Similar presentations:
Histology and Embryology can be divided into four main parts
1.
Histology and Embryology can be divided into four main parts:Divisions of Histology:
I) General Histology:
- Structure of the Cell and Histologic Techniques (Microscopes and Tissue Processing Techniques)
- Microscopic organization of 4 Basic Tissues: Epithelial Tissue, Connective Tissue and Specialized
Connective Tissues (Cartilage and Bone), Muscle Tissue and Nervous Tissue
II) Systemic Histology:
Histology of the all organs and systems
Divisions of Embryology:
III) General Embryology:
1. Subdivisions of the prenatal and postnatal periods
2. Male genital system and spermatogenesis
3. Female genital system and oogenesis/menstruel cycle
4. Transport of gametes, fertilization and first week of human development
5. Second week of human development
6. Third week of human development
7. Embryonic period and fetal period
8. Structure and functions of placenta and extraembryonic/fetal membranes: Chorion, Amnion, Yolk Sac,
Allantois and Umblical Cord
9. Multiple pregnancies
10. Birth Defects and Prenatal Diagnosis
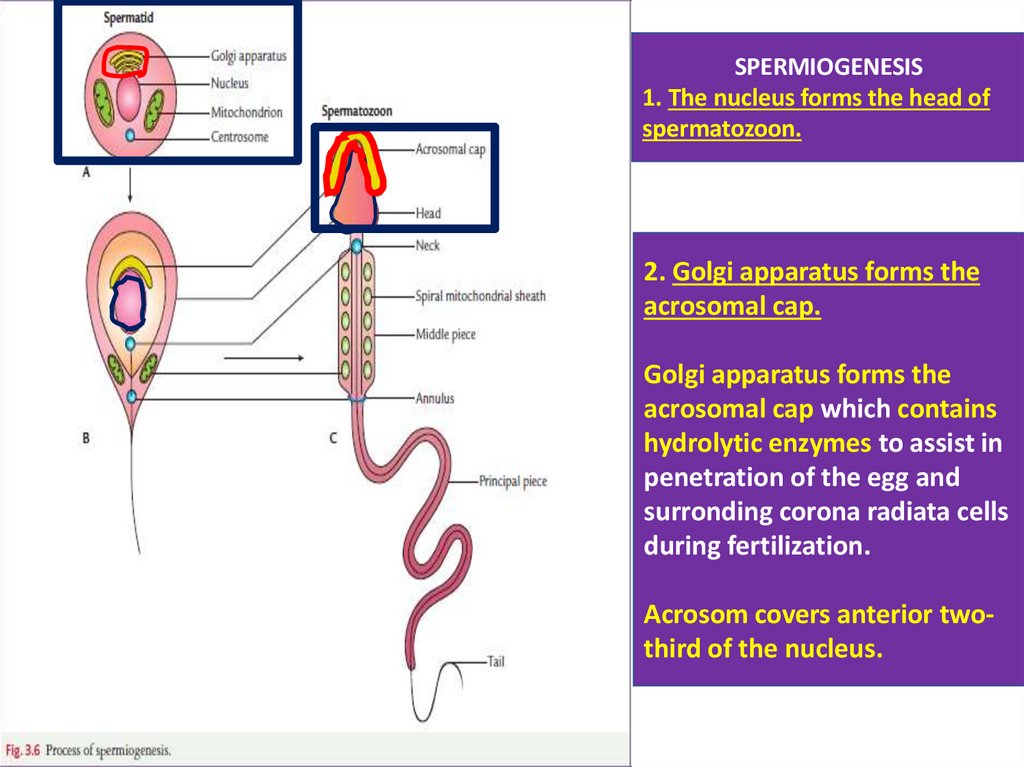
IV) Systems-Based Embryology:
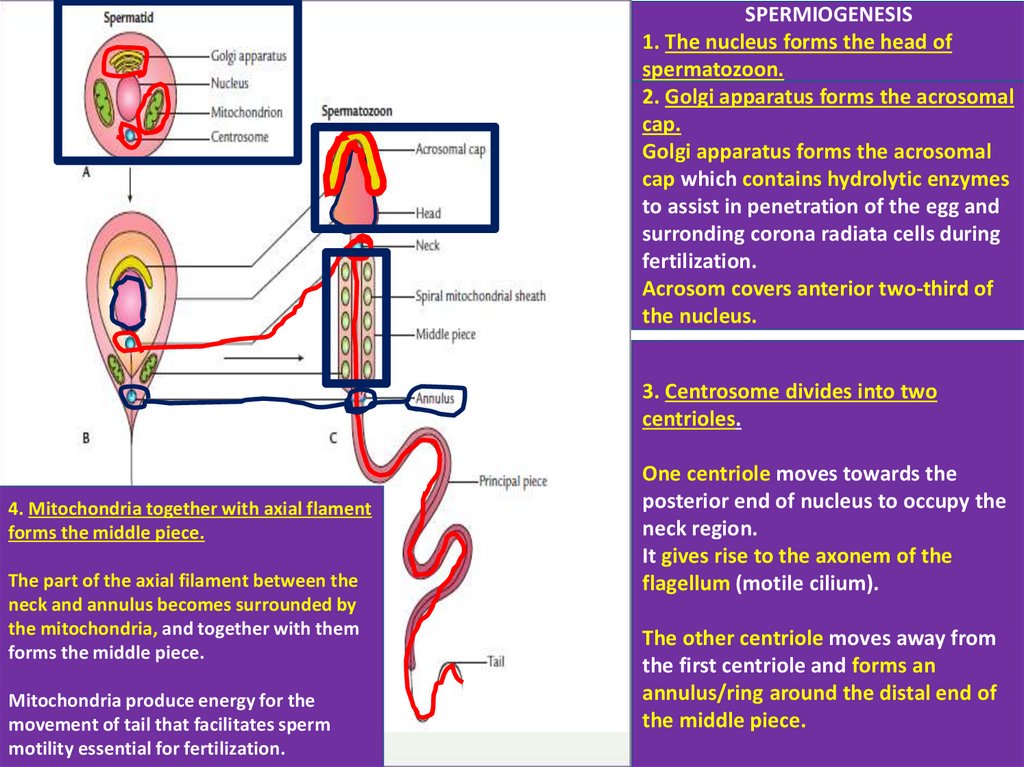
Development of all organ systems from trilaminar embryonic germ disc
2.
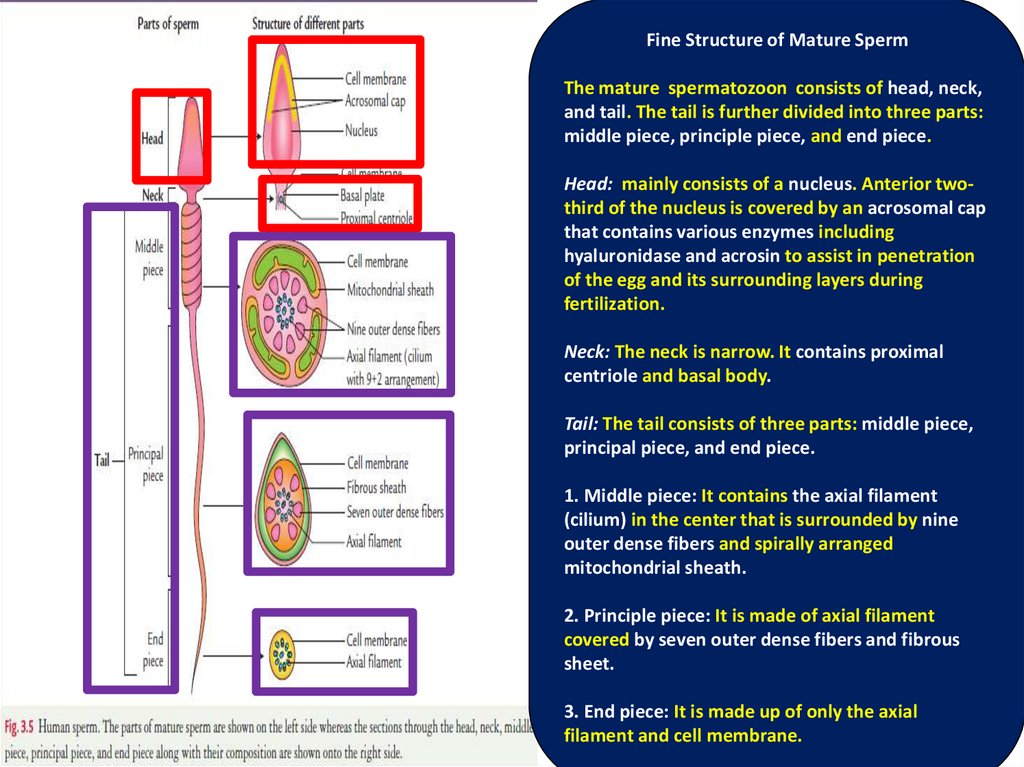
General Embryology Topics1. Subdivisions of the prenatal and postnatal periods
2. Male genital system and spermatogenesis
3. Female genital system and oogenesis/menstruel cycle
4. Transport of gametes, fertilization and first week of human development
5. Second week of human development
6. Third week of human development
7. Embryonic period and fetal period
8. Structure and functions of placenta and extraembryonic/fetal membranes: Chorion,
Amnion, Yolk Sac, Allantois and Umblical Cord
9. Multiple pregnancies
10. Birth Defects and Prenatal Diagnosis
3.
