Similar presentations:
Dermatology. Skin and soft tissue infections dermatitis
1.
DERMATOLOGYSKIN AND SOFT TISSUE INFECTIONS
DERMATITIS
2.
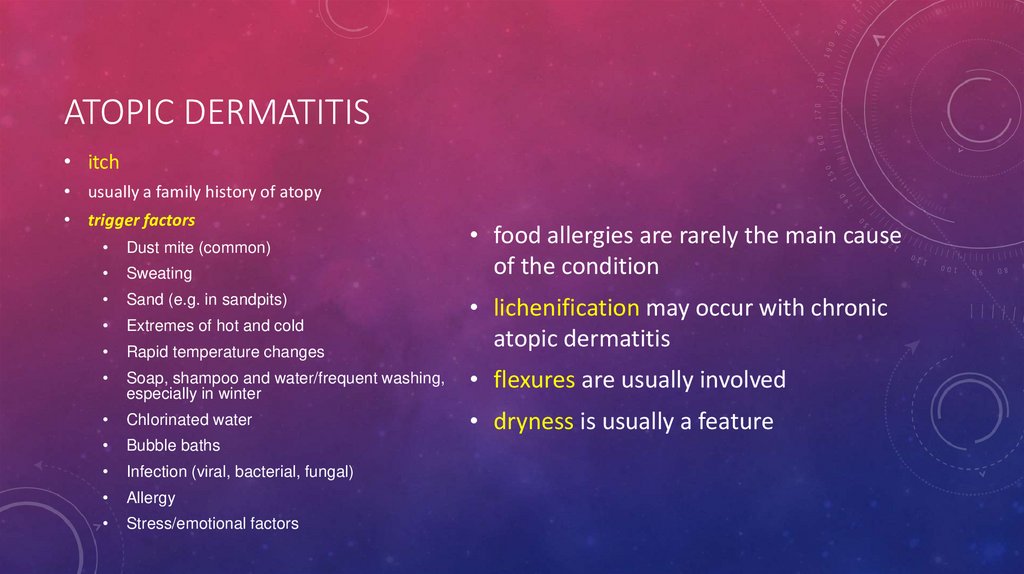
ATOPIC DERMATITIS• itch
• usually a family history of atopy
• trigger factors
• food allergies are rarely the main cause
of the condition
Dust mite (common)
Sweating
Sand (e.g. in sandpits)
Extremes of hot and cold
Rapid temperature changes
• lichenification may occur with chronic
atopic dermatitis
Soap, shampoo and water/frequent washing,
especially in winter
• flexures are usually involved
Chlorinated water
• dryness is usually a feature
Bubble baths
Infection (viral, bacterial, fungal)
Allergy
Stress/emotional factors
3.
ATOPIC DERMATITISCriteria for diagnosis
• Itch
• Typical morphology and distribution
• Dry skin
• History of atopy
• Chronic relapsing dermatitis
4.
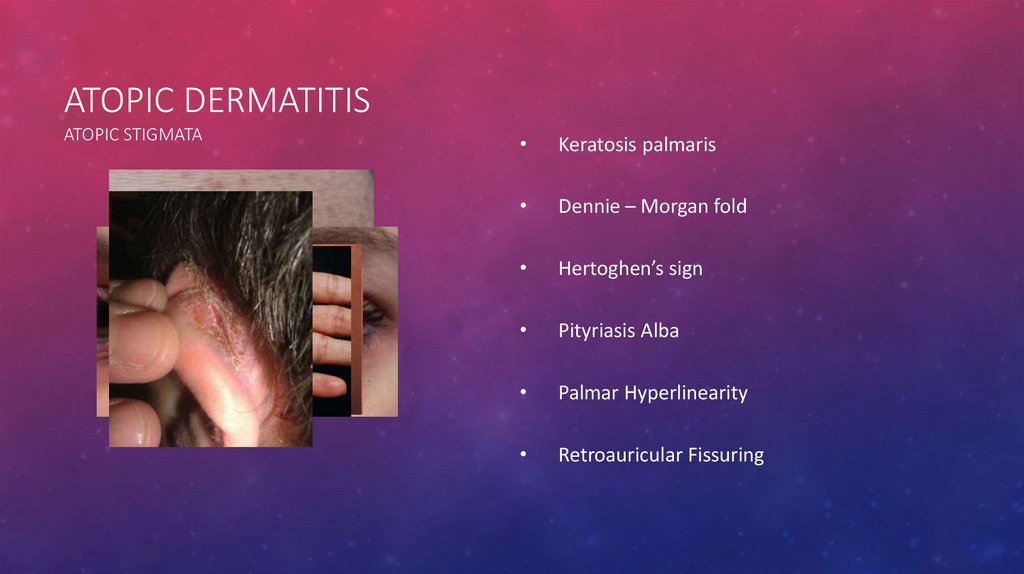
ATOPIC DERMATITISATOPIC STIGMATA
Keratosis palmaris
Dennie – Morgan fold
Hertoghen’s sign
Pityriasis Alba
Palmar Hyperlinearity
Retroauricular Fissuring
5.
