Similar presentations:
What is infection
1.
LESSON № 132. WHAT IS INFECTION?
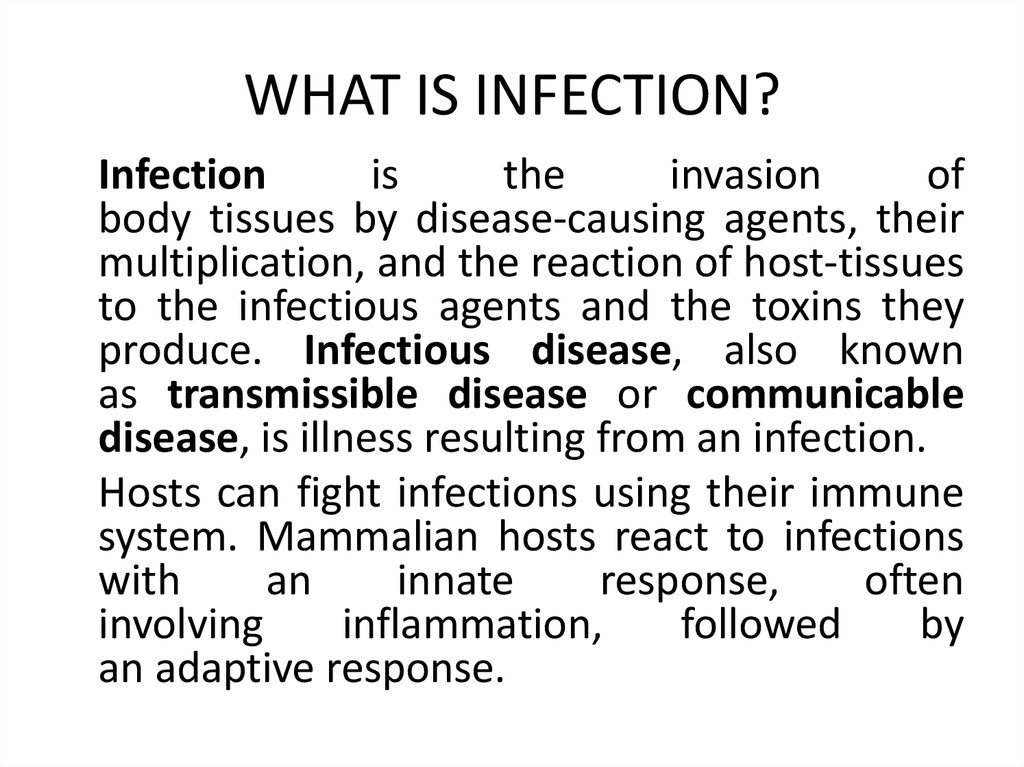
Infectionis
the
invasion
of
body tissues by disease-causing agents, their
multiplication, and the reaction of host-tissues
to the infectious agents and the toxins they
produce. Infectious disease, also known
as transmissible disease or communicable
disease, is illness resulting from an infection.
Hosts can fight infections using their immune
system. Mammalian hosts react to infections
with
an
innate
response,
often
involving
inflammation,
followed
by
an adaptive response.
3. WHAT CAUSES INFECTIONS?
Infections are caused by infectiousagents including
Bacteria
Viruses
Fungi (ringworm)
Protozoa
Macroparasites (nematodes, tapeworms,
helminths)
4.
5. PROPERTIES OF INFECTIOUS AGENTS
PathogenicityVirulence
Specificity
Organotropicity
6. PATHOGENICITY
Pathogenicity is a specific sign of the pathogen,its potential to cause a specific infectious
process under favorable conditions. On this
basis, all states of microbes are subdivided into
pathogenic, opportunistic and saprophytes.
Pathogenicity and virulence are different
concepts. A microorganism is considered
virulent if it, when introduced into the animal's
organism, even in small doses, causes the
development of an infectious process.
7. VIRULENCE
Virulenceis
the
degree
of
pathogenicity
of
a
particular
microorganism, i.e. this is an
individual characteristic. Virulence is a
quantity that is measured (e.g.,
minimum lethal dose DLM, median
lethal dose LD50).
8. SPECIFICITY
Each infectious disease causes a specificpathogen. So, the causative agent of plague
causes plague, cholera - cholera, etc. Infections
(for
example,
purulent-inflammatory
processes) caused by various microbes are
known. On the other hand, one causative agent
(for example, streptococcus) is capable of
causing various lesions.
