Similar presentations:
Diseases of the thyroid gland
1. DISEASES OF THE THYROID GLAND
Perm State Medical University named after Academician E. A. WagnerPolyclinic therapy department
Shulkina S.G., PhD, MD
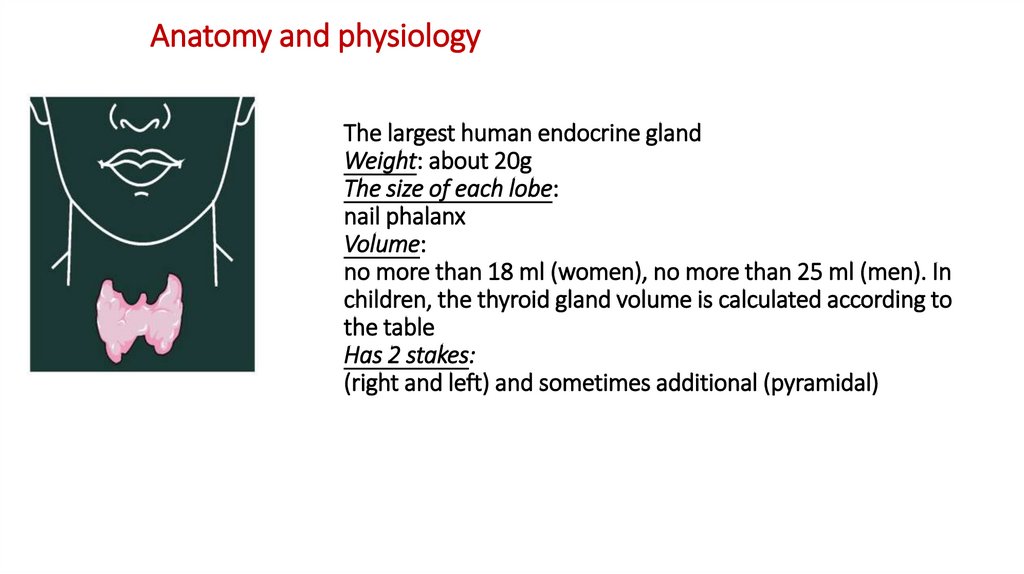
2. Anatomy and physiology
The largest human endocrine glandWeight: about 20g
The size of each lobe:
nail phalanx
Volume:
no more than 18 ml (women), no more than 25 ml (men). In
children, the thyroid gland volume is calculated according to
the table
Has 2 stakes:
(right and left) and sometimes additional (pyramidal)
