Similar presentations:
Cholinoblockers
1.
Cholinoblockers2.
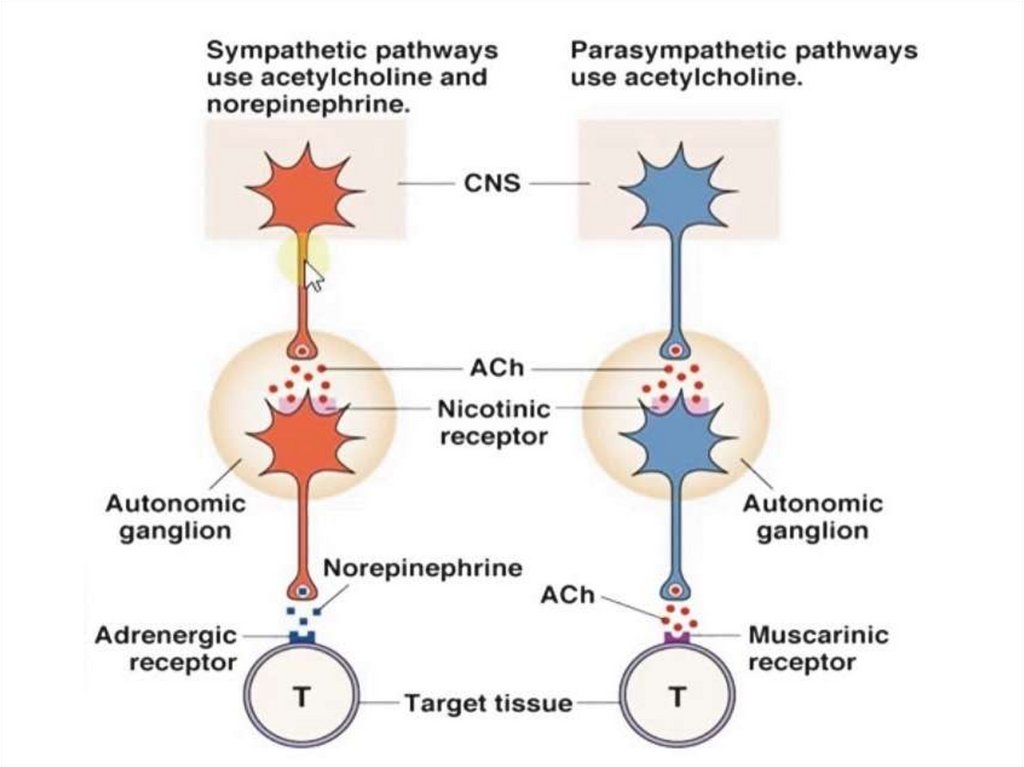
• Anticholinergics block the cholinergicreceptors, prevents their interaction with
acetylcholine and disrupts the conduction of
nerve impulses.
Cholinoblockers:
M-cholinoblockers
M,N-cholinoblockers
N-cholinoblockers
Ganglionblockers
Neuromuscular relaxants (curare-like drugs)
3.
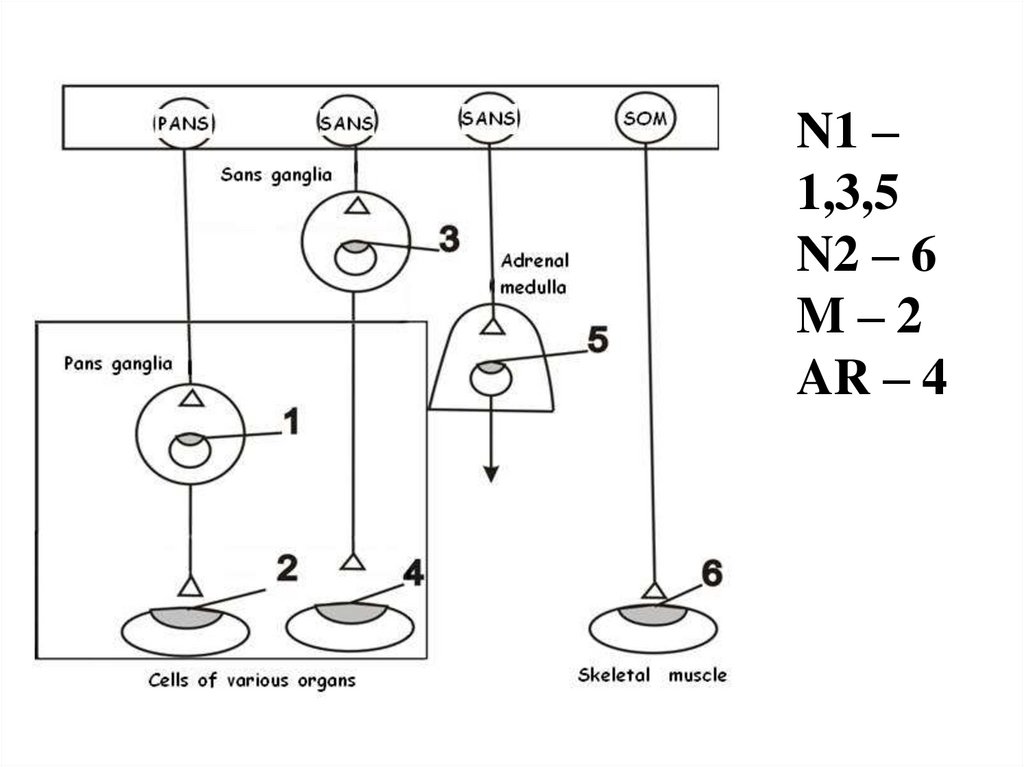
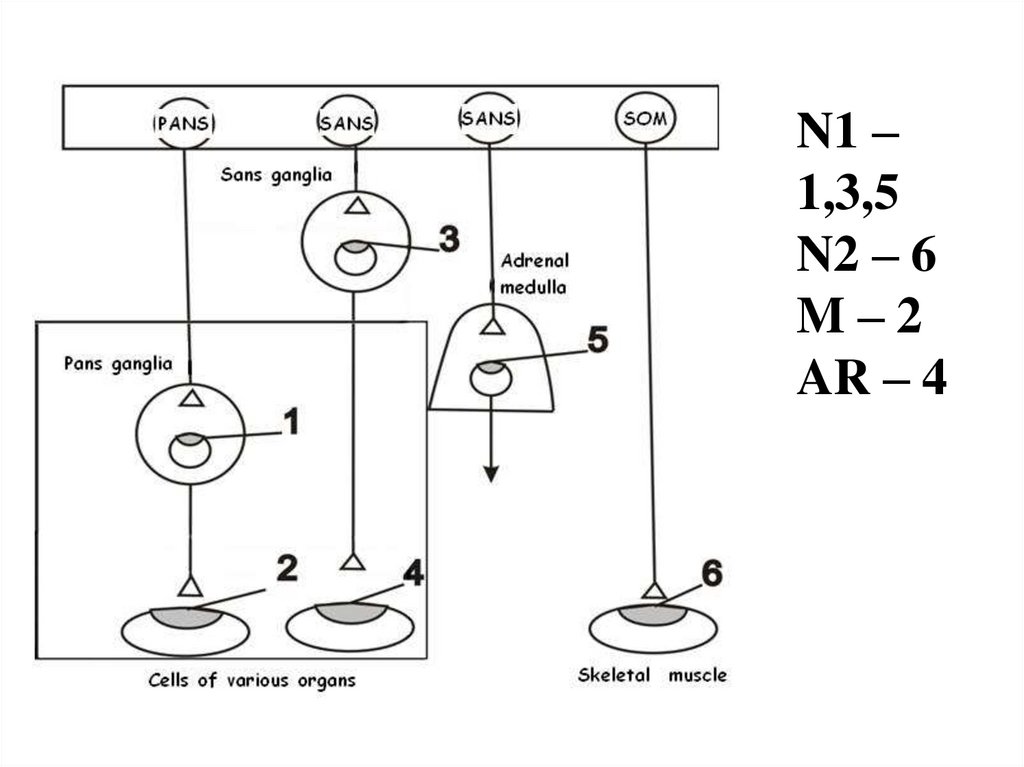
N1 –1,3,5
N2 – 6
M–2
AR – 4
4.