9. ORGANOTROPICITY
Organotropicity is the defeat ofcells, tissues and organs that are
most suitable for their biochemical
properties for life support of this
type of microorganism.
10. VIRULENCE FACTORS
1. Adhesion to cellsMany bacteria for infection of
certain cells of the body, for
example,
intestinal
epithelium should attach to
them. It was found that a
large number of host cell
molecules, in particular, and
the receptors of bacteria
(proteins of the outer
bacterial membrane) are
involved in this process.
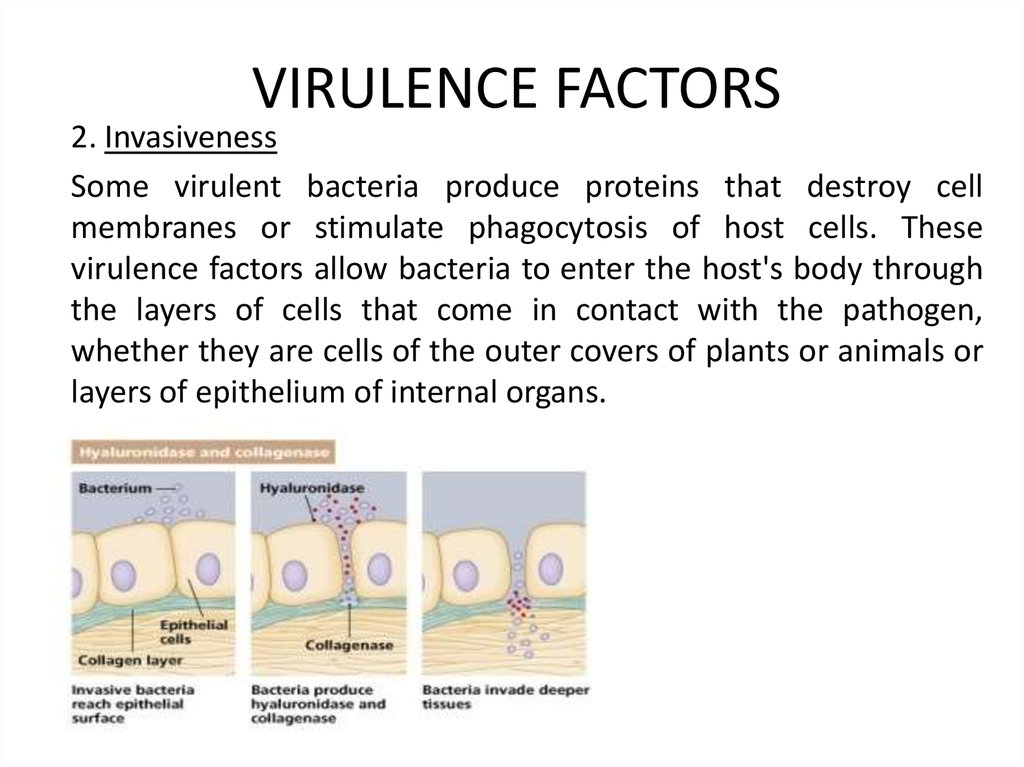
11. VIRULENCE FACTORS
2. InvasivenessSome virulent bacteria produce proteins that destroy cell
membranes or stimulate phagocytosis of host cells. These
virulence factors allow bacteria to enter the host's body through
the layers of cells that come in contact with the pathogen,
whether they are cells of the outer covers of plants or animals or
layers of epithelium of internal organs.
12. VIRULENCE FACTORS
3. Colonization is the process ofmultiplication of microbes at the site of
adhesion. Colonization provides the
accumulation of microorganisms to such
a critical concentration that can cause a
pathological effect.
13. VIRULENCE FACTORS
4. Suppression of the immune responseMany bacteria release virulence factors that inhibit
the body's immune system. For example, bacteria
secrete proteins that attach to host antibodies.
Another type of substance that inhibits the immune
response is the polysaccharide capsule surrounding
the cell. These polysaccharides complicate
phagocytosis of bacteria by specialized cells of the
immune system (macrophages) and lymphocytes.
