Similar presentations:
Atherosclerosis (1)
1. Atherosclerosis risk factors and prevention
ATHEROSCLEROSISRISK FACTORS AND PREVENTION
COMPLETED: SHERALI UULU AMANTUR 113
2. Definition
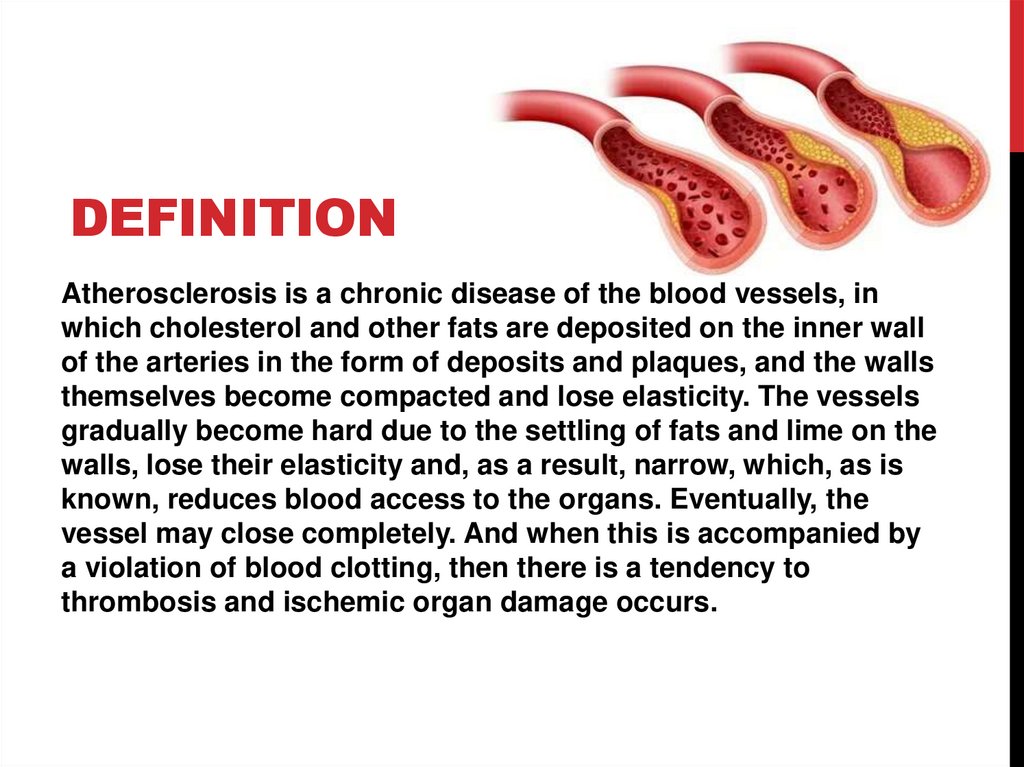
DEFINITIONAtherosclerosis is a chronic disease of the blood vessels, in
which cholesterol and other fats are deposited on the inner wall
of the arteries in the form of deposits and plaques, and the walls
themselves become compacted and lose elasticity. The vessels
gradually become hard due to the settling of fats and lime on the
walls, lose their elasticity and, as a result, narrow, which, as is
known, reduces blood access to the organs. Eventually, the
vessel may close completely. And when this is accompanied by
a violation of blood clotting, then there is a tendency to
thrombosis and ischemic organ damage occurs.
3. Risk factors
RISK FACTORSMaudited entities (which can be eliminated or Ne modifiable (change them you can't)
correct it)
1. Age: men over 45 years old and women
1. Lifestyle: physical inactivity, abuse of fatty, over 55 years old or with early menopause.
cholesterol-rich foods, personality and
behavior characteristics – stressful character 2. Male gender (men develop
atherosclerosis 10 years earlier than
type, alcohol abuse, smoking.
women).
2. Arterial hypertension, blood pressure
3. Family history of early atherosclerosis.
140/90 mmHg and above.
Familial hypercholesterolemia with a
3. Diabetes mellitus, fasting blood glucose
genetic basis. Myocardial infarction, stroke,
level more than 6 mmol/l.
and sudden death in the next of kin under
the age of 55 years for a man and 65 years
4. Hypercholesterolemia (blood cholesterol
for a woman.
level greater than 5 mmol / l).
5. Abdominal obesity (waist size in men is
more than 102 cm and more than 88 cm in
women).
4. Symptoms
SYMPTOMSVascular changes are more often localized in the aorta, heart,
brain, renal and limb arteries, more often in the lower ones.