1. Subdivisions of the prenatal and postnatal periodsFrom the zygote to death, human life consists of two major periods:
I) Prenatal Period (Before birth or intrauterine life/IUL): It begins with single cell-the zygote and
culminates after 9 months.
II) Postnatal Period (After birth): It extends from birth to death.
Prenatal period (38-40 weeks: 266-280 days) is divided into three parts:
I) Pre-embryonic period: It extends from fertilization to the end of the second week.
II) Embryonic period: This period extends from beginning of the third week to the end of the eight week.
The living organism in this period is called the Embryo.
This period is also known organogenetic period (All organs and systems are formed in this period).
During this period a single cell called zygote is converted into a form that externally resembles with the
features of an adult individual (only 3 cm in length).
Embryonic period is also most risky and dangerous period of most affected by teratogens (Alcohol,
cigarette, some drugs, radiation and infections-TORCH).
Teratology is a branch of embryology that is concerned with the congenital anomalies or birth defects.
It deals with abnormal embryonic and fetal development.
III) Fetal Period: It extends from beginning of the ninth week (57th day) to birth.
The human being in this period is called the Fetus.
3
4.
Postnatal Period: from Birth – to Death1. Infancy period: from birth - to 1 year and newborn during this period is termed
infant-baby
The first four weeks of infancy period is called Neonatal period (0-1 month period).
The care of baby during the neonatal period is termed Neonatology.
2. Childhood period: from 2nd to 12th year
The medical subject dealing with care of children in health an disease is termed
pediatrics.
3. Puberty period: (Latin: pubertas, which means development of sex
characteristics): from 13th to 16th year
4. Adolescence period: Very rapid physical growth and sexual maturation, 17 - 18
year.
5. Adulthood period: (Latin: Adultus, which means grown up): from 19th to 60 year
6. Senility-Geriatry: from 60 – to death
5.
General Embryology Topics1. Subdivisions of the prenatal and postnatal periods
2. Male genital system and spermatogenesis
3. Female genital system and oogenesis/menstruel cycle
4. Transport of gametes, fertilization and first week of human development
5. Second week of human development
6. Third week of human development
7. Embryonic period and fetal period
8. Structure and functions of placenta and extraembryonic/fetal membranes: Chorion,
Amnion, Yolk Sac, Allantois and Umblical Cord
9. Multiple pregnancies
10. Birth Defects and Prenatal Diagnosis
6.
2. Male genital system and spermatogenesisI) Male reproductive system and histologic organization of the Testis:
* Capsule, septa and testicular lobules
* Fine structure of seminiferous tubule (where spermatogenesis takes place)
* Structure and Functions of Sertoli cells and Leydig cells
II) Common Ancestor Cells=PGCs (Primordial Germ Cells):
Their formation, their migration and their convertion to Spermatogonia
III) When and how spermatogenesis does begin:
Hypothalamo – Pituitary – Gonadal (Testicular) Axis (at puberty)
IV) Three stages of spermatogenesis:
Spermatogonial stage/Spermatocytogenesis, Meiosis stage, Spermiogenesis
V) Male Infertility and Semen Analysis (Sperm Analysis)
7.
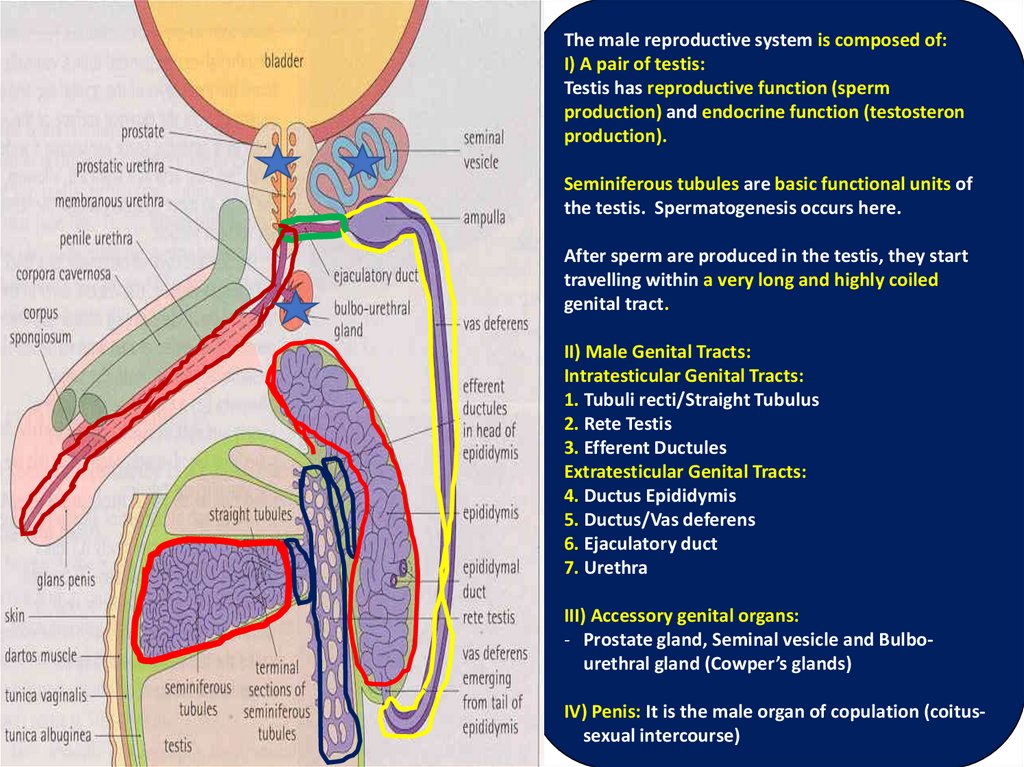
The male reproductive system is composed of:I) A pair of testis:
Testis has reproductive function (sperm
production) and endocrine function (testosteron
production).
Seminiferous tubules are basic functional units of
the testis. Spermatogenesis occurs here.
After sperm are produced in the testis, they start
travelling within a very long and highly coiled
genital tract.
II) Male Genital Tracts:
Intratesticular Genital Tracts:
1. Tubuli recti/Straight Tubulus
2. Rete Testis
3. Efferent Ductules
Extratesticular Genital Tracts:
4. Ductus Epididymis
5. Ductus/Vas deferens
6. Ejaculatory duct
7. Urethra
III) Accessory genital organs:
- Prostate gland, Seminal vesicle and Bulbourethral gland (Cowper’s glands)
IV) Penis: It is the male organ of copulation (coitus7
sexual intercourse)
8.
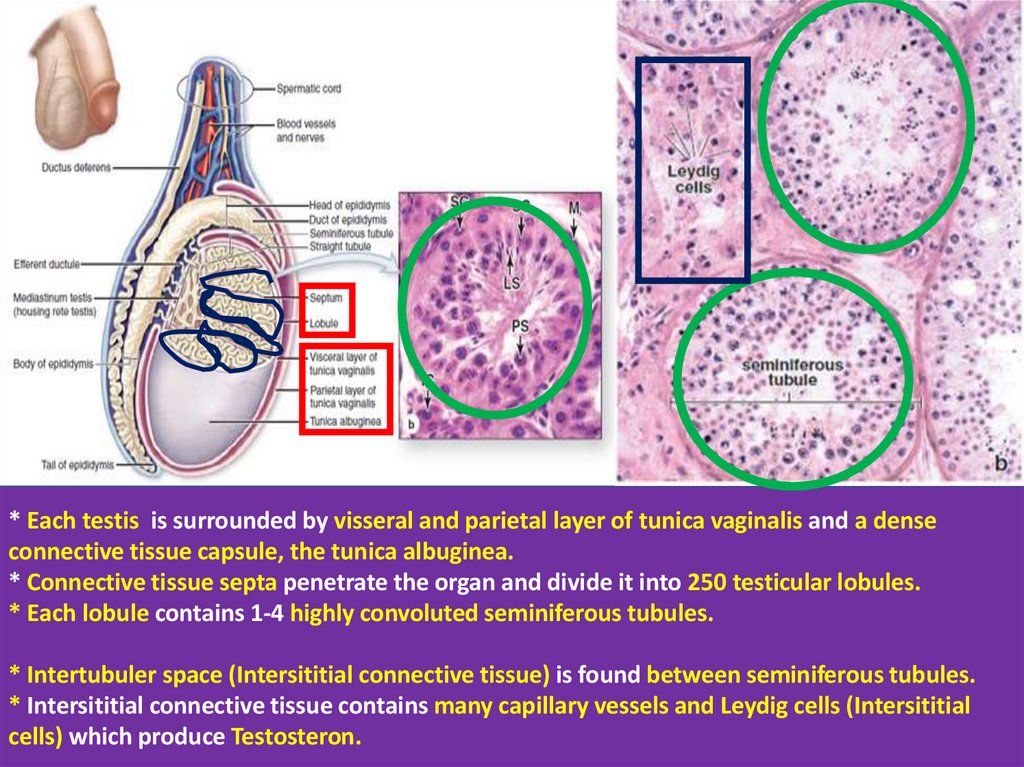
* Each testis is surrounded by visseral and parietal layer of tunica vaginalis and a denseconnective tissue capsule, the tunica albuginea.