14. VIRULENCE FACTORS
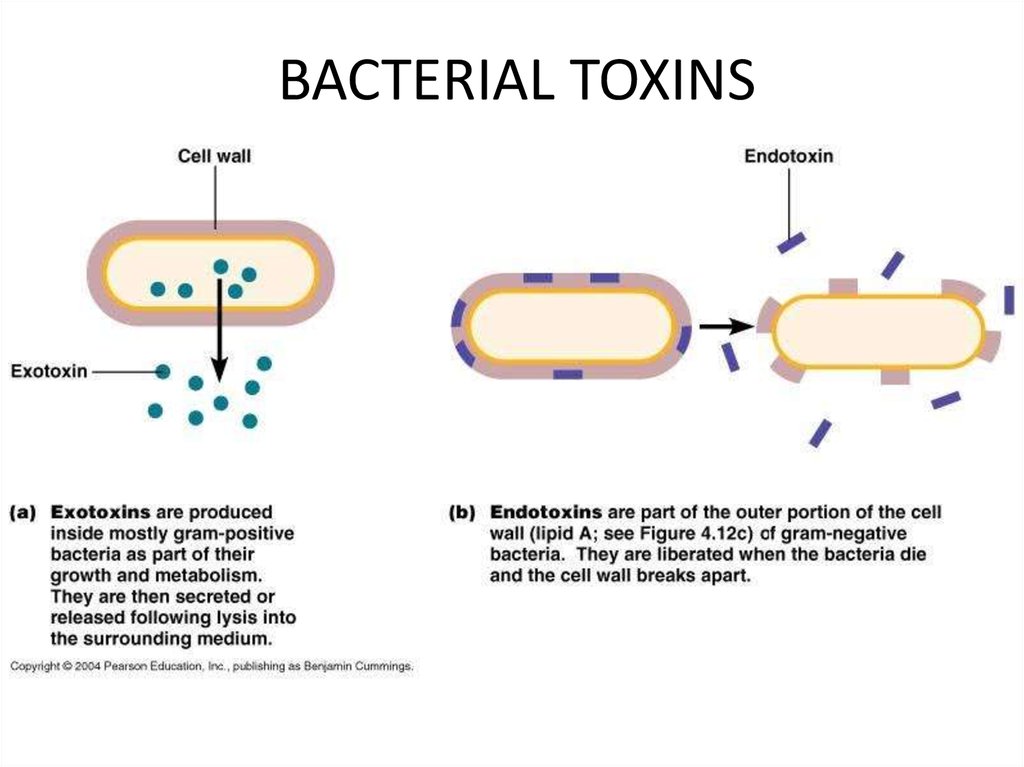
5. ToxinsMany virulence factors are proteins that the
pathogen produces and then secretes into the
environment and which causes damage to the host
tissues. For example, with food poisoning it is the
toxins that cause the symptoms of the disease.
15. BACTERIAL TOXINS
16.
17.
18. FORMS OF INFECTION PROCESSES
Infectious diseaseBacteriocarrier
Chronic (presence of
pathogens for several
months or even years)
Transitory (short-term
(most often - once)
excretion of the pathogen
in the absence of clinical
manifestations of the
disease)
Sharp (a consequence of a
recent illness)
19. COMMON ORAL INFECTIONS
GingivitisDental Caries
Periodontal Disease
Canker Sores
Oral Herpes
20. REASONS OF ORAL INFECTIONS
injuriesa lack of vitamins and trace elements
a general decrease in immunity
allergic reactions
infections
the presence of tartar deposits
poor hygienic condition of the cavity
21. BIOLOGICAL RESEARCH METHODS
Biological research methods are aimed atdetermining the presence of pathogen toxins in
the test material and on the detection of the
causative agent. Methods include infecting
laboratory animals with the test material,
followed by isolation of a pure pathogen culture
or establishing the presence of a microbial toxin
and its nature. The method is highly sensitive, can
be used in the early stages of the disease, but is
not always available, expensive, long-lasting,
unsafe.
22. OBJECTIVES OF BIOLOGICAL METHOD
1. Diagnosis of infectious diseases.2. Identification of pure culture.
3. Definition of virulence.
4. Isolation and identification of exotoxins.
5. Cultivation of viruses.
6. Reception of immunopreparations.
7. Checking the harmlessness and effectiveness of
medications (including chemotherapy drugs,
immunopreparations) and others.
23. STAGES OF BIOLOGICAL METHOD
1. Material intake.2. Material processing.
3. The choice of a laboratory animal.
4. Infection of animals by one of the methods.
5. Registration of signs of illness of the infected animal or its
death.
6. Intravital sampling of material from the animal and carrying
out bacteriological and serological studies, setting an allergic
test.
7. Autopsy, study of pathoanatomical and pathomorphological
pattern. Preparation of smears-prints from internal organs.