• M-cholinoblockers block the peripheral Mcholinoceptors of the effectors' cellmembranes (on the terminals of
postganglionic cholinergic fibers) and Mcholinoceptors in the CNS. Among these
drugs there are:
1.Preparations of plant origin:
A. Herbal medicines:
Tincture of belladonna
Extract of belladonna (tablets “ Besalol”,
suppositories “ Anusol”),
5.
B. Alkaloids: Atropine, Scopolamine,Platyphilline
2.Semisynthetic derivatives:
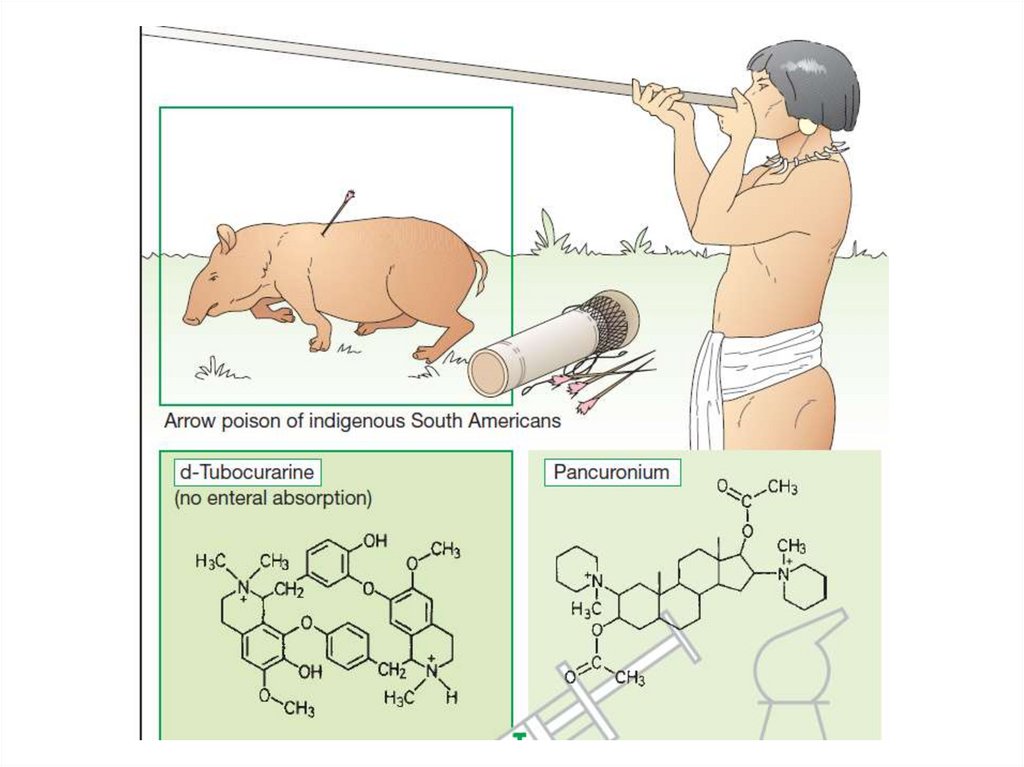
Homatropine, Tiotropium bromide,
Ipratropium bromide
3. Synthetic drug: Tropicamide,
Metocinium iodide,
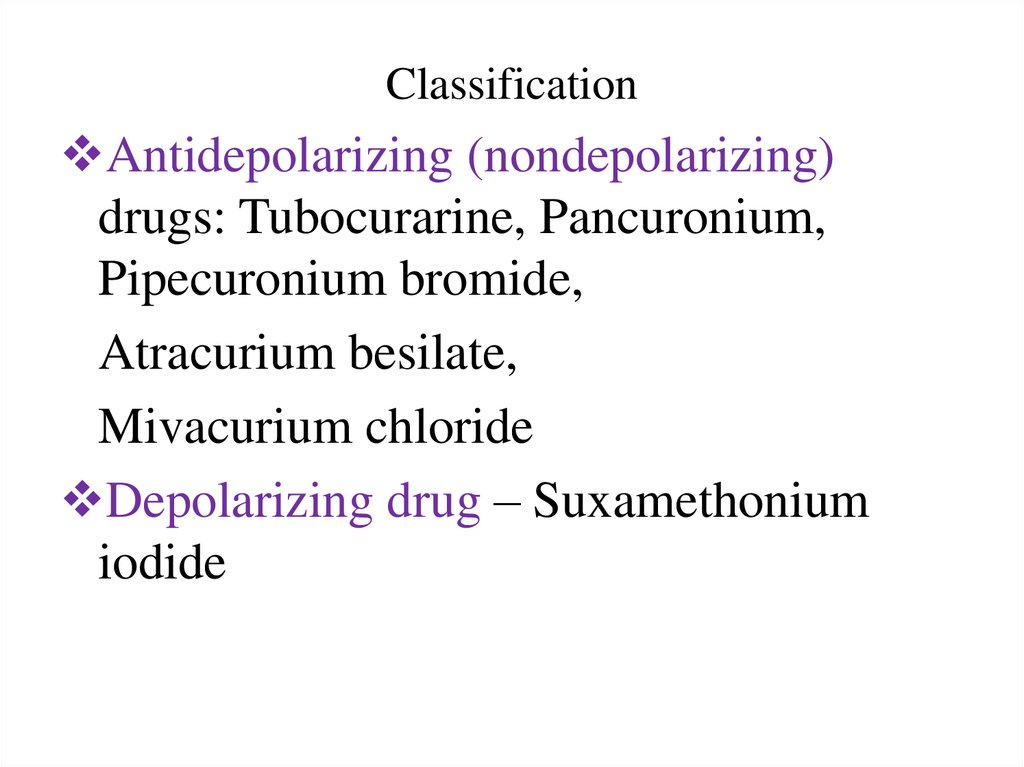
Pirenzepine hydrochloride,
4. Antiparkinsonian: Trihexyphenidyl
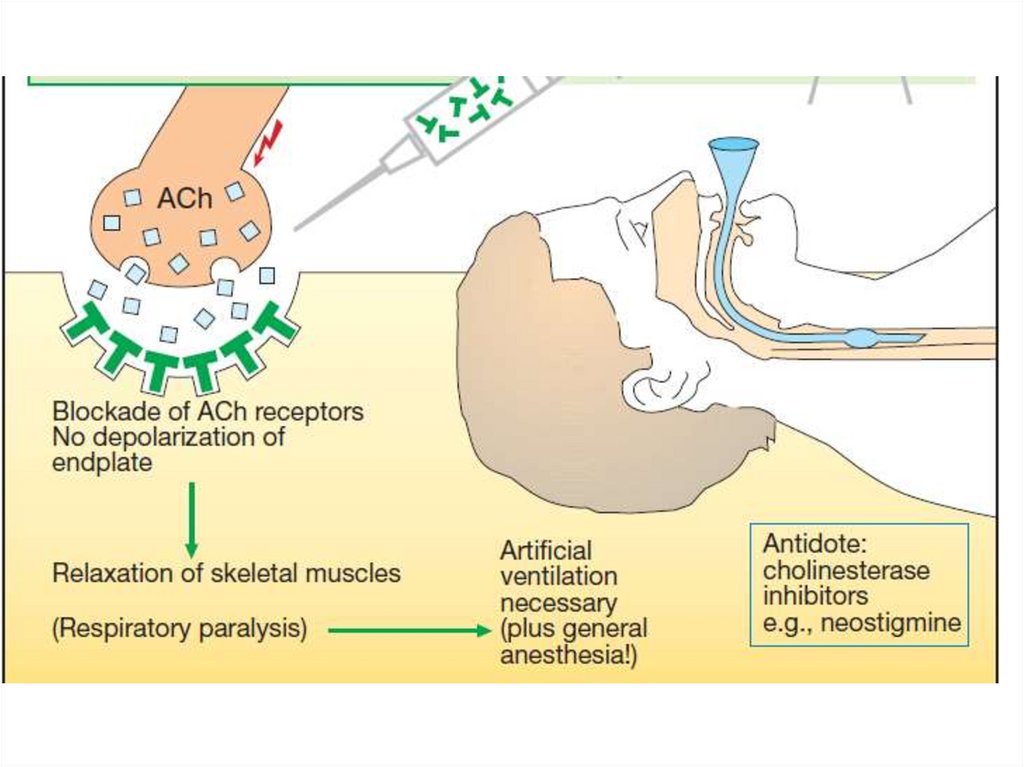
6.
Alkaloids are tertiary amines and passwell through the BBB, synthetic drugs