* Connective tissue septa penetrate the organ and divide it into 250 testicular lobules.
* Each lobule contains 1-4 highly convoluted seminiferous tubules.
* Intertubuler space (Intersititial connective tissue) is found between seminiferous tubules.
* Intersititial connective tissue contains many capillary vessels and Leydig cells (Intersititial
cells) which produce Testosteron.
9.
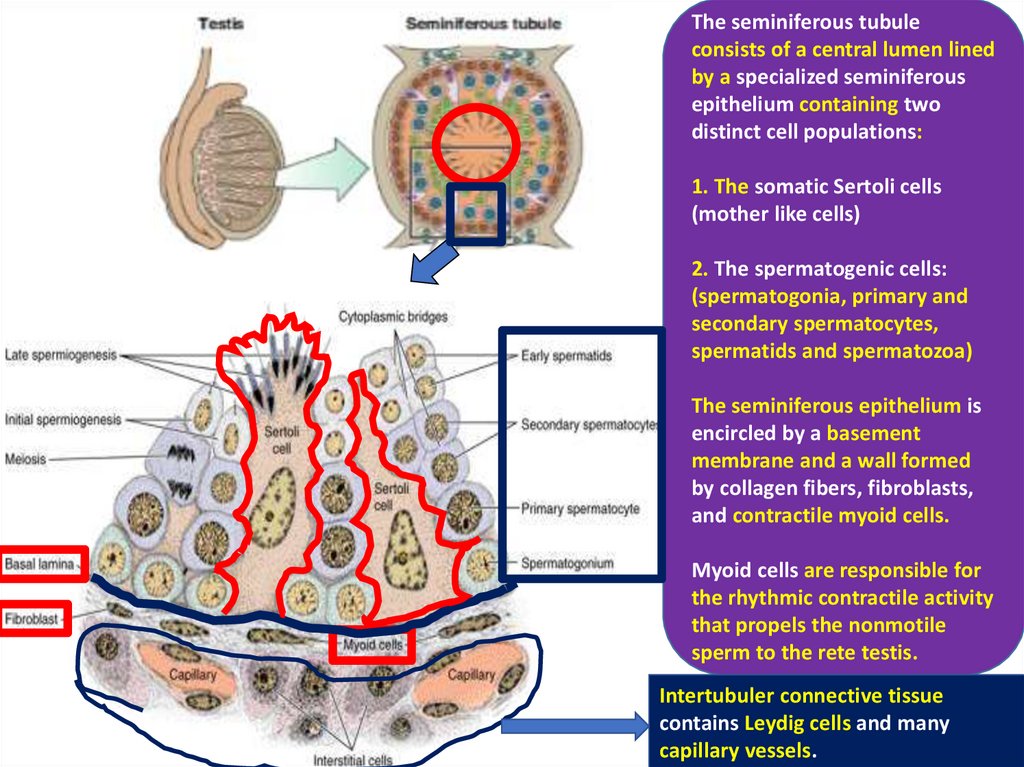
The seminiferous tubuleconsists of a central lumen lined
by a specialized seminiferous
epithelium containing two
distinct cell populations:
1. The somatic Sertoli cells
(mother like cells)
2. The spermatogenic cells:
(spermatogonia, primary and
secondary spermatocytes,
spermatids and spermatozoa)
The seminiferous epithelium is
encircled by a basement
membrane and a wall formed
by collagen fibers, fibroblasts,
and contractile myoid cells.
Myoid cells are responsible for
the rhythmic contractile activity
that propels the nonmotile
sperm to the rete testis.
Intertubuler connective tissue
contains Leydig cells and many
capillary vessels.
10.
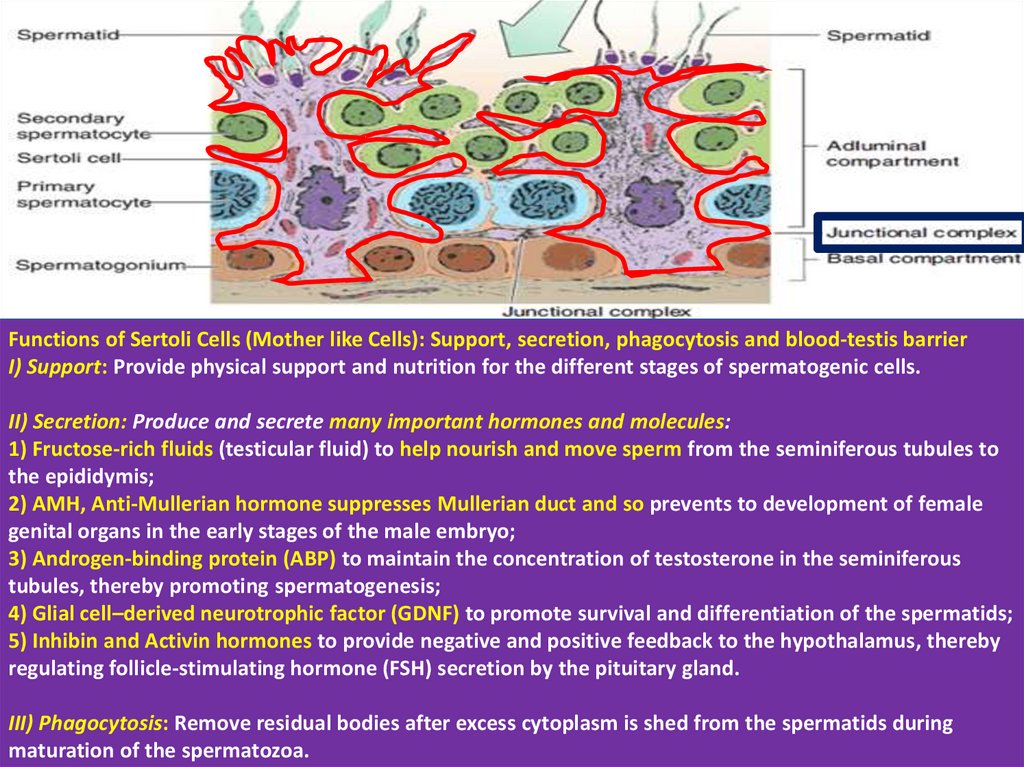
Functions of Sertoli Cells (Mother like Cells): Support, secretion, phagocytosis and blood-testis barrierI) Support: Provide physical support and nutrition for the different stages of spermatogenic cells.
II) Secretion: Produce and secrete many important hormones and molecules:
1) Fructose-rich fluids (testicular fluid) to help nourish and move sperm from the seminiferous tubules to
the epididymis;
2) AMH, Anti-Mullerian hormone suppresses Mullerian duct and so prevents to development of female
genital organs in the early stages of the male embryo;
3) Androgen-binding protein (ABP) to maintain the concentration of testosterone in the seminiferous
tubules, thereby promoting spermatogenesis;
4) Glial cell–derived neurotrophic factor (GDNF) to promote survival and differentiation of the spermatids;
5) Inhibin and Activin hormones to provide negative and positive feedback to the hypothalamus, thereby
regulating follicle-stimulating hormone (FSH) secretion by the pituitary gland.
III) Phagocytosis: Remove residual bodies after excess cytoplasm is shed from the spermatids during
maturation of the spermatozoa.
11.