8. Identification of the selected culture.
9. Conclusion on the results of the study.
24. TASK 1 STAINING BY BURRY-HINS METHOD
The Burry-Hins method is used to color capsular bacteriaand is based on the fact that the capsule does not perceive
the dyes. The capsule is detected by negative contrasting
backgrounds over the Burry. For this, black mascara is
mixed into culture and dried. After that, for fixation in the
flame of the burner, stain the bodies of microbial cells
according to Hins – aqueous fuchsine for 1 minute and
rinse with water for 5-10 seconds.
NB! As a result, a colorless capsule and red microbial
bodies are clearly visible on a dark background.
25. TASK 1 STAINING BY BURRY-HINS METHOD
Klebsiella pneumonia.A smear of pure culture.
Burri-Hins staining
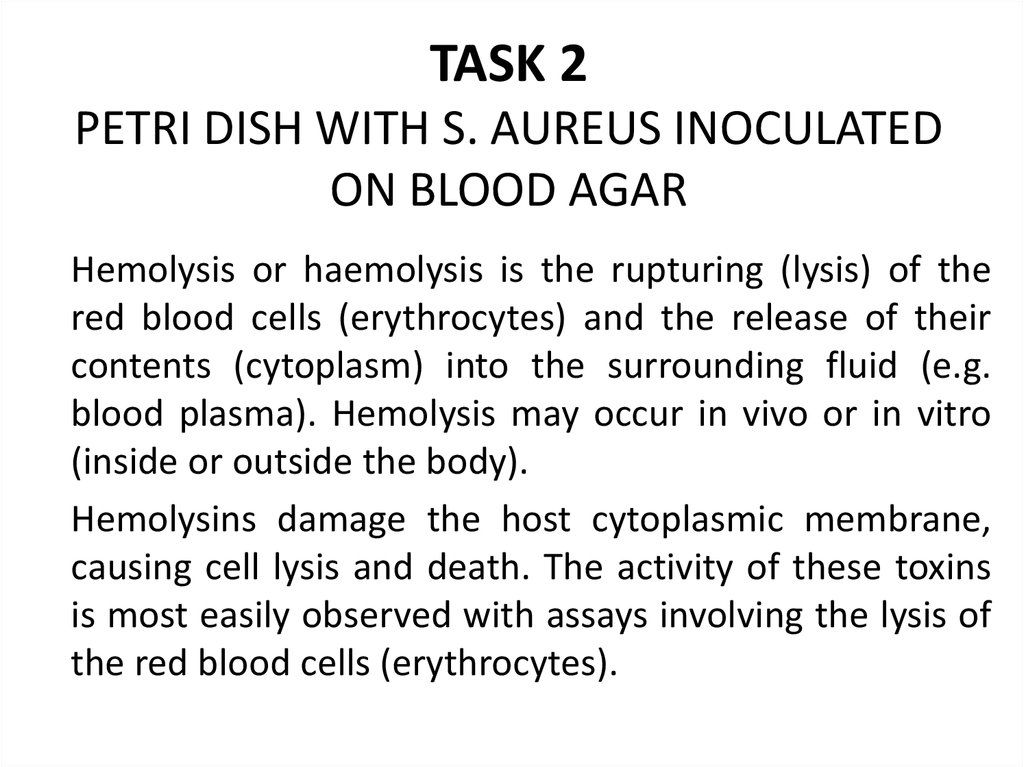
26. TASK 2 PETRI DISH WITH S. AUREUS INOCULATED ON BLOOD AGAR
Hemolysis or haemolysis is the rupturing (lysis) of thered blood cells (erythrocytes) and the release of their
contents (cytoplasm) into the surrounding fluid (e.g.
blood plasma). Hemolysis may occur in vivo or in vitro
(inside or outside the body).
Hemolysins damage the host cytoplasmic membrane,
causing cell lysis and death. The activity of these toxins
is most easily observed with assays involving the lysis of
the red blood cells (erythrocytes).