(Quaternary ammonium compounds) pass
poorly.
M-cholinoblockers block receptors
differently.
• Selective blocker of M1-cholinoceptors
of stomach – pirenzepin
• N, m blocker - Platyphylline
• Non-selective blockers – all other drugs
7.
8.
CNS• Atropine stimulates many medullary
centres —vagal, respiratory, vasomotor.
• It depresses vestibular excitation and has
antimotion sickness property. It suppresses
tremor and rigidity of parkinsonism.
• High doses cause cortical excitation,
restlessness, disorientation, hallucinations
and delirium followed by respiratory
depression and coma.
9.
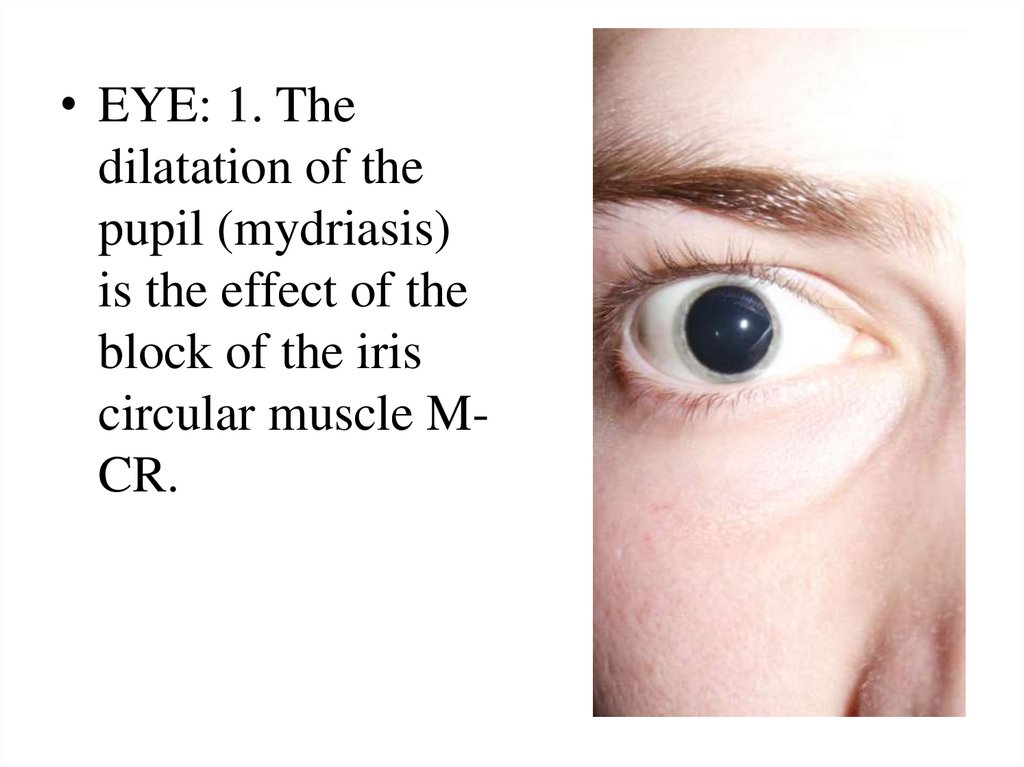
• EYE: 1. Thedilatation of the
pupil (mydriasis)
is the effect of the
block of the iris
circular muscle MCR.