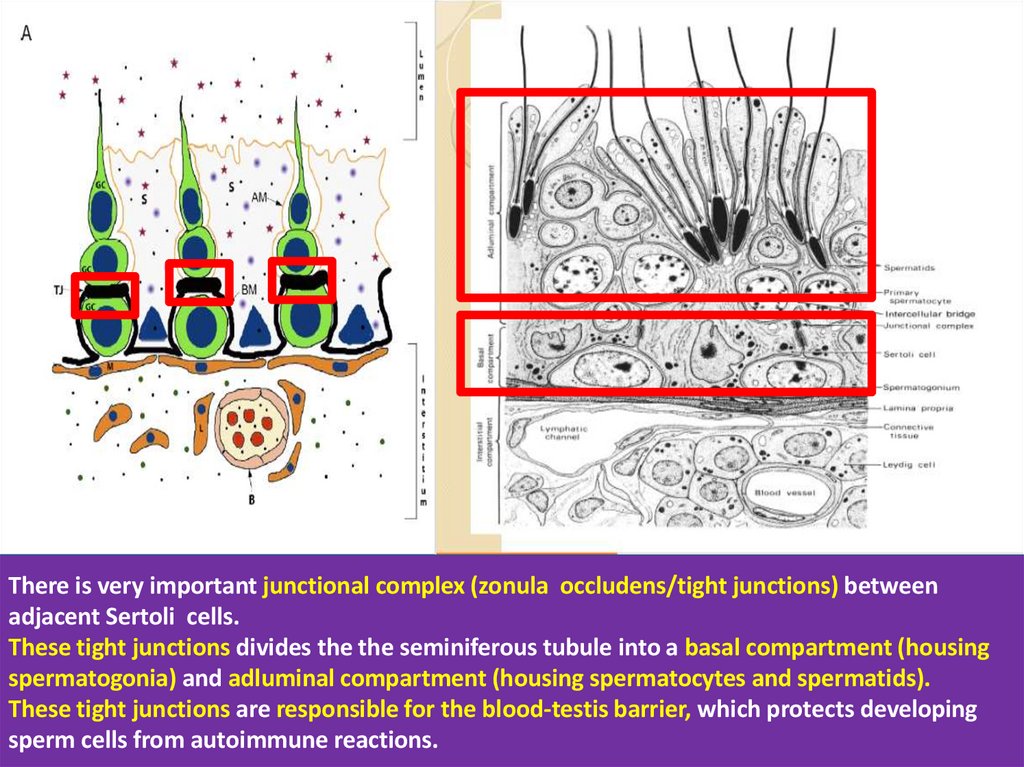
There is very important junctional complex (zonula occludens/tight junctions) betweenadjacent Sertoli cells.
These tight junctions divides the the seminiferous tubule into a basal compartment (housing
spermatogonia) and adluminal compartment (housing spermatocytes and spermatids).
These tight junctions are responsible for the blood-testis barrier, which protects developing
sperm cells from autoimmune reactions.
12.
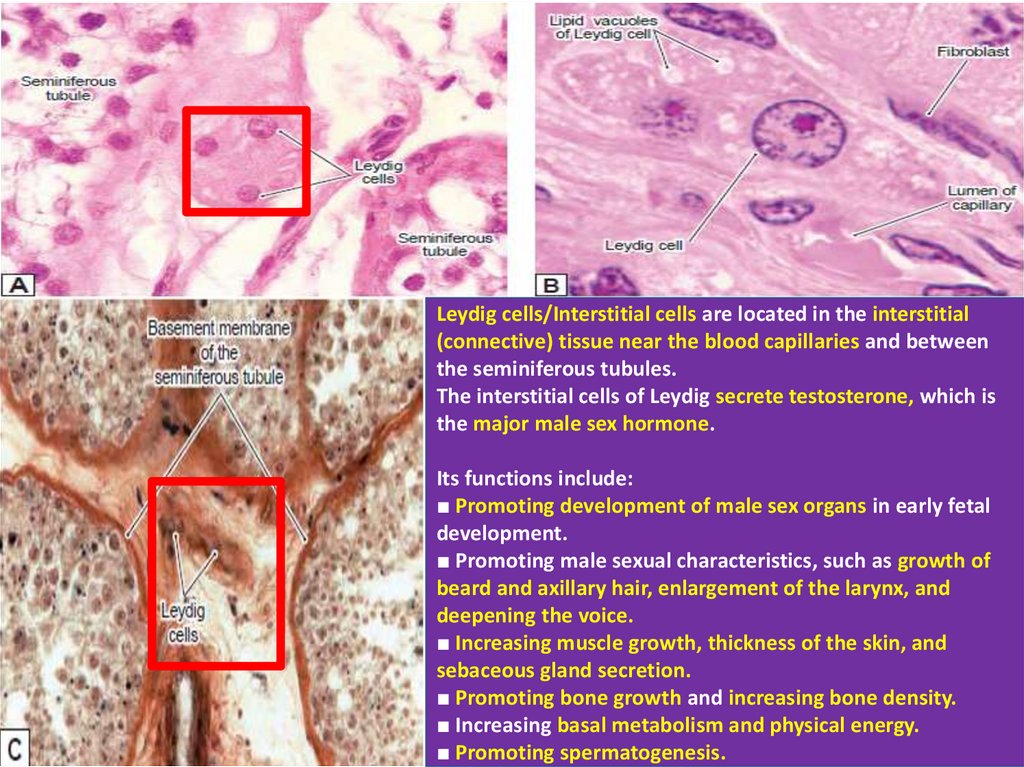
Leydig cells/Interstitial cells are located in the interstitial(connective) tissue near the blood capillaries and between
the seminiferous tubules.
The interstitial cells of Leydig secrete testosterone, which is
the major male sex hormone.
Its functions include:
■ Promoting development of male sex organs in early fetal
development.
■ Promoting male sexual characteristics, such as growth of
beard and axillary hair, enlargement of the larynx, and
deepening the voice.
■ Increasing muscle growth, thickness of the skin, and
sebaceous gland secretion.
■ Promoting bone growth and increasing bone density.
■ Increasing basal metabolism and physical energy.
■ Promoting spermatogenesis.
13.
2. Male genital system and spermatogenesisI) Male reproductive system and histologic organization of the Testis:
* Capsule, septa and testicular lobules
* Fine structure of seminiferous tubule (where spermatogenesis takes place)
* Structure and Functions of Sertoli cells and Leydig cells
II) Common Ancestor Cells=PGCs (Primordial Germ Cells):
Their formation, their migration and their convertion to Spermatogonia
III) When and how spermatogenesis does begin?:
Hypothalamo – Pituitary – Gonadal (Testicular) Axis
IV) Three stages of spermatogenesis:
Spermatogonial stage/Spermatocytogenesis, Meiosis stage, Spermiogenesis
V) Male Infertility and Semen Analysis (Sperm Analysis)
14.
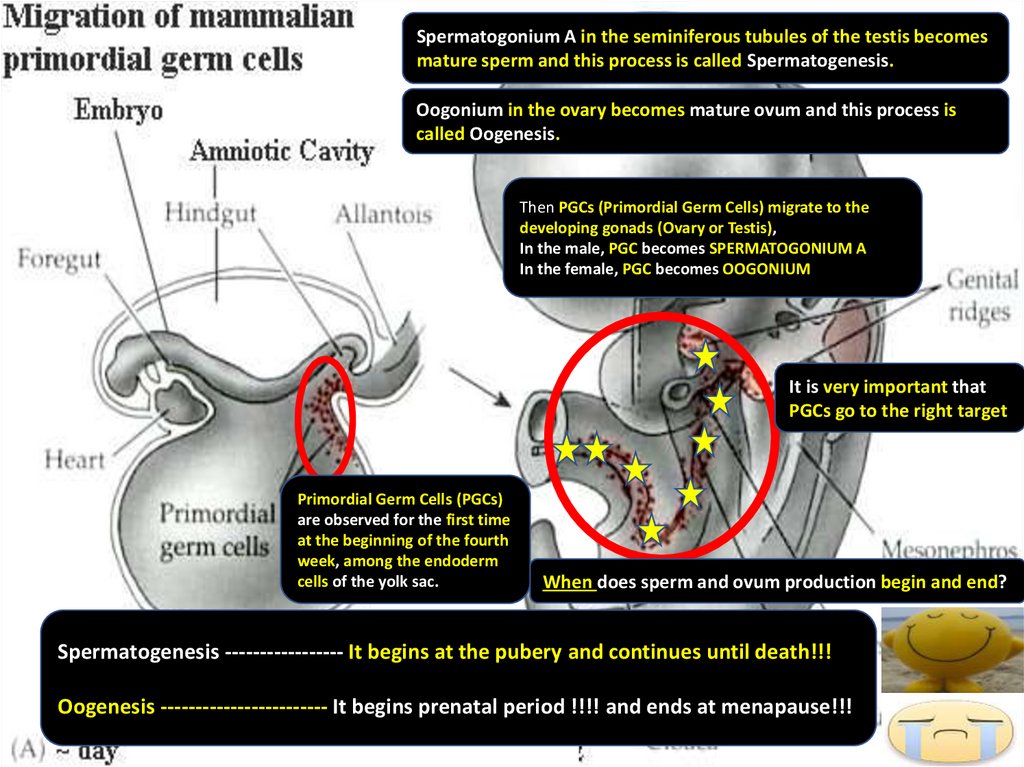
Spermatogonium A in the seminiferous tubules of the testis becomesmature sperm and this process is called Spermatogenesis.
