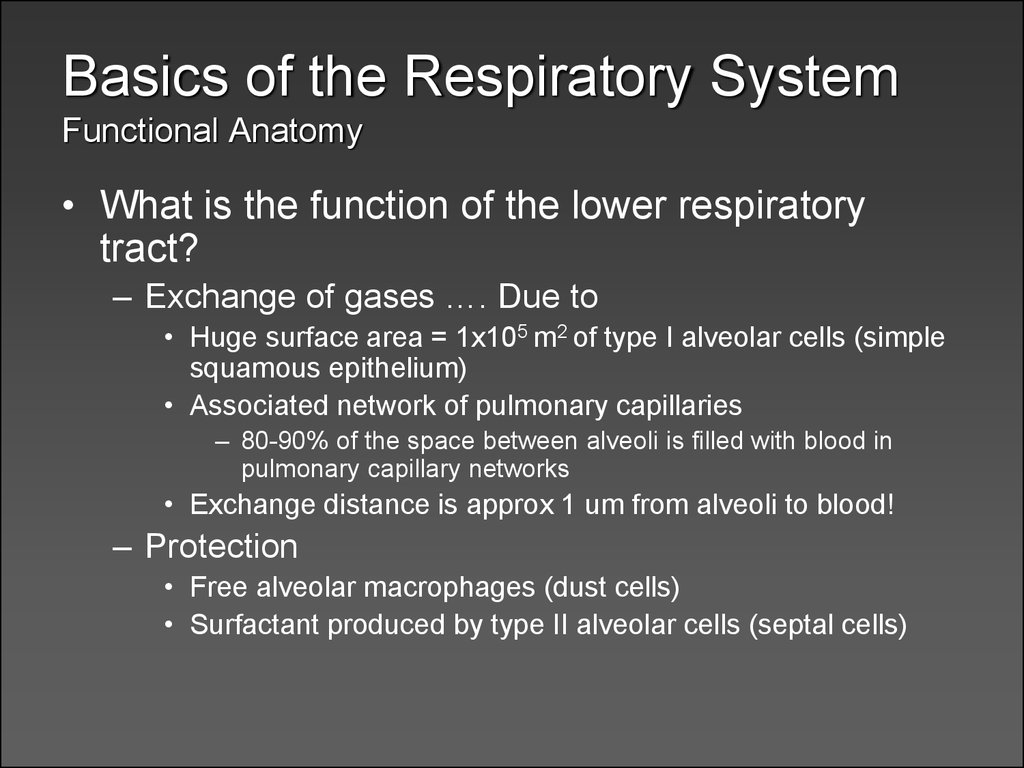
15. Basics of the Respiratory System Functional Anatomy
• What is the function of the lower respiratorytract?
– Exchange of gases …. Due to
• Huge surface area = 1x105 m2 of type I alveolar cells (simple
squamous epithelium)
• Associated network of pulmonary capillaries
– 80-90% of the space between alveoli is filled with blood in
pulmonary capillary networks
• Exchange distance is approx 1 um from alveoli to blood!