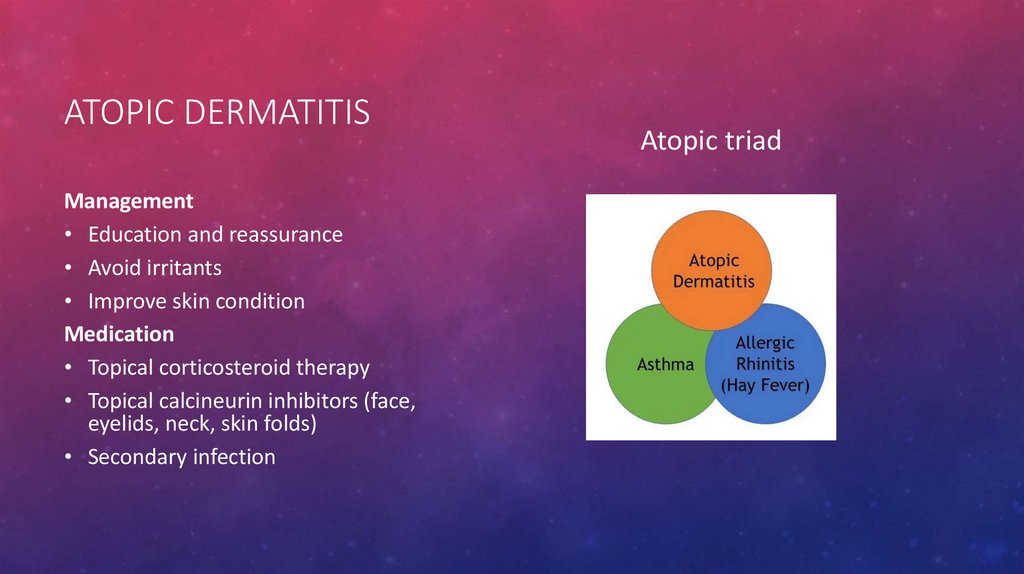
ATOPIC DERMATITISManagement
• Education and reassurance
• Avoid irritants
• Improve skin condition
Medication
• Topical corticosteroid therapy
• Topical calcineurin inhibitors (face,
eyelids, neck, skin folds)
• Secondary infection
Atopic triad
6.
LICHEN SIMPLEX CHRONICUS• Circumscribed thick plaques of lichenification
• Caused by repeated rubbing and scratching of
previously normal skin
• Due to chronic itch of unknown cause
• At sites within reach of fingers (e.g. neck,
forearms, thighs, vulva, heels, fingers)
• May arise from habit
Treatment
• Refrain from scratching
• Topical corticosteroid ointment
7.
CONTACT DERMATITIS• Site and shape suggest contact
• Dermatitis ranges from faint erythema to ‘water
melon’ face oedema
• Worse in peri-orbital region, genitalia and hairy
skin
Think of Rhus, Grevillea or poison ivy allergy
if linear blisters on forearms and/or puffy eyes
• Improvement when off work or on holiday
Treatment
• Determine cause and remove it
• Topical corticosteroid
• Oral prednisolone for severe cases
8.
CONTACT DERMATITISPATCH TEST
9.
STASIS DERMATITISrisk factors:
• varicose veins
• high blood pressure
• obesity, vein surgeries
• multiple pregnancies
• a history of blood clots in the legs
• congestive heart failure
• kidney failure
• certain lifestyle factors such as getting little
physical activity or having a job that
involves hours of sitting or standing
10.
STASIS DERMATITISclinical features:
• Bilateral
• redness in lighter skin tones that may appear
brown, purple, gray or ashen in darker skin tones
• itching
• scaling
• dryness
• a heavy or achy feeling after long periods of sitting
or standing
• increased risk of developing contact dermatitis
11.