The picture of the disease and the patient's complaints
depend on the lesion of certain arteries. So atherosclerosis
of the coronary arteries (heart vessels) is very often
manifested in the form of angina pectoris, a heart attack. The
pathological process, i.e., the disease, is based on a violation
of the correspondence between the heart's need for blood
supply and its actual implementation. Often, severe forms of
aortic atherosclerosis can be asymptomatic. The patient may
experience pressing or burning pains behind the sternum,
extending to both arms, neck, back, and upper abdomen. But
unlike angina, these pains last for a long time, then
increasing, then weakening.
5.
When the renal vessels are affected, severe arterial hypertension occurs.Atherosclerosis of the cerebral arteries is manifested by a decrease in working
capacity (especially mental), a decrease in memory, active attention, and rapid
fatigue. Over time, it appears dizziness, insomnia, patients become fussy,
obsessive, picky. Their intelligence decreases. A complication of atherosclerosis
of the cerebral arteries is a violation of cerebral circulation, hemorrhage (stroke),
thrombosis. Arteriosclerosis of the arteries of the extremities, more often the lower
ones, manifests itself in the calf muscles when walking ("intermittent lameness").
There are chilly and cold extremities. Thus, atherosclerosis leads to the
development of most modern "diseases of civilization".
If atherosclerotic changes are suspected, a specialist consultation is
indicated.: cardiologist (for ischemic heart disease); oculist (arteriosclerosis of the
fundus vessels); neurologist (cerebral arteriosclerosis); nephrologist
(arteriosclerosis of the renal arteries); vascular surgeon (arteriosclerosis of the
lower extremities, aorta). To clarify the degree of atherosclerotic lesion, additional
instrumental research methods may be prescribed: electrocardiography,
angiography, coronarography, intravascular ultrasound, duplex and triplex
scanning, magnetic resonance imaging, and others.
6. Prevention
PREVENTION• Anti-atherosclerotic diet.
Dietary recommendations are given to all patients, taking into
account the level of cholesterol and other risk factors: obesity,
arterial hypertension, diabetes mellitus. The diet should be
varied, in accordance with the patient's cultural traditions. The
caloric content of the daily diet should be sufficient to achieve
and maintain a normal weight.
Total fat intake should not exceed 30% of the caloric content of
the diet. It is recommended to limit the consumption of animal
fats (butter, cream, meat, lard), replacing them with vegetable
fats. The daily intake of fresh vegetables and fruits should be at
least 500 g per day.
It is recommended to consume lean meat and poultry without
skin, fermented dairy products, low-fat cottage cheese, grain
bread with bran, products enriched with unsaturated fatty acids
(sea and ocean fish-salmon, mackerel, tuna, etc.). Limit the
intake of table salt to 6 g per day, which corresponds to 1
teaspoon. Following a diet can reduce cholesterol levels by up
to 10%.
7. Prevention
PREVENTIONRefusal from drinking alcohol.
Safe for health alcohol consumption (no more than 20-30 ml of pure
ethanol per day for men and no more than 20 ml per day for women)
is allowed only for practically healthy individuals. Drinking 5 servings
of alcohol (60 g per day) increases the risk of cardiovascular
complications by 65%.
• Normalization of body weight indicators.
Overweight and obesity, especially abdominal (waist size in men is
more than 102cm and more than 88cm in women), increase the risk of
developing cardiovascular diseases. To reduce weight, an individual
diet is selected, taking into account age and concomitant diseases.
8. Prevention
PREVENTION• Physical properties loads in atherosclerosis.
Increase physical activity has a positive effect for patients
with atherosclerosis.
Patients without clinical manifestations of atherosclerosis
are shown to exercise for 30 minutes, daily. Patients with
cardiovascular diseases need a constant regime of dynamic
physical activity, taking into account the results of stress
tests. Walking, swimming, and moderate-intensity dancing
for 60-90 minutes per week are useful. Isometric (power)
loads are not allowed. It is recommended to use any
opportunities for physical activity: to walk, to use the car less
often.
9. Prevention
PREVENTION• Smoking cessation.
Smoking As a result of a sharp decrease in HDL (an antiatherogenic class of lipoproteins), pathological effects on the
vascular system, and violations of the rheological properties
of blood, it increases the risk of morbidity and mortality from
cardiovascular complications by 20%. Smokers are twice as
likely to develop an ischemic stroke as non-smokers.
10. Thanks for your attention
THANKS FOR YOURATTENTION
 medicine
medicine