10.
2. The fluid outflow from the anteriorchamber of the eye is decreased and
intraocular pressure can increase (especially
in glaucoma).
3. Blocking M-CR of the ciliary muscle leads
to its relaxation, which results in an increase
of the ciliary zonule (ligament of Zinn)
tension and a reduction of lens curvative.
Accommodation paralysis occurs and the
eye become adjusted to the distant point of
vision.
11.
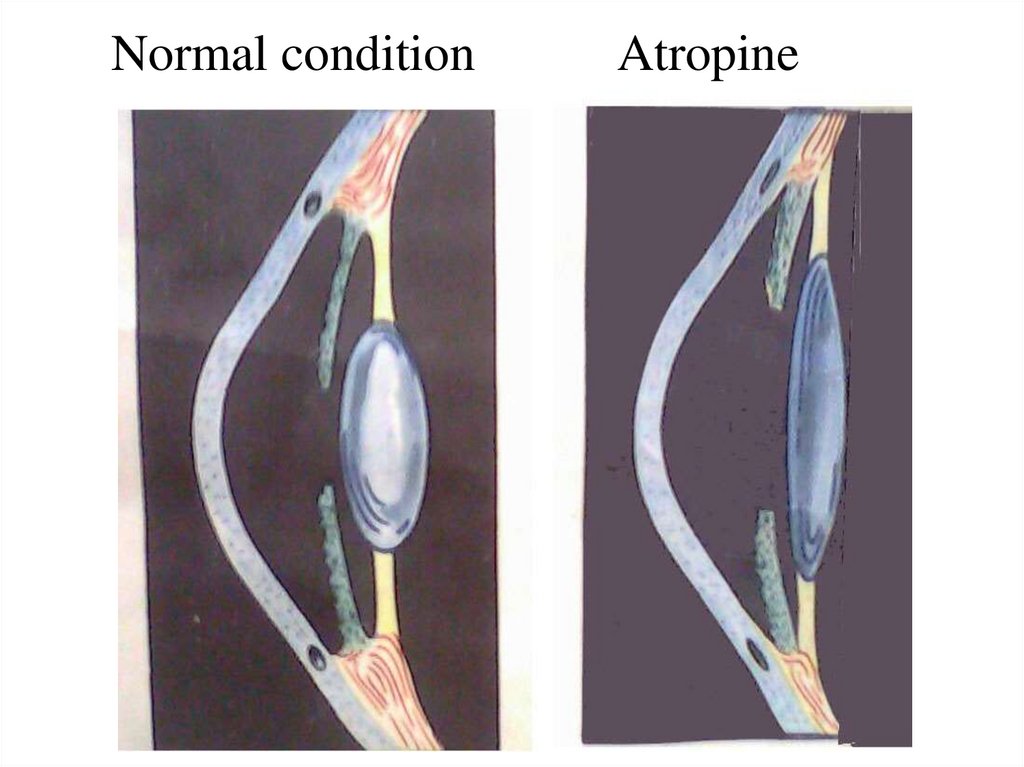
Normal conditionAtropine
12.
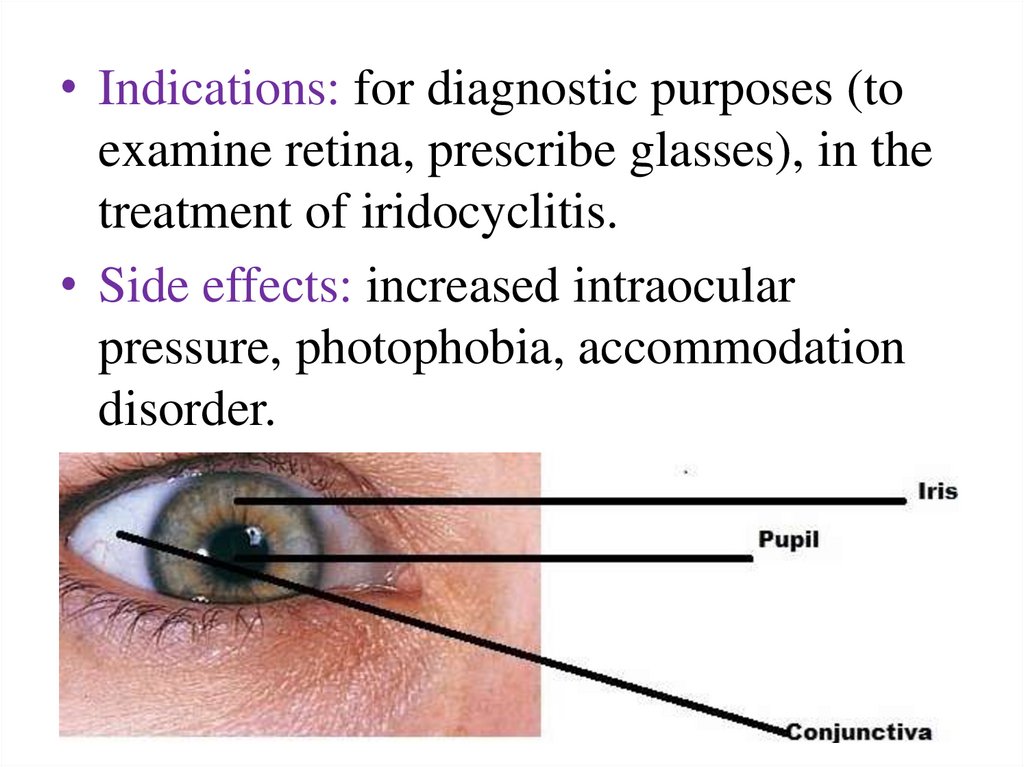
• Indications: for diagnostic purposes (toexamine retina, prescribe glasses), in the
treatment of iridocyclitis.
• Side effects: increased intraocular
pressure, photophobia, accommodation
disorder.
13.