STASIS DERMATITISTreatment
• compression stockings
• diuretics
• elevating legs above the heart
• for red or darker-colored, itchy skin,
dermatologists may prescribe a topical
corticosteroid
• topical or oral antibiotic if skin is infected
12.
SEBORRHEIC DERMATITISAdults
• Any age from teenage onwards
• Quite pruritic
• The head is a common area: scalp and ears, face,
eyebrows, eyelids, nasolabial folds
• Less involvement of inguinal areas
• Scaling on scalp causing dandruff and/or erythematous
patches
• Worse with stress and fatigue
It is a chronic, recurring condition
13.
SEBORRHEIC DERMATITISKids
• Age of onset Mainly within first 3
months
• Itchiness Nil or mild
• Distribution Scalp, cheeks, folds of
neck, axillae, folds of elbows and knees
• Yellow-red greasy, crusted and scaling
plaques on scalp and face
• Napkin rash Common
Benign and self-limiting
14.
SEBORRHEIC DERMATITISManagement
• Likely to resolve on it’s own
• Soft baby brush and some baby oil
• Anti-fungal shampoos or cream
• Topical steroids
15.
CELLULITIS• Cellulitis is a common bacterial infection
• The most common bacteria causing cellulitis are Streptococcus pyogenes (two-thirds of cases) and
Staphylococcus aureus (one third)
• Clinical features:
• Cellulitis can affect any site, most often a limb and can be around the eye – periorbital cellulitis
• unilateral
• It can occur by itself or complicate an underlying skin condition or wound.
16.
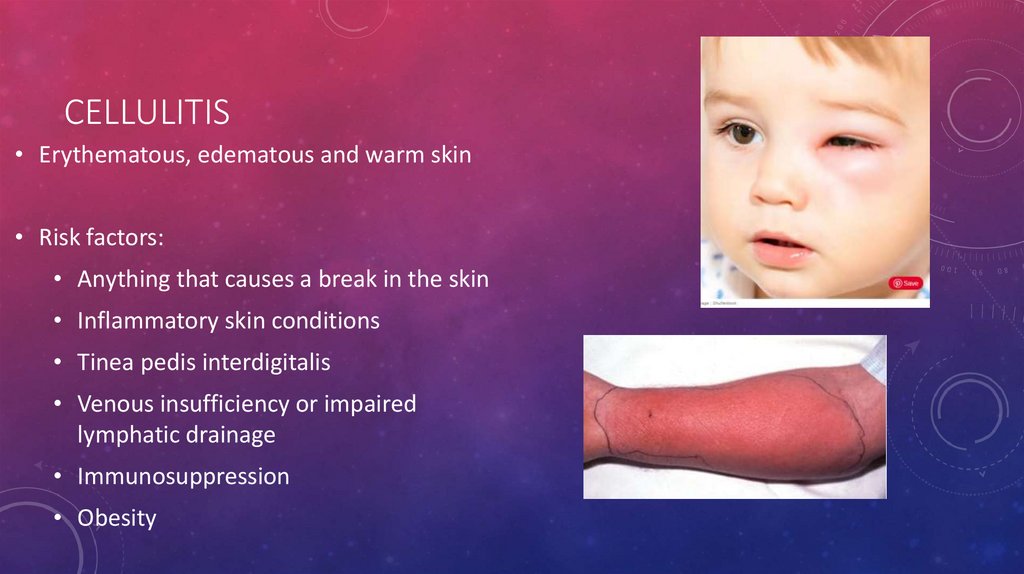
CELLULITIS• Erythematous, edematous and warm skin
• Risk factors:
• Anything that causes a break in the skin
• Inflammatory skin conditions
• Tinea pedis interdigitalis
• Venous insufficiency or impaired
lymphatic drainage
• Immunosuppression
• Obesity
17.
CELLULITISTreatment
Non purulent: Cephalexin Cefazolin
Purulent: TMP, Clindamycin or
Tetracyclines
Systemically ‘’toxic’’ – vancomycin or
daptomycin
18.
OSTEOMYELITIS• is mainly a disease of childhood
• Main organisms—S. aureus, S.
pneumonia, Kingella kingae,
Propionibacterium acnes
• Sources of infection—boils, abscesses,
septic toes, surgical procedures
• Diagnostic: X-Ray, rad MRI
• Treatment: debridement
19.
GAS GANGRENE• necrotising soft tissue infection can involve skin and
subcutaneous fat, fascia and muscle
• caused by clostridium species
• diagnosis based on clinical and radiographic pictures
20.