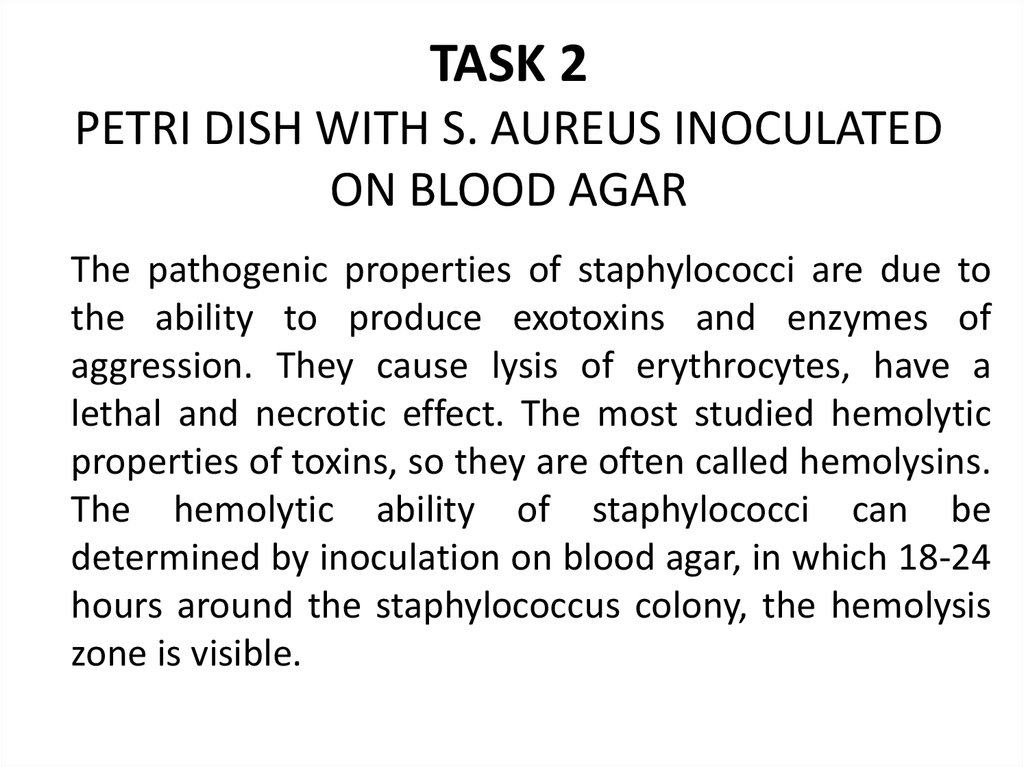
27. TASK 2 PETRI DISH WITH S. AUREUS INOCULATED ON BLOOD AGAR
The pathogenic properties of staphylococci are due tothe ability to produce exotoxins and enzymes of
aggression. They cause lysis of erythrocytes, have a
lethal and necrotic effect. The most studied hemolytic
properties of toxins, so they are often called hemolysins.
The hemolytic ability of staphylococci can be
determined by inoculation on blood agar, in which 18-24
hours around the staphylococcus colony, the hemolysis
zone is visible.
28. TASK 2 PETRI DISH WITH S. AUREUS INOCULATED ON BLOOD AGAR
32 1
1 – Staphylococcus
colonies
2 – Hemolysis
zones
3 – Blood agar
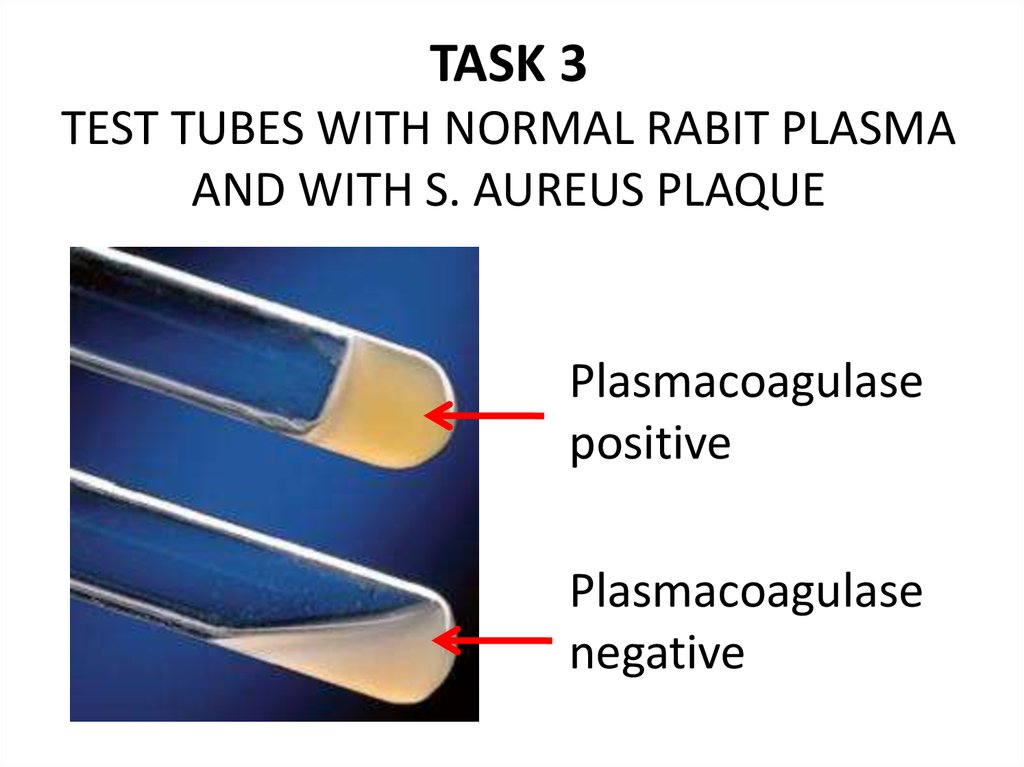
29. TASK 3 TEST TUBES WITH NORMAL RABIT PLASMA AND WITH S. AUREUS PLAQUE
Plasma-coagulant activity of the culture ischecked by inoculation in tubes with 0.5 ml of
citrated rabbit plasma at a dilution of 1: 4.