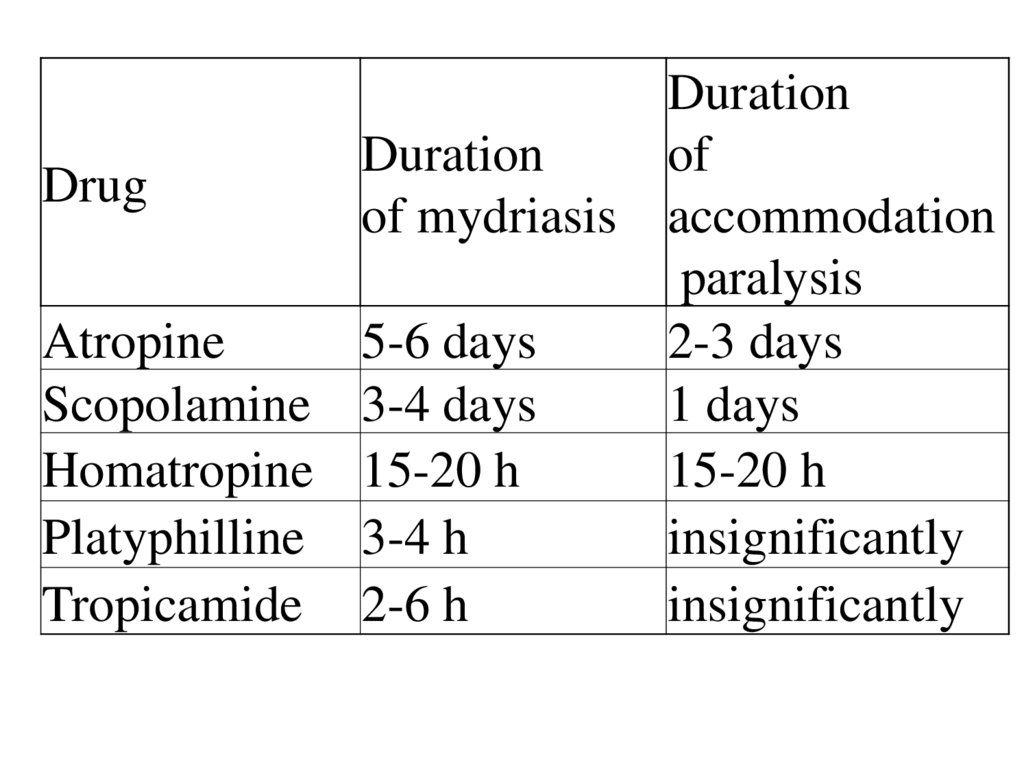
DurationDuration
of
Drug
of mydriasis accommodation
paralysis
Atropine
5-6 days
2-3 days
Scopolamine 3-4 days
1 days
Homatropine 15-20 h
15-20 h
Platyphilline 3-4 h
insignificantly
Tropicamide 2-6 h
insignificantly
14.
• Heart. The main effect is tachycardia. Itis due to blockade of M2 receptors on the
SA node through which vagal tone
decreases HR. Atropine facilitates A-V
conduction.
• Smooth muscles. A. decreases muscular
tone of the gastrointestinal tract, bile
ducts, gallbladder, bronchi, bladder.
15.
• Exocrine glands. It inhibits glandularsecretion: bronchial, nasopharyngeal,
digestive (especially salivary), sweat and
lacrimal. It leads to a dryness of oral
mucous membrane (xerostomia), skin
(xerodermia) and a change in the timbre
of the voice. A decrease in sweating may
leads to a rise in body temperature.
16.
Indications:Bradyarrhythmia, atrioventricular block;
Stomach and duodenal ulcer, hyperacid
gastritis; acute pancreatitis;
Spastic pain or colic (intestinal, hepatic, renal);
Bronchial asthma, bronchospasm;
Hypersalivation (in Parkinsonism, poisoning
with heavy metals salts);
Overdose of cholinomimetics,
anticholinesterase drugs, cardiac glycosides
17.
• Wide use of atropine for premedicationbefore surgical interventions is linked to its
ability to inhibit secretion of salivary,
nasopharyngeal
and
thracheobrochial
glands. Moreover, blocking MCR of the
heart (vagolytic action), A. prevents
negative effects on the heart, including the
possibility of its reflectory arrest (for
example, in administration of inhalation
anesthetics that irritate the upper respiratory
tract).
18.
Side effects of atropine:Dryness of oral mucosa,
Accommodation disorder,
Tachycardia,
An increase in intraocular pressure,
Constipation,
Urination difficulty.
19.
Symptoms of atropine poisoning (usually children):Dryness of the mucous membranes of the
mouth and nasopharynx, difficulty with
swallowing and speech,
dry skin, rise of temperature,
dilated pupils, photophobia,
motor and verbal agitation, impairment of
memory and orientation, hallucinations
(acute psychosis).
Help: anticholinesterase drugs
20.
Scopolamine more strongly affects theeyes and the secretion of a number of
excretory glands. It causes calming,
drowsiness, sleep. It inhibits the
extrapyramidal system and transmission
from
pyramidal
pathways
to
motorneurons.
It can be used for the prevention of
seasickness and airsickness and for
Parkinson treatment.
21.
• Platyphillinehas
moderate
ganglioblocking and direct myotropic
spasmolytic (papaverine-like) actions. It
inhibits the vasomotor center.
• It is used as a spasmolytic drug in spasm
of the stomach, intestine, biliary ducts,
gallbladder and uretes. It is administered
to reduce pathologically increased tone
of cerebral and coronary vessels.
22.
• Metocinium iodide passes poorly throughthe blood-brain-barrier. It does not affect
the CNS and eye. It has more prominent
broncholytic effect.
• It is used as broncholytic in bronchial
asthma, biliary colic, for premedication in
anesthesiology (reduces secretion of the
bronchial glands, blocks transmission from
the vagus nerve to the heart and bronchi).
23.
Ipratropium, Tiotropium, TroventolumThey are administered via inhalation.
They dilate the bronchi and are used for the
treatment of bronchial asthma.
24.