GAS GANGRENEClinical features
• sweet smelling odor
• edema, discoloration, ecchymosis
• blebs and hemorrhagic bullae
• ''dishwater pus'' discharge
• crepitus
• altered mental status
21.
GAS GANGRENEManagement
• Debridement and excision with possible
amputation
• Start benzylpenicillin 2.4 g IV, 4 hourly +
clindamycin
• Hyperbaric oxygen if available
22.
NECROTIZING FASCIITIS• Necrotising fasciitis is a very serious bacterial infection of the
soft tissue and fascia
• The bacteria multiply and release toxins and enzymes that
result in thrombosis in the blood vessels.
• The result is the destruction of the soft tissues and fascia.
• There is poor adherence of tissue to the fascia on incising the
site.
Necrotic tissue/pus oozes out of the fascial planes.
Dishwater-coloured fluid seeps out of the skin.
Typically, necrotising fasciitis does not bleed
23.
NECROTIZING FASCIITISTreatment
Immediate surgical debridement
The third generation cephalosporins
+ Clinda
24.
IMPETIGO• caused by Streptococcus pyogenes or
Staphylococcus aureus
• kids
• honey crusted lesions on the face
Treatment
• Soak and remove crusts with saline or soap
and water
• Amoxicillin (clindamycin)
25.
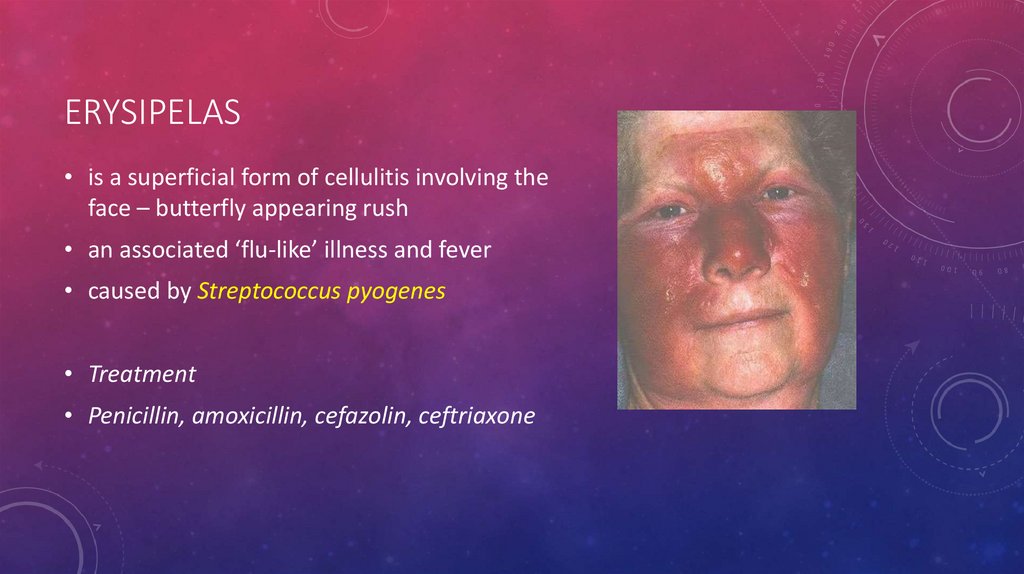
ERYSIPELAS• is a superficial form of cellulitis involving the
face – butterfly appearing rush
• an associated ‘flu-like’ illness and fever
• caused by Streptococcus pyogenes
• Treatment
• Penicillin, amoxicillin, cefazolin, ceftriaxone
26.
DIFFERENTIAL DIAGNOSIS27.
TINEATinea capitis
(Scalp ringworm)
hair loss, dry scaly areas,
redness, and itch
Tinea corporis
(Ringworm)
Well described,
circumscribed, moderately
scaled with central
cleaning
Tinea cruris
Jock itchy
Tinea unguium
(Dermatophyte
onychomycosis)
Tinea pedis
(Athlete’s foot)
Red, itchy feet, maceration
in between the toes
28.
CELLULITISERYSIPELAS
• Deep dermis and subcutaneous adipose
tissue
• Upper dermis and superficial lymphatic
• Indolent onset
• Acute onset
• Localised symptoms
• Fever, chills and malaise
• Non-purulent or purulent
• Non-purulent: Beta-hemolytic streptococci
• Purulent: Staph. aureus
• Clear demarcation
• Often raised
• Always non-purulent
























 medicine
medicine