Pathogenic staphylococci coagulate the plasma
for 2-24 h under the conditions of a
thermostat. Accounting is performed after 24
hours by the formation of a small jelly-like clot
on the bottom of the tube.
30. TASK 3 TEST TUBES WITH NORMAL RABIT PLASMA AND WITH S. AUREUS PLAQUE
Plasmacoagulasepositive
Plasmacoagulase
negative
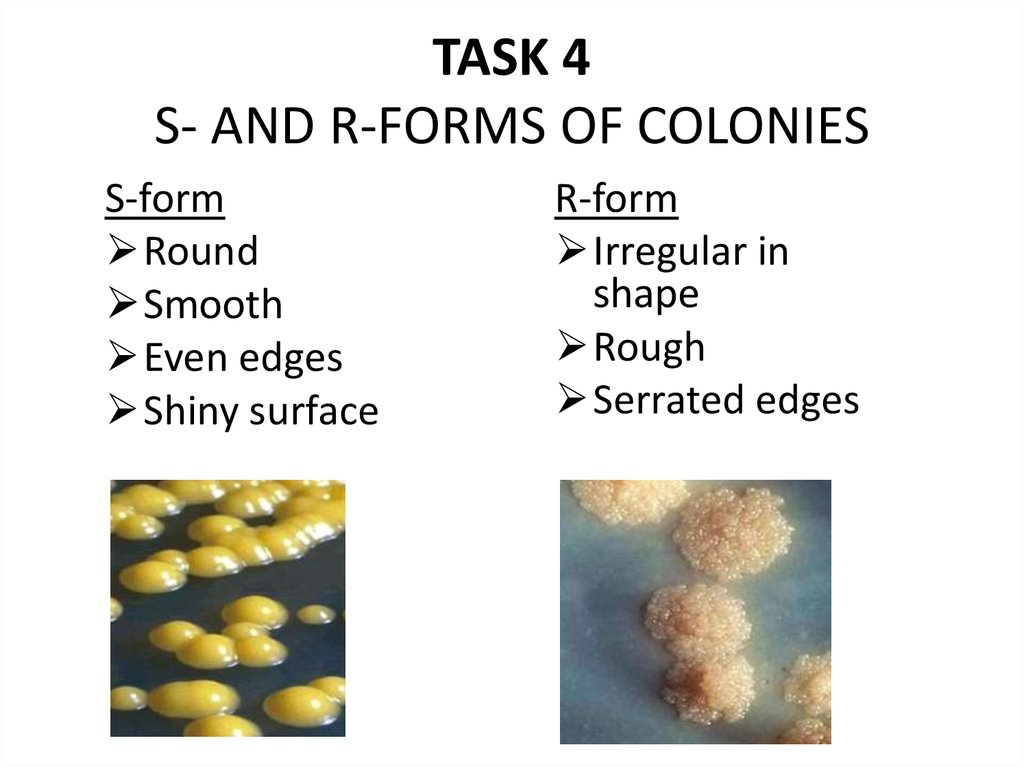
31. TASK 4 S- AND R-FORMS OF COLONIES
S-formRound
Smooth
Even edges
Shiny surface
R-form
Irregular in
shape
Rough
Serrated edges








 biology
biology