– Protection
• Free alveolar macrophages (dust cells)
• Surfactant produced by type II alveolar cells (septal cells)
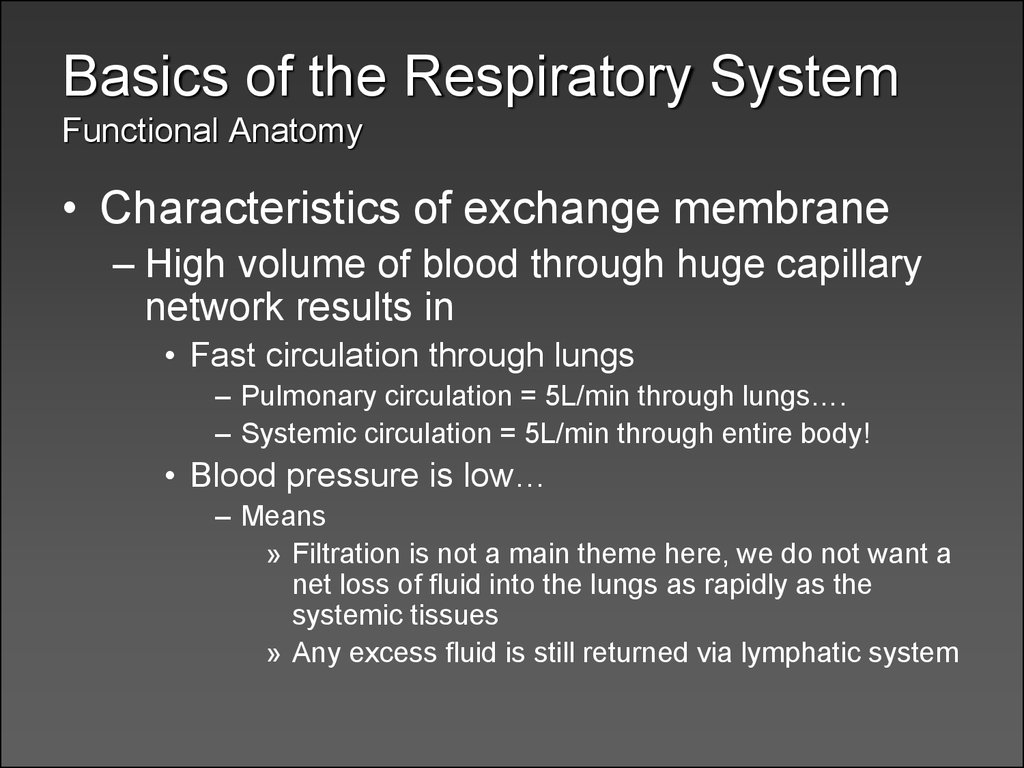
16. Basics of the Respiratory System Functional Anatomy
• Characteristics of exchange membrane– High volume of blood through huge capillary
network results in
• Fast circulation through lungs
– Pulmonary circulation = 5L/min through lungs….
– Systemic circulation = 5L/min through entire body!
• Blood pressure is low…
– Means
» Filtration is not a main theme here, we do not want a
net loss of fluid into the lungs as rapidly as the
systemic tissues
» Any excess fluid is still returned via lymphatic system
17. Basics of the Respiratory System Functional Anatomy
• Sum-up of functional anatomy– Ventilation?
– Exchange?
– Vocalization?
– Protection?
18. Respiratory Physiology Gas Laws
• Basic Atmospheric conditions– Pressure is typically measured in mm Hg
– Atmospheric pressure is 760 mm Hg
– Atmospheric components
Nitrogen = 78% of our atmosphere
Oxygen = 21% of our atmosphere
Carbon Dioxide = .033% of our atmosphere
Water vapor, krypton, argon, …. Make up the rest
• A few laws to remember
–
–
–
–
Dalton’s law
Fick’s Laws of Diffusion
Boyle’s Law
Ideal Gas Law
19. Respiratory Physiology Gas Laws
• Dalton’s Law– Law of Partial Pressures
• “each gas in a mixture of gases will exert a pressure
independent of other gases present”
Or
• The total pressure of a mixture of gases is equal to the sum
of the individual gas pressures.
– What does this mean in practical application?
• If we know the total atmospheric pressure (760 mm Hg) and
the relative abundances of gases (% of gases)
– We can calculate individual gas effects!
– Patm x % of gas in atmosphere = Partial pressure of any
atmospheric gas
» PO2 = 760mmHg x 21% (.21) = 160 mm Hg
• Now that we know the partial pressures we know the
gradients that will drive diffusion!
20. Respiratory Physiology Gas Laws
• Fick’s Laws of Diffusion– Things that affect rates of diffusion
• Distance to diffuse
• Gradient sizes
• Diffusing molecule sizes
• Temperature
– What is constant & therefore out of our realm
of concern?
• So it all comes down to partial pressure gradients
of gases… determined by Dalton’s Law!