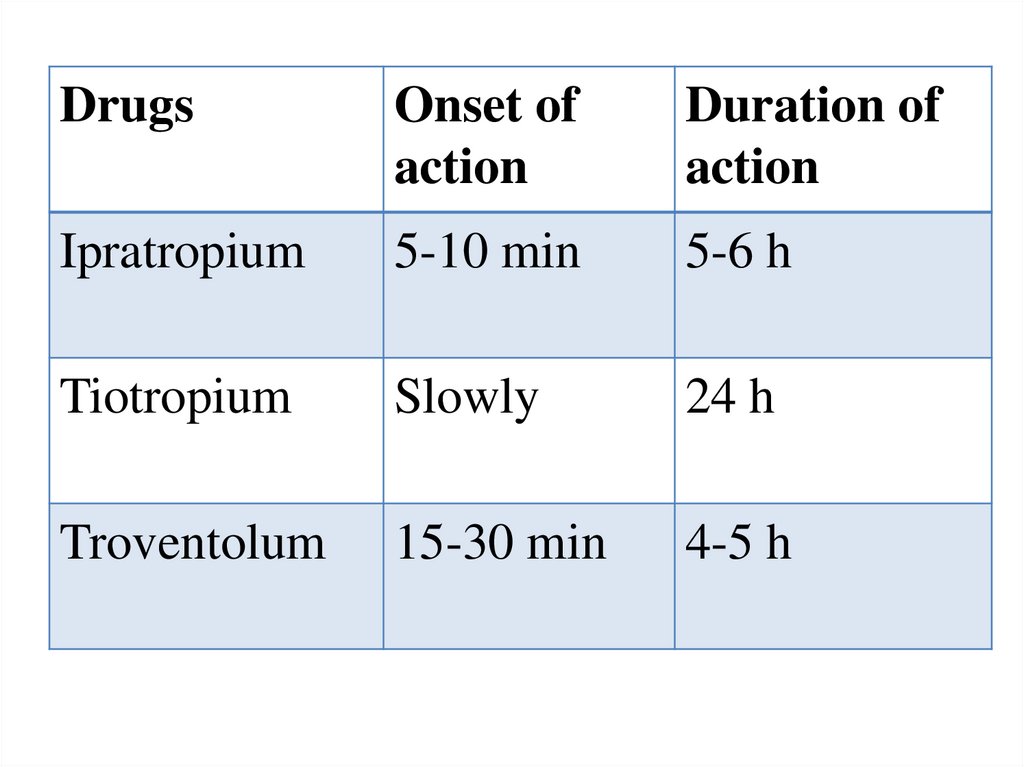
DrugsOnset of
action
Duration of
action
Ipratropium
5-10 min
5-6 h
Tiotropium
Slowly
24 h
Troventolum
15-30 min
4-5 h
25.
• Pirenzepineblocks
M1-CR
of
the
enterochromaffin cells and parasympathetic
ganglia of the stomach. It suppresses basal and
induced secretion of hydrochloric acid and
pepsinogen, causes a decrease in gastrin release
in response to food.
• It increases the resistance of gastric mucosal
sells to injury (gastroprotective effect).
• P. causes a slight decrease in salivary glands
secretion.
• It is used for the treatment of gastric and
duodenal ulcers.
26.
• Ganglionic blockers block sympathetic andparasympathetic ganglia, N-CR of the adrenal
medulla and carotid body.
Classification
Bis-Quaternary ammonium salts do not penetrate
the BBB
1. Short-acting drugs (5-20 minutes): Trepirium
iodide
2. Average duration (3-4 hours): Azametonium
bromide, Hexamethonium benzolsulfonate
3. Long-acting (tertiary amines): Pachycarpine (68 hours)
27.
• They dilate arterial and venous vessels,decrease blood pressure, reduce preload
and postload of the heart, improve blood
circulation in organs (lower limbs),
improve tissue trophism .
• They reduce smooth muscle tone
(intestine, bronchi, except myometrium),
secretion of exocrine glands (salivary,
gastric). But they can increase tone of
uterine and stimulate labor.
28.
Indications for the use:Obliterating endarteritis, pulmonary edema,
arterial embolism, hypertensive crisis.
Short-acting drugs can be used for controlled
hypotension during operation. They are
administered IV drip, dilate vessels, decrease
arterial pressure and reduce hemorrhage during
thyroidectomy and mastectomy. In neurosurgery
they reduce the possibility of the development of
brain edema.
Spastic pain (colic), bronchospasm, gastric and
duodenal ulcer.
29.
Side effects:Orthostatic collapse develops after an
abrupt change of the body’s position in
space. Marked and rapid decrease in the
arterial pressure develops after transition
from horizontal to vertical position.
Syncope.
Constipation, urinary retention.
Accommodation disorder, mydriasis.
Dysarthria, dysphagia.
30.
• Drugs blocking neuromuscular transmission(neuromuscular relaxants, peripheral
muscles relaxants)
• They inhibit neuromuscular transmission on
the level of postsynaptic membrane,
interacting with N-cholinoceptors of the
endplates.
• Curare was the first muscle relaxant. Its extract
was obtained from plants in South America
and used as an arrow poisoning.
31.
32.
N1 –1,3,5
N2 – 6
M–2
AR – 4
33.
ClassificationAntidepolarizing (nondepolarizing)
drugs: Tubocurarine, Pancuronium,
Pipecuronium bromide,
Atracurium besilate,
Mivacurium chloride
Depolarizing drug – Suxamethonium
iodide
34.
Duration of action:Short-acting:
Mivacurium chloride (15 min),
Suxamethonium iodide (5-8 min)
Average duration:
Atracurium besilate(15-35 min)
Long-acting:
Pipecuronium bromide (50-120 min)
35.