Oogonium in the ovary becomes mature ovum and this process is
called Oogenesis.
Then PGCs (Primordial Germ Cells) migrate to the
developing gonads (Ovary or Testis),
In the male, PGC becomes SPERMATOGONIUM A
In the female, PGC becomes OOGONIUM
It is very important that
PGCs go to the right target
Primordial Germ Cells (PGCs)
are observed for the first time
at the beginning of the fourth
week, among the endoderm
cells of the yolk sac.
When does sperm and ovum production begin and end?
Spermatogenesis ----------------- It begins at the pubery and continues until death!!!
Oogenesis ------------------------ It begins prenatal period !!!! and ends at menapause!!!
15.
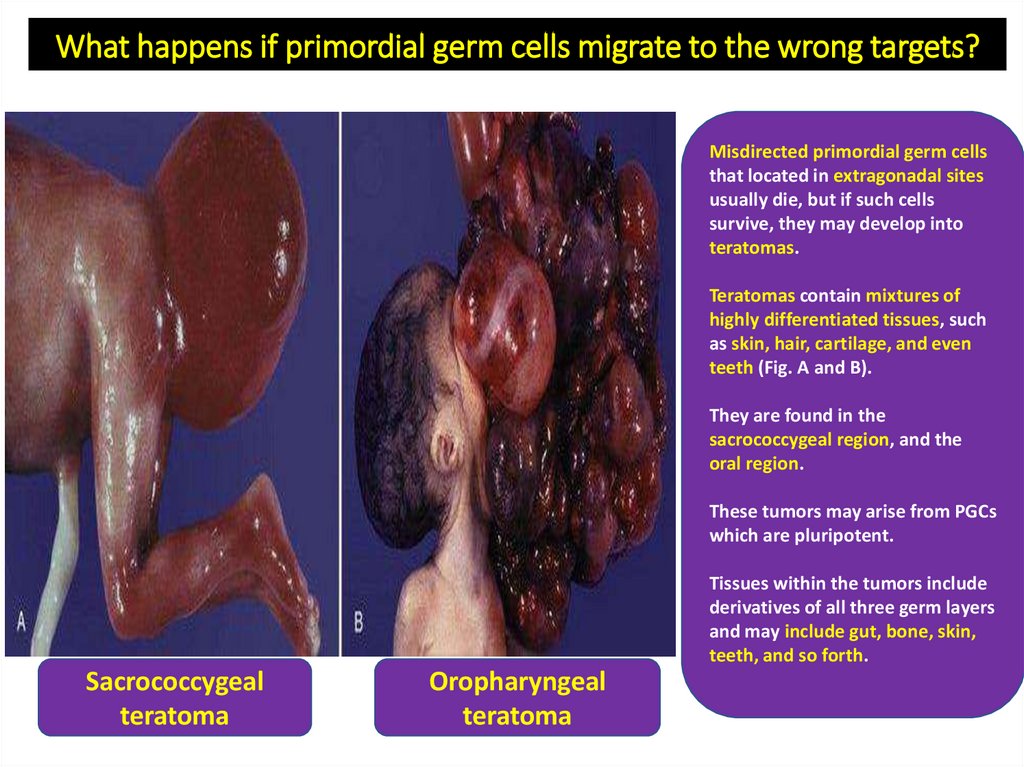
What happens if primordial germ cells migrate to the wrong targets?Misdirected primordial germ cells
that located in extragonadal sites
usually die, but if such cells
survive, they may develop into
teratomas.
Teratomas contain mixtures of
highly differentiated tissues, such
as skin, hair, cartilage, and even
teeth (Fig. A and B).
They are found in the
sacrococcygeal region, and the
oral region.
These tumors may arise from PGCs
which are pluripotent.
Tissues within the tumors include
derivatives of all three germ layers
and may include gut, bone, skin,
teeth, and so forth.
Sacrococcygeal
teratoma
Oropharyngeal
teratoma
16.
2. Male genital system and spermatogenesisI) Male reproductive system and histologic organization of the Testis:
* Capsule, septa and testicular lobules
* Fine structure of seminiferous tubule (where spermatogenesis takes place)
* Structure and Functions of Sertoli cells and Leydig cells
II) Common Ancestor Cells=PGCs (Primordial Germ Cells):
Their formation, their migration and their convertion to Spermatogonia
III) When and how spermatogenesis does begin?:
Hypothalamo – Pituitary – Gonadal (Testicular) Axis
IV) Three stages of spermatogenesis:
Spermatogonial stage/Spermatocytogenesis, Meiosis stage, Spermiogenesis
V) Male Infertility and Semen Analysis (Sperm Analysis)
17.
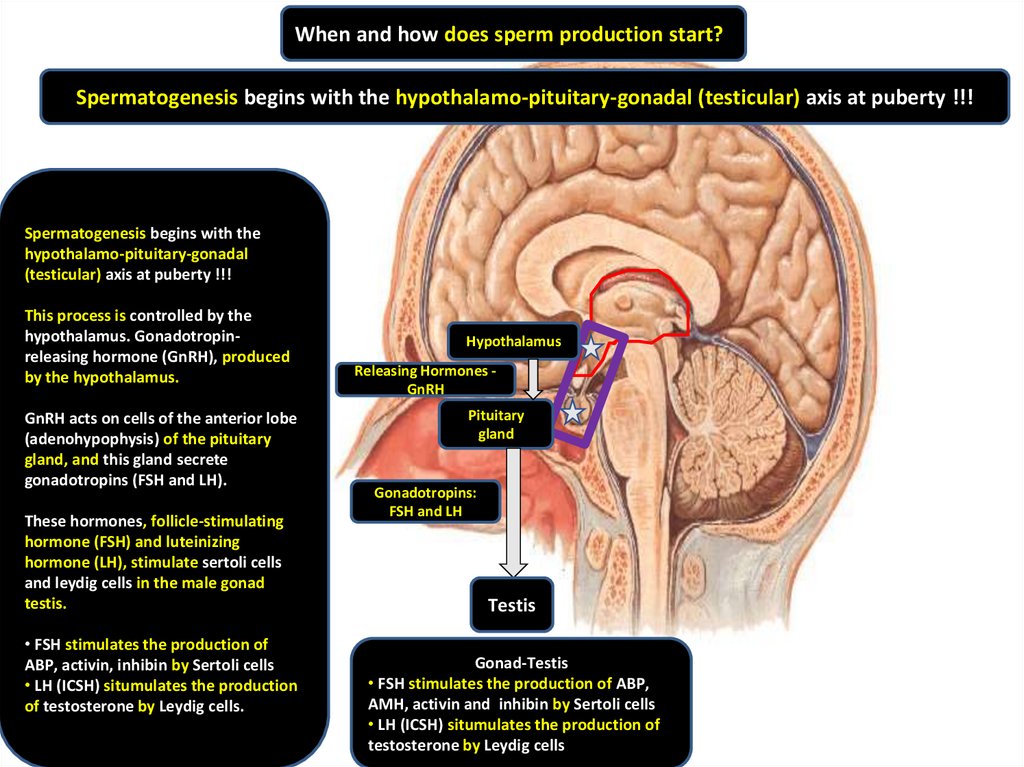
When and how does sperm production start?Spermatogenesis begins with the hypothalamo-pituitary-gonadal (testicular) axis at puberty !!!
Spermatogenesis begins with the
hypothalamo-pituitary-gonadal
(testicular) axis at puberty !!!
This process is controlled by the
hypothalamus. Gonadotropinreleasing hormone (GnRH), produced
by the hypothalamus.
GnRH acts on cells of the anterior lobe
(adenohypophysis) of the pituitary
gland, and this gland secrete
gonadotropins (FSH and LH).
These hormones, follicle-stimulating
hormone (FSH) and luteinizing
hormone (LH), stimulate sertoli cells
and leydig cells in the male gonad
testis.
• FSH stimulates the production of
ABP, activin, inhibin by Sertoli cells
• LH (ICSH) situmulates the production
of testosterone by Leydig cells.
Hypothalamus
Releasing Hormones GnRH
Pituitary
gland
Gonadotropins:
FSH and LH
Testis
Gonad-Testis
• FSH stimulates the production of ABP,
AMH, activin and inhibin by Sertoli cells
• LH (ICSH) situmulates the production of
testosterone by Leydig cells
18.
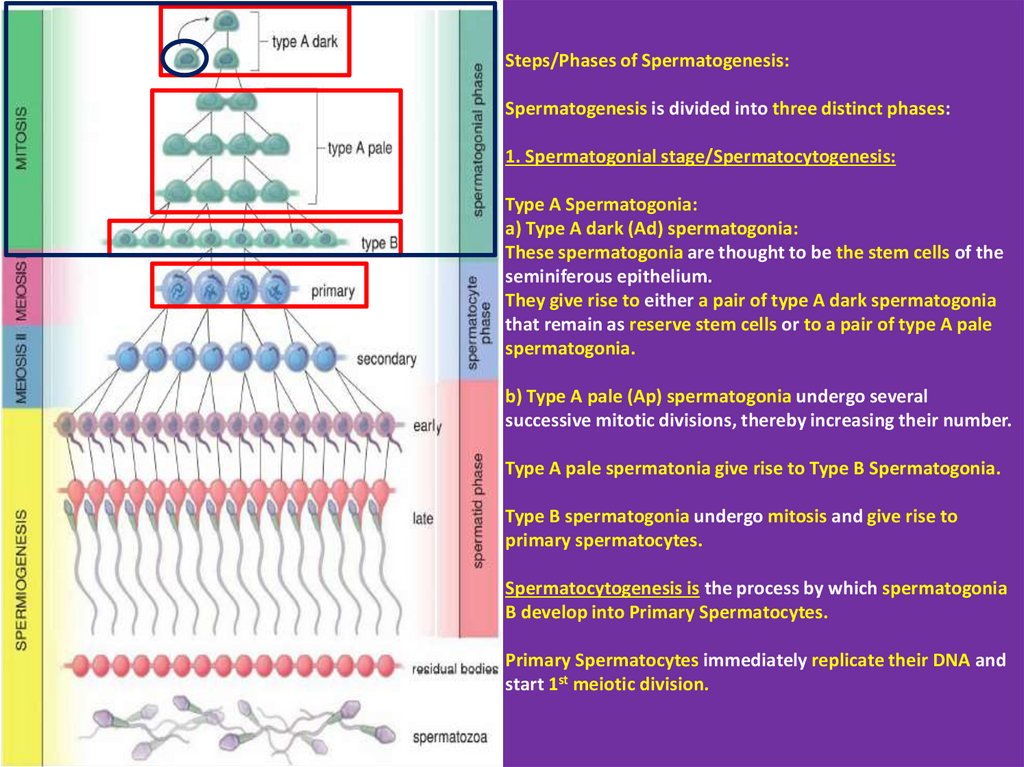
Steps/Phases of Spermatogenesis:Spermatogenesis is divided into three distinct phases:
1. Spermatogonial stage/Spermatocytogenesis:
Type A Spermatogonia:
a) Type A dark (Ad) spermatogonia:
These spermatogonia are thought to be the stem cells of the
seminiferous epithelium.
They give rise to either a pair of type A dark spermatogonia
that remain as reserve stem cells or to a pair of type A pale
spermatogonia.
b) Type A pale (Ap) spermatogonia undergo several
successive mitotic divisions, thereby increasing their number.
Type A pale spermatonia give rise to Type B Spermatogonia.
Type B spermatogonia undergo mitosis and give rise to
primary spermatocytes.
Spermatocytogenesis is the process by which spermatogonia
B develop into Primary Spermatocytes.
Primary Spermatocytes immediately replicate their DNA and
start 1st meiotic division.
19.
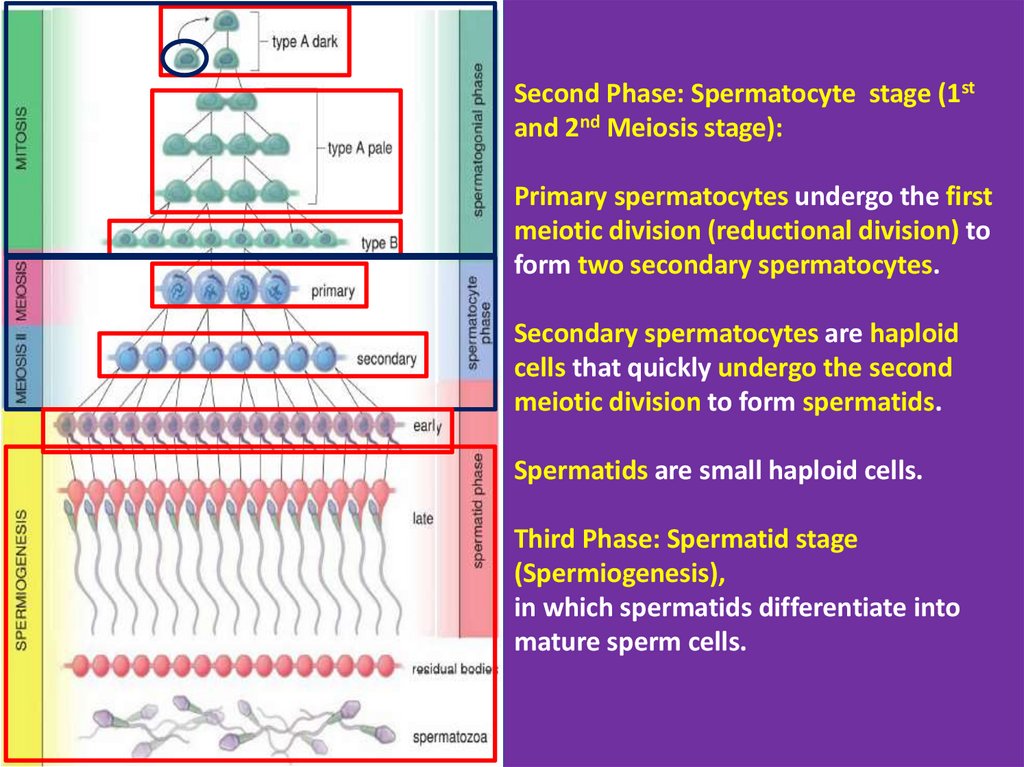
Second Phase: Spermatocyte stage (1stand 2nd Meiosis stage):
Primary spermatocytes undergo the first
meiotic division (reductional division) to
form two secondary spermatocytes.
Secondary spermatocytes are haploid
cells that quickly undergo the second
meiotic division to form spermatids.
Spermatids are small haploid cells.
Third Phase: Spermatid stage
(Spermiogenesis),
in which spermatids differentiate into
mature sperm cells.
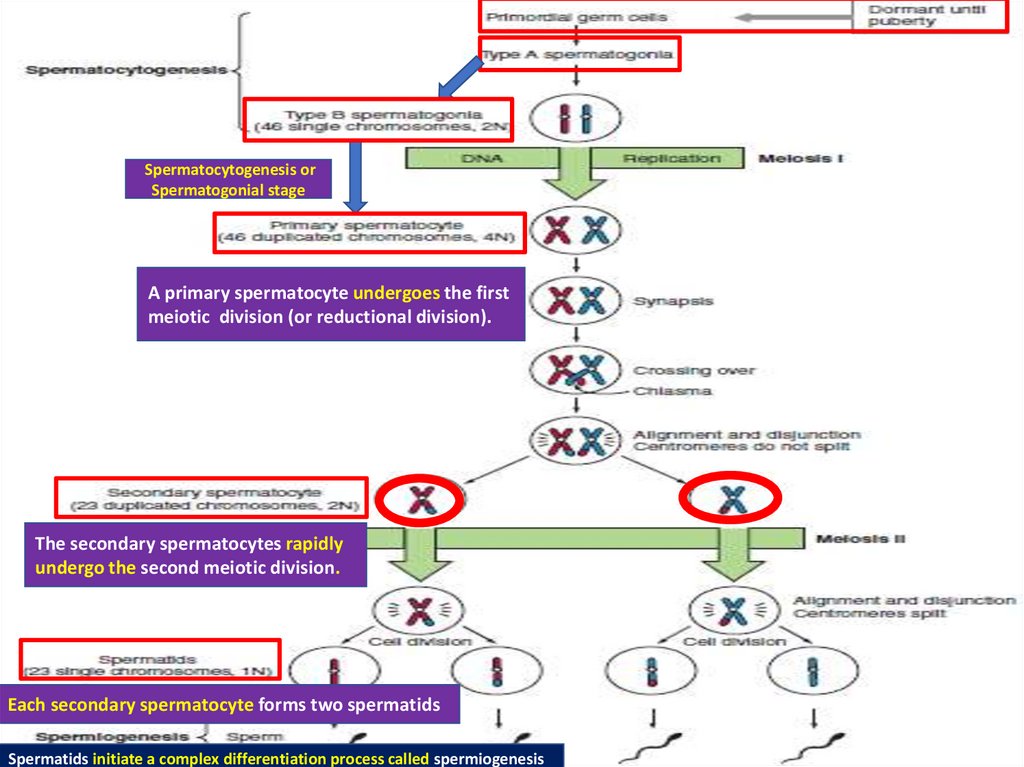
20.
Spermatocytogenesis orSpermatogonial stage
A primary spermatocyte undergoes the first
meiotic division (or reductional division).
The secondary spermatocytes rapidly
undergo the second meiotic division.
Each secondary spermatocyte forms two spermatids
Spermatids initiate a complex differentiation process called spermiogenesis
21.
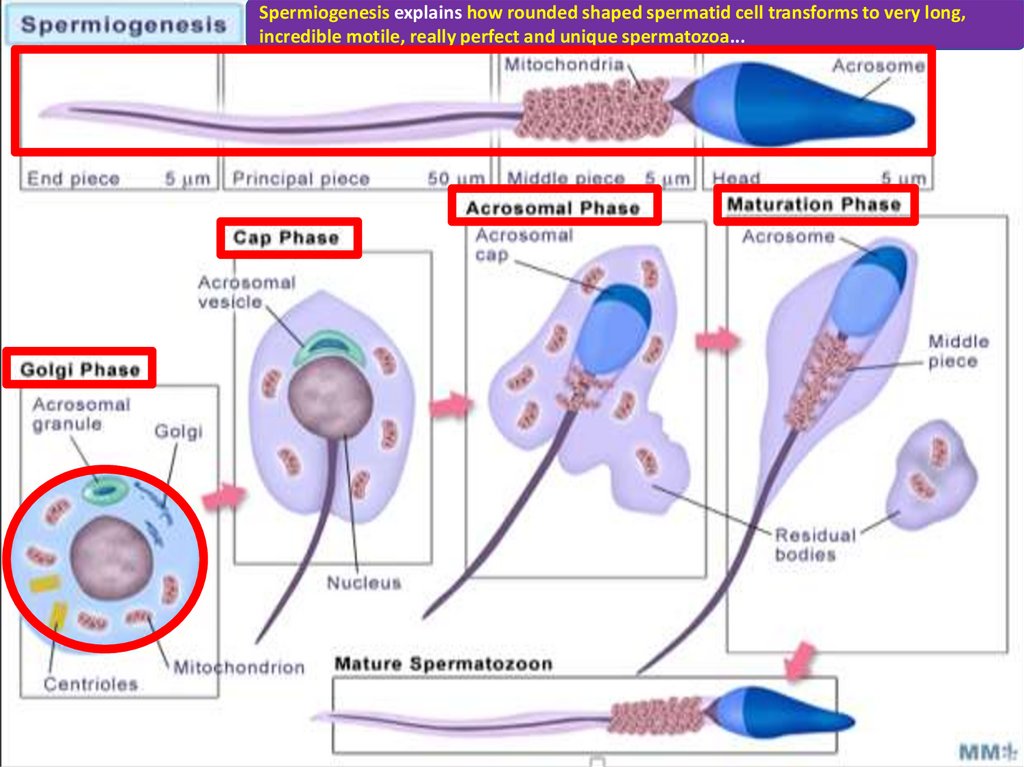
Spermiogenesis explains how rounded shaped spermatid cell transforms to very long,incredible motile, really perfect and unique spermatozoa...
22.
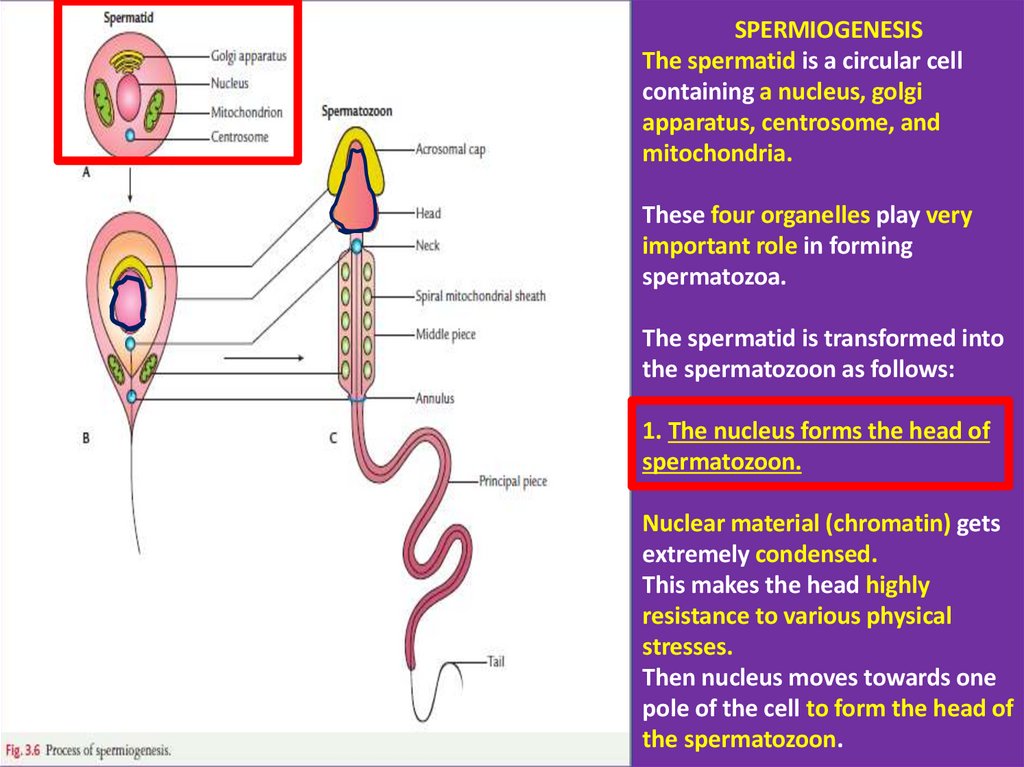
SPERMIOGENESISThe spermatid is a circular cell
containing a nucleus, golgi
apparatus, centrosome, and
mitochondria.
These four organelles play very
important role in forming
spermatozoa.
The spermatid is transformed into
the spermatozoon as follows:
1. The nucleus forms the head of
spermatozoon.
Nuclear material (chromatin) gets
extremely condensed.
This makes the head highly
resistance to various physical
stresses.
Then nucleus moves towards one
pole of the cell to form the head of
the spermatozoon.
23.
SPERMIOGENESIS1. The nucleus forms the head of
spermatozoon.
2. Golgi apparatus forms the
acrosomal cap.
Golgi apparatus forms the
acrosomal cap which contains
hydrolytic enzymes to assist in
penetration of the egg and
surronding corona radiata cells
during fertilization.
Acrosom covers anterior twothird of the nucleus.
24.
SPERMIOGENESIS1. The nucleus forms the head of
spermatozoon.
2. Golgi apparatus forms the acrosomal
cap.
Golgi apparatus forms the acrosomal
cap which contains hydrolytic enzymes
to assist in penetration of the egg and
surronding corona radiata cells during
fertilization.
Acrosom covers anterior two-third of
the nucleus.
3. Centrosome divides into two
centrioles.
4. Mitochondria together with axial flament
forms the middle piece.
The part of the axial filament between the
neck and annulus becomes surrounded by
the mitochondria, and together with them
forms the middle piece.
Mitochondria produce energy for the
movement of tail that facilitates sperm
motility essential for fertilization.
One centriole moves towards the
posterior end of nucleus to occupy the
neck region.
It gives rise to the axonem of the
flagellum (motile cilium).
The other centriole moves away from
the first centriole and forms an
annulus/ring around the distal end of
the middle piece.
25.
Fine Structure of Mature SpermThe mature spermatozoon consists of head, neck,
and tail. The tail is further divided into three parts:
middle piece, principle piece, and end piece.
Head: mainly consists of a nucleus. Anterior twothird of the nucleus is covered by an acrosomal cap
that contains various enzymes including
hyaluronidase and acrosin to assist in penetration
of the egg and its surrounding layers during
fertilization.
Neck: The neck is narrow. It contains proximal
centriole and basal body.
Tail: The tail consists of three parts: middle piece,
principal piece, and end piece.
1. Middle piece: It contains the axial filament
(cilium) in the center that is surrounded by nine
outer dense fibers and spirally arranged
mitochondrial sheath.
2. Principle piece: It is made of axial filament
covered by seven outer dense fibers and fibrous
sheet.
3. End piece: It is made up of only the axial
filament and cell membrane.
26.
2. Male genital system and spermatogenesisI) Male reproductive system and histologic organization of the Testis:
* Capsule, septa and testicular lobules
* Fine structure of seminiferous tubule (where spermatogenesis takes place)
* Structure and Functions of Sertoli cells and Leydig cells
II) Common Ancestor Cells=PGCs (Primordial Germ Cells):
Their formation, their migration and their convertion to Spermatogonia
III) When and how spermatogenesis does begin?:
Hypothalamo – Pituitary – Gonadal (Testicular) Axis
IV) Three stages of spermatogenesis:
Spermatogonial stage/Spermatocytogenesis, Meiosis stage, Spermiogenesis
V) Male Infertility and Semen Analysis (Sperm Analysis)
27.
Semen: It is the mixed fluid ejaculated into the vagina at the time of orgasm.It consists of:
- sperms produced by seminiferous tubules of testes (5%)
- secretion of seminal vesicles, 60% (They secrete nutrients such as fructose
sugar and important proteins needed by the sperm cells)
- secretion of prostate, 30% (Thin milky secretion of the prostate gland is
alkaline in nature and neutralizes the acidic pH of the vagina)
The movement of sperms is best at pH of 6–6.5 while vaginal pH is about 3–4.
The enzymes of prostatic secretion break down the coagulated proteins
secreted by seminal vesicles and make the semen more liquid
- secretion of bulbourethral glands, 5% (Alkalinity of their secretion protects
sperms against the acidity of the urethra and vagina
The secretions of bulbourethral glands also provide lubrication during coitus
28.
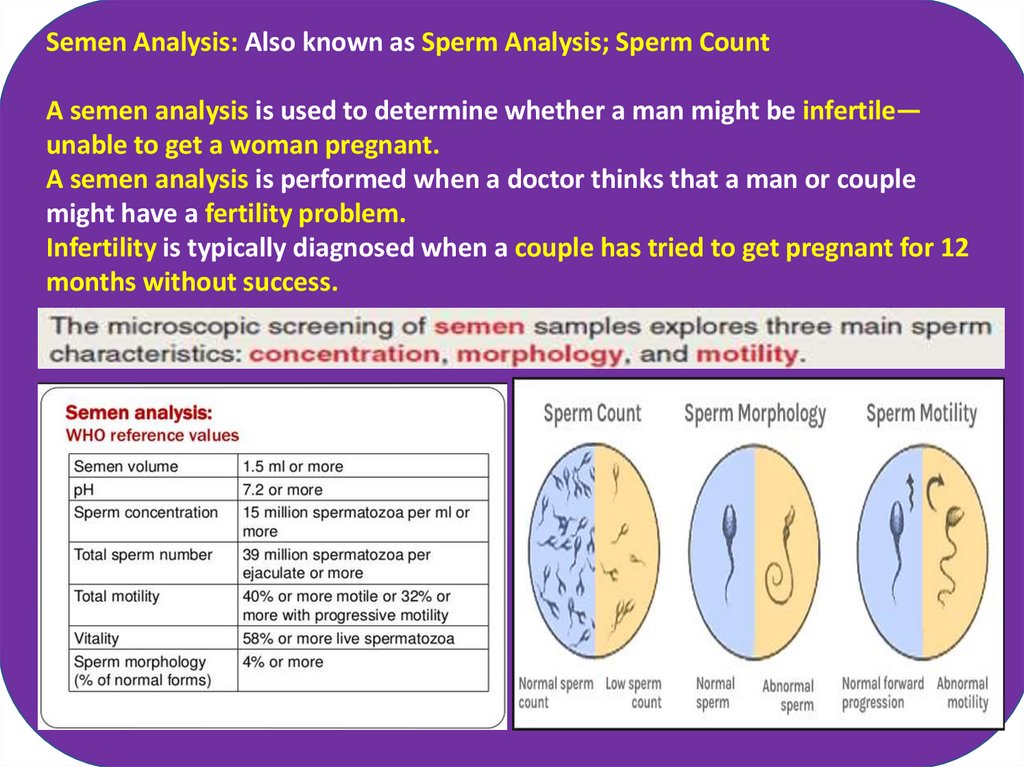
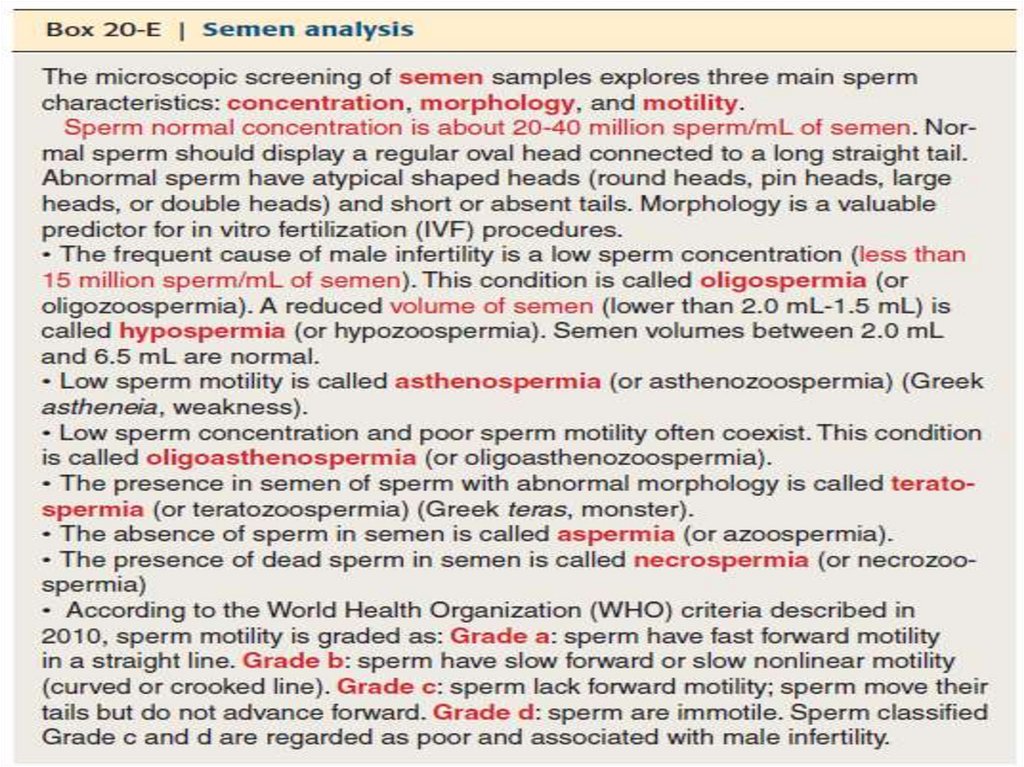
Semen Analysis: Also known as Sperm Analysis; Sperm CountA semen analysis is used to determine whether a man might be infertile—
unable to get a woman pregnant.
A semen analysis is performed when a doctor thinks that a man or couple
might have a fertility problem.
Infertility is typically diagnosed when a couple has tried to get pregnant for 12
months without success.
29.
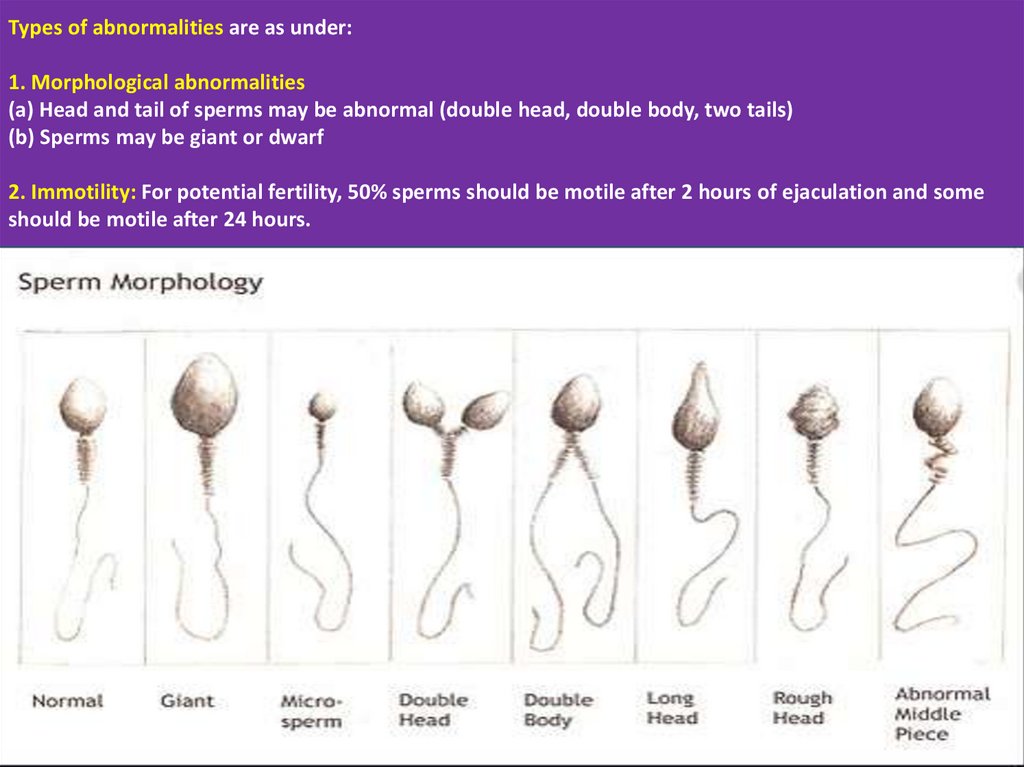
Types of abnormalities are as under:1. Morphological abnormalities
(a) Head and tail of sperms may be abnormal (double head, double body, two tails)
(b) Sperms may be giant or dwarf
2. Immotility: For potential fertility, 50% sperms should be motile after 2 hours of ejaculation and some
should be motile after 24 hours.


 biology
biology