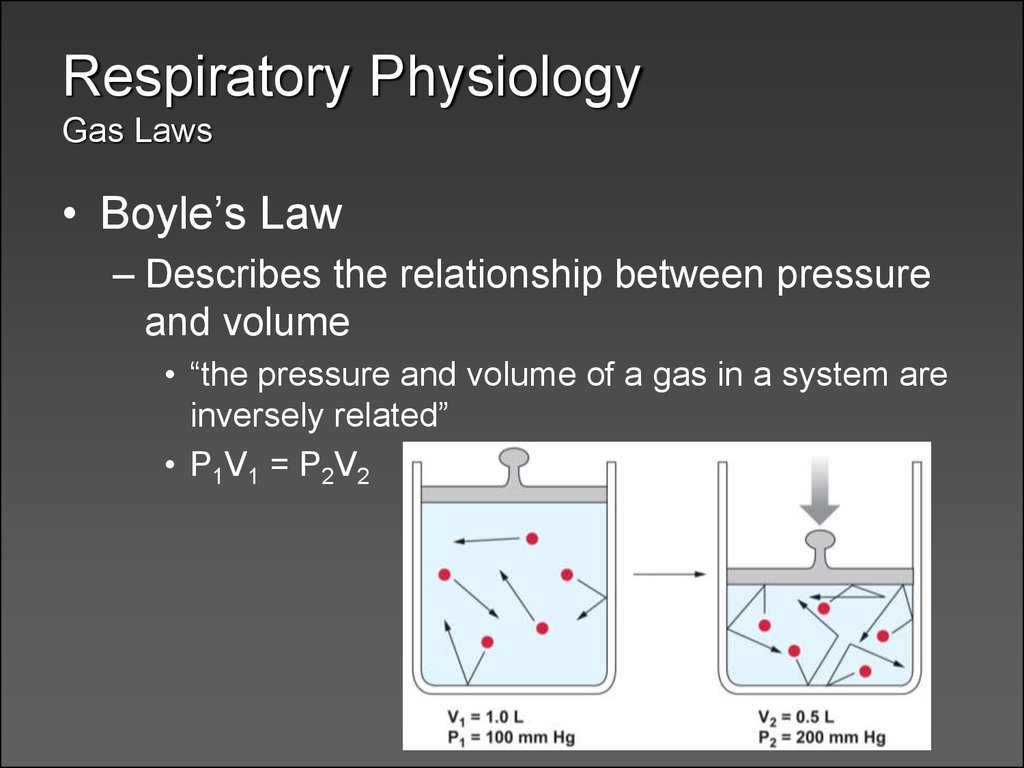
21. Respiratory Physiology Gas Laws
• Boyle’s Law– Describes the relationship between pressure
and volume
• “the pressure and volume of a gas in a system are
inversely related”
• P1V1 = P2V2
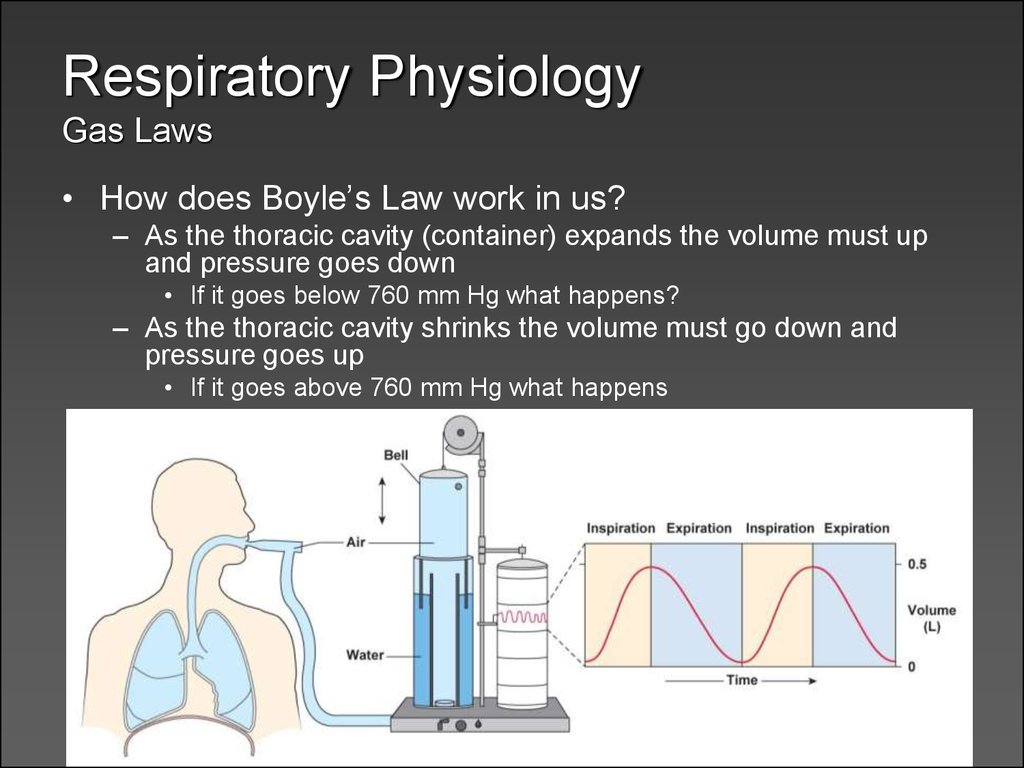
22. Respiratory Physiology Gas Laws
• How does Boyle’s Law work in us?– As the thoracic cavity (container) expands the volume must up
and pressure goes down
• If it goes below 760 mm Hg what happens?
– As the thoracic cavity shrinks the volume must go down and
pressure goes up
• If it goes above 760 mm Hg what happens
23. Respiratory Physiology Gas Laws
• Ideal Gas law– The pressure and volume of a container of