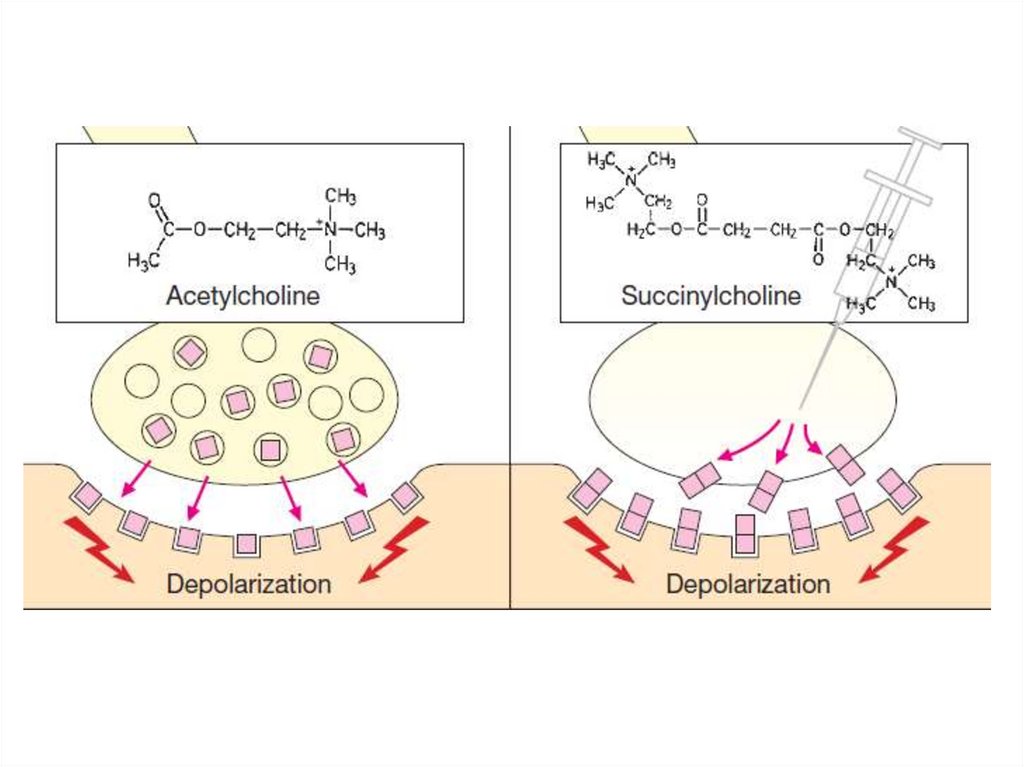
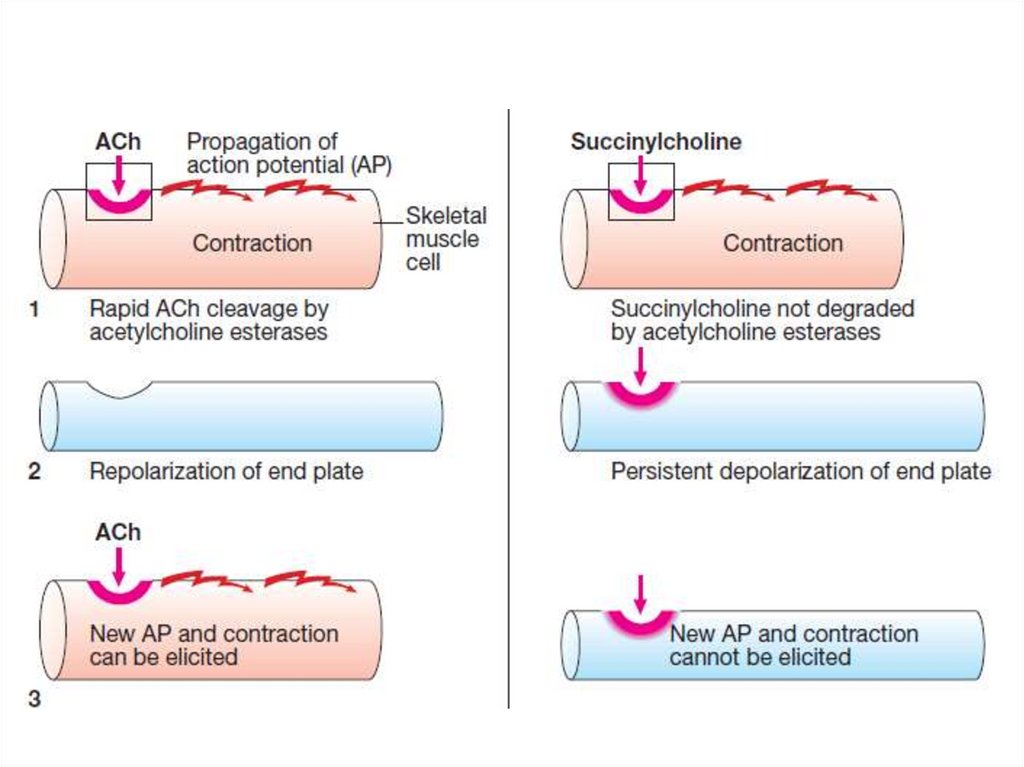
Antidepolarizing drugs block N-ChR and preventdepolarizing effect of acetylcholine. They act
competitive. If the concentration of acetylcholine
in the area of block is increased significantly this
will lead to restoration of the neuromuscular
transmission.
Depolarizing drug excite N-ChR and causes
steady depolarization of the postsynaptic
membrane. In the beginning, depolarization
development is manifested by muscular
fasciculations. Soon after a myoparalytic effect
develops.
36.
37.
38.
39.
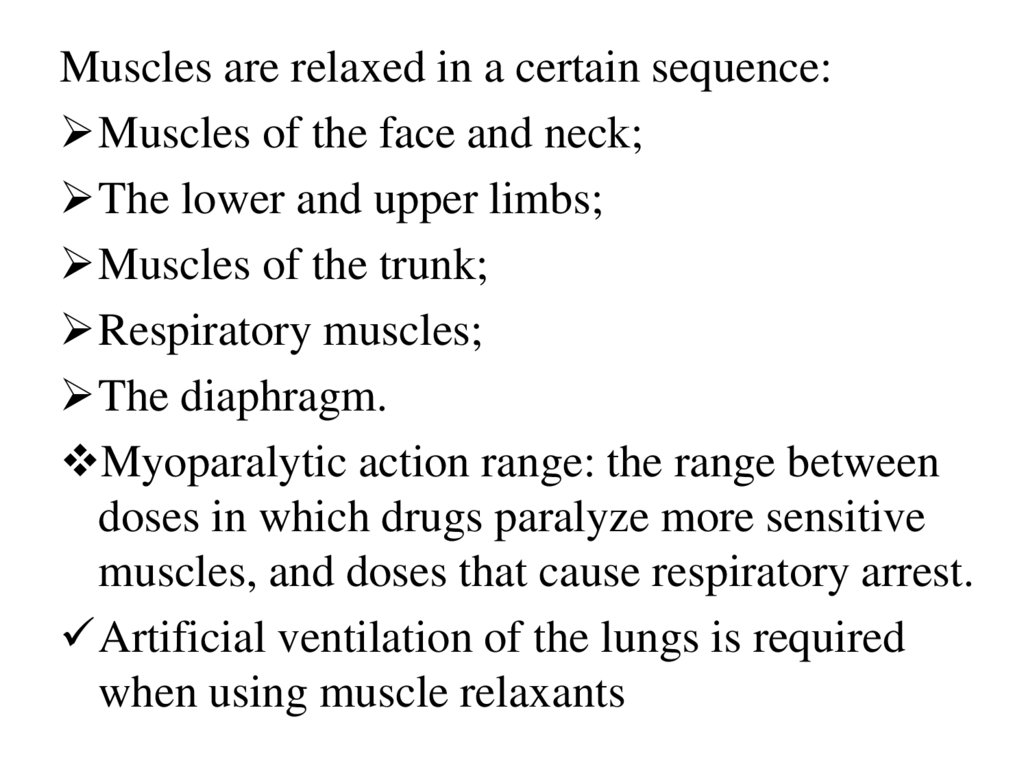
Muscles are relaxed in a certain sequence:Muscles of the face and neck;
The lower and upper limbs;
Muscles of the trunk;
Respiratory muscles;
The diaphragm.