gas is directly related to the temperature of
the gas and the number of molecules in the
container
– PV = nRT
• n = moles of gas
• T = absolute temp
• R = universal gas constant @ 8.3145 J/K·mol
– Do we care?
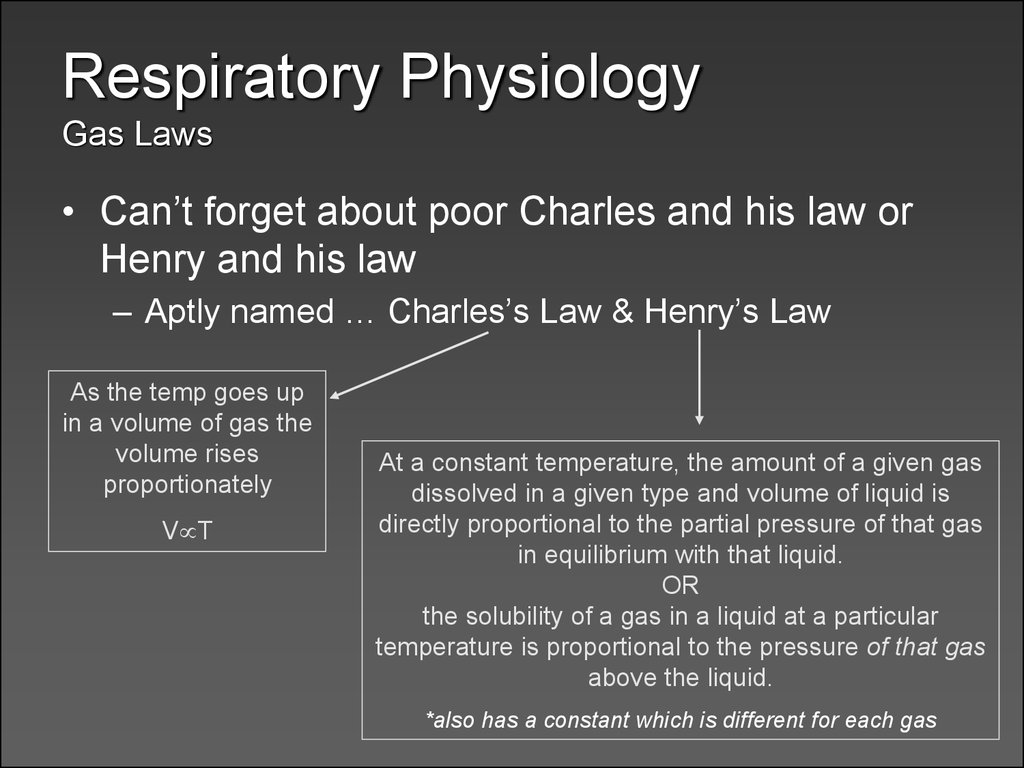
24. Respiratory Physiology Gas Laws
• Can’t forget about poor Charles and his law orHenry and his law
– Aptly named … Charles’s Law & Henry’s Law
As the temp goes up
in a volume of gas the
volume rises
proportionately
V T
At a constant temperature, the amount of a given gas
dissolved in a given type and volume of liquid is
directly proportional to the partial pressure of that gas
in equilibrium with that liquid.
OR
the solubility of a gas in a liquid at a particular
temperature is proportional to the pressure of that gas
above the liquid.
*also has a constant which is different for each gas
25. Ventilation
• Terminology– Inspiration = the movement of air into the respiratory tracts
(upper & lower)
– Expiration = movement of air out of the respiratory tracts
– Respiratory cycle is one inspiration followed by an expiration
• Cause of Inspiration?
– Biological answer
• Contraction of the inspiratory muscles causes an increase in the
thoracic cavity size, thus allowing air to enter the respiratory tract
– Physics answer
• As the volume in the thoracic cavity increases (due to inspiratory
muscle action) the pressure within the respiratory tract drops below
atmospheric pressure, creating a pressure gradient which causes
molecular movement to favor moving into the respiratory tract
– Cause of Expiration?
26. Ventilation
Besides thediaphragm (only
creates about
60-75% of the
volume change)
what are the
muscles of
inspiration &
expiration?
27. Ventilation
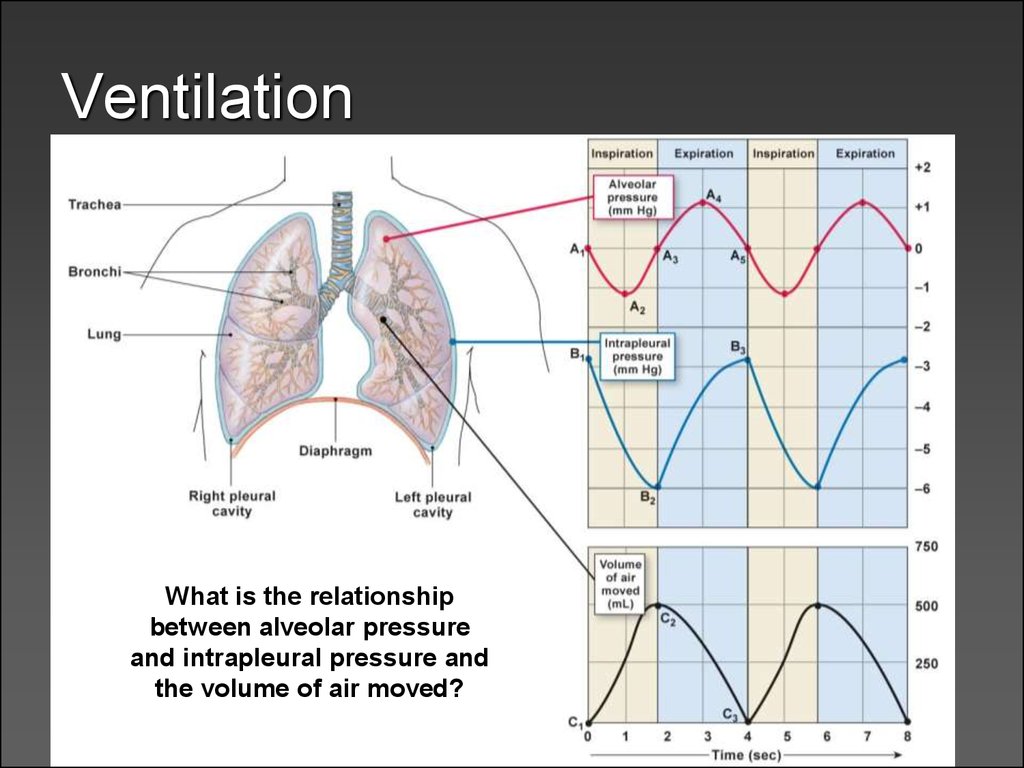
What is the relationshipbetween alveolar pressure
and intrapleural pressure and
the volume of air moved?
28. Ventilation
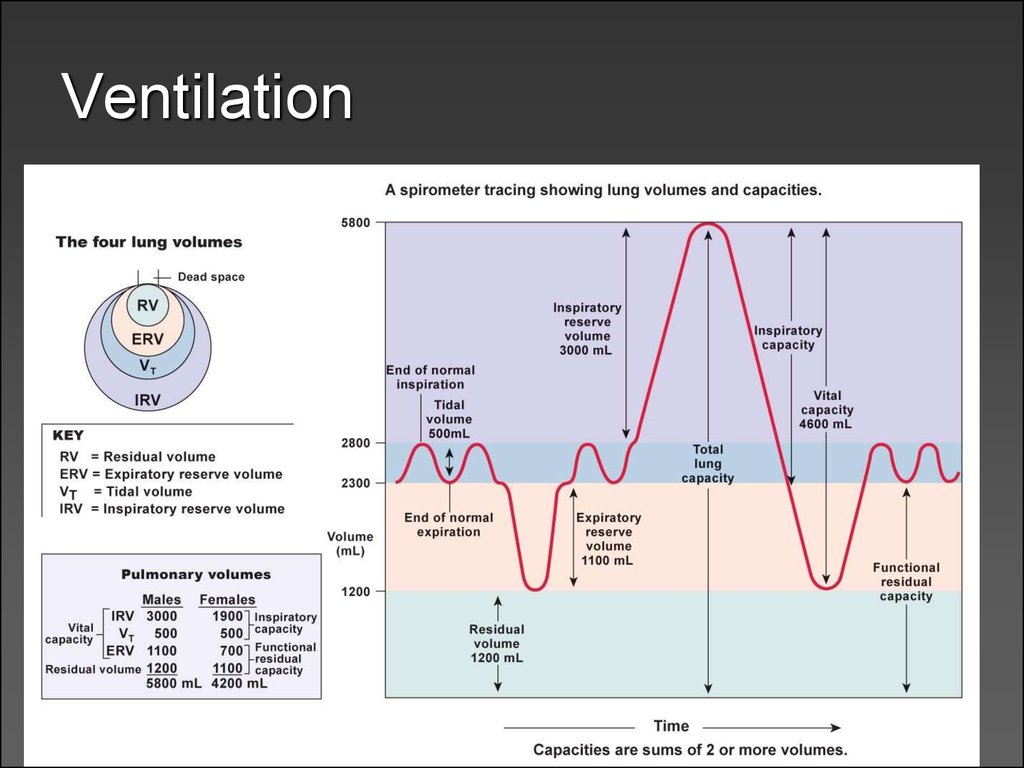
• What are the different respiratorypatterns?
– Quiet breathing (relaxed)
– Forced inspirations & expirations
• Respiratory volumes follow these
respiratory patterns…
29. Ventilation
30. Ventilation
• Inspiration– Occurs as alveolar pressure drops below atmospheric
pressure
• For convenience atmospheric pressure = 0 mm Hg
– A (-) value then indicates pressure below atmospheric P
– A (+) value indicates pressure above atmospheric P
• At the start of inspiration (time = 0),
– atmospheric pressure = alveolar pressure
» No net movement of gases!
• At time 0 to 2 seconds
– Expansion of thoracic cage and corresponding pleural
membranes and lung tissue causes alveolar pressure to drop to
-1 mm Hg
– Air enters the lungs down the partial pressure gradient
31. Ventilation
• Expiration– Occurs as alveolar pressure elevates above
atmospheric pressure due to a shrinking
thoracic cage
• At time 2-4 seconds
– Inspiratory muscles relax, elastic tissue of corresponding
structures initiates a recoil back to resting state
– This decreases volume and correspondingly increases
alveolar pressure to 1 mm Hg
» This is above atmospheric pressure, causing…?
• At time 4 seconds
– Atmospheric pressure once again equals alveolar
pressure and there is no net movement
32. Ventilation
• Both inspiration and expiration can bemodified
– Forced or active inspiration
– Forced or active expiration
– The larger and quicker the expansion of the
thoracic cavity, the larger the gradient and
• The faster air moves down its pressure gradient
33. Ventilation
• Things to consider– surfactant effect
– airway diameter
– Minute volume respiration (ventilation rate times tidal
volume) & anatomical dead space
• Leading to a more accurate idea of alveolar ventilation rates
– Changes in ventilation patterns
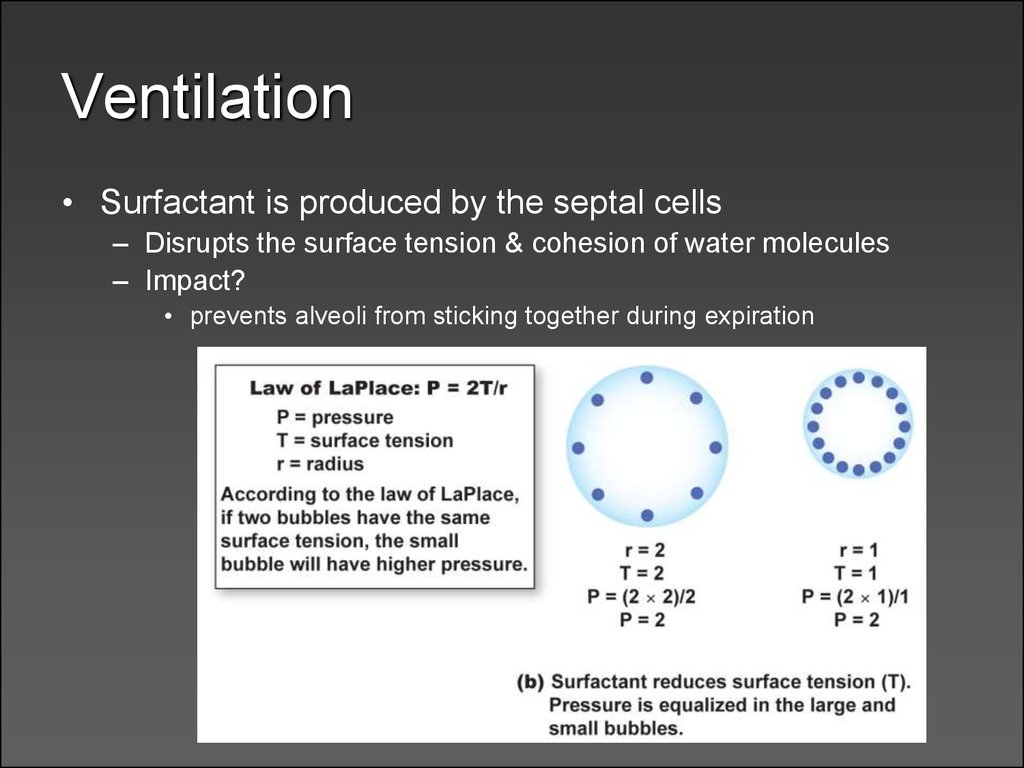
34. Ventilation
• Surfactant is produced by the septal cells– Disrupts the surface tension & cohesion of water molecules
– Impact?
• prevents alveoli from sticking together during expiration
35. Ventilation
Airwaydiameter &
other factors
that affect
airway
resistance?
36. Ventilation
The relationship between minute volume (total pulmonary ventilation)and alveolar ventilation & the subsequent “mixing” of air
37. Next Time…
• Diffusion and Solubility– Gas composition in the alveoli
• Gas exchange
• Gas transport in blood
• Regulation of pulmonary function



 biology
biology