Myoparalytic action range: the range between
doses in which drugs paralyze more sensitive
muscles, and doses that cause respiratory arrest.
Artificial ventilation of the lungs is required
when using muscle relaxants
40.
The sequence shutdown of skeletal muscle duringintravenous curare-like drugs
41.
Antagonists:Antagonists of the antidepolarizing drugs
are anticholinesterase drugs (Neostigmine,
Galanthamine).
The action of depolarizing drug
(suxamethonium) can be reversed by the
administration of fresh citrated blood,
containing plasma cholinesterase, which
hydrolyzes suxamethonium.
42.
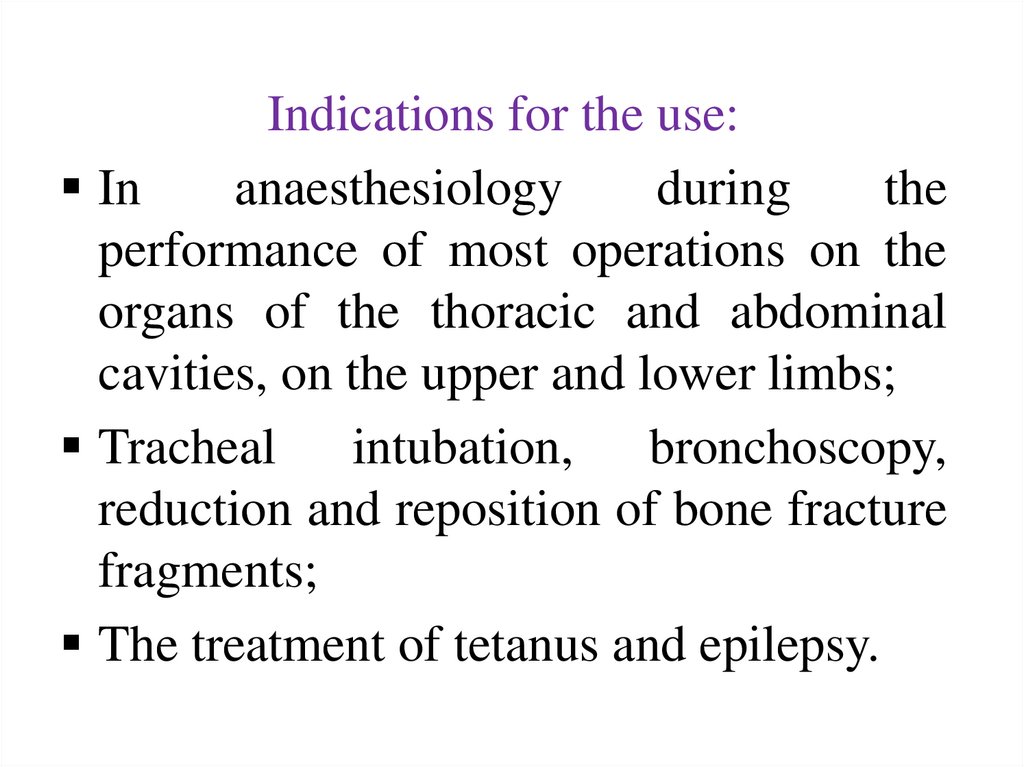
Indications for the use:In
anaesthesiology
during
the
performance of most operations on the
organs of the thoracic and abdominal
cavities, on the upper and lower limbs;
Tracheal intubation, bronchoscopy,
reduction and reposition of bone fracture
fragments;
The treatment of tetanus and epilepsy.
43.
Side effects:Tachycardia (pancuronium), fluctuations
in blood pressure,
Allergic reactions,
Arrhythmia, increase in intraocular
pressure, muscular pains, long-term
apnoea (suxamethonium).
44.
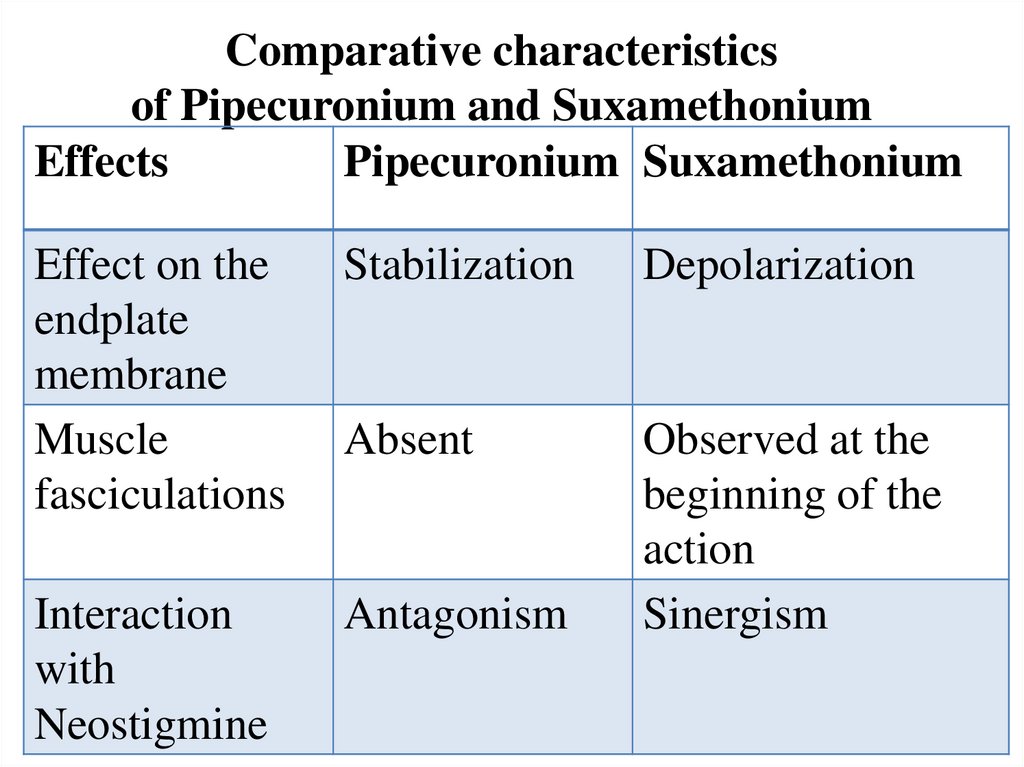
Comparative characteristicsof Pipecuronium and Suxamethonium
Effects
Pipecuronium Suxamethonium
Effect on the
endplate
membrane
Muscle
fasciculations
Stabilization
Depolarization
Absent
Interaction
with
Neostigmine
Antagonism
Observed at the
beginning of the
action
Sinergism










 medicine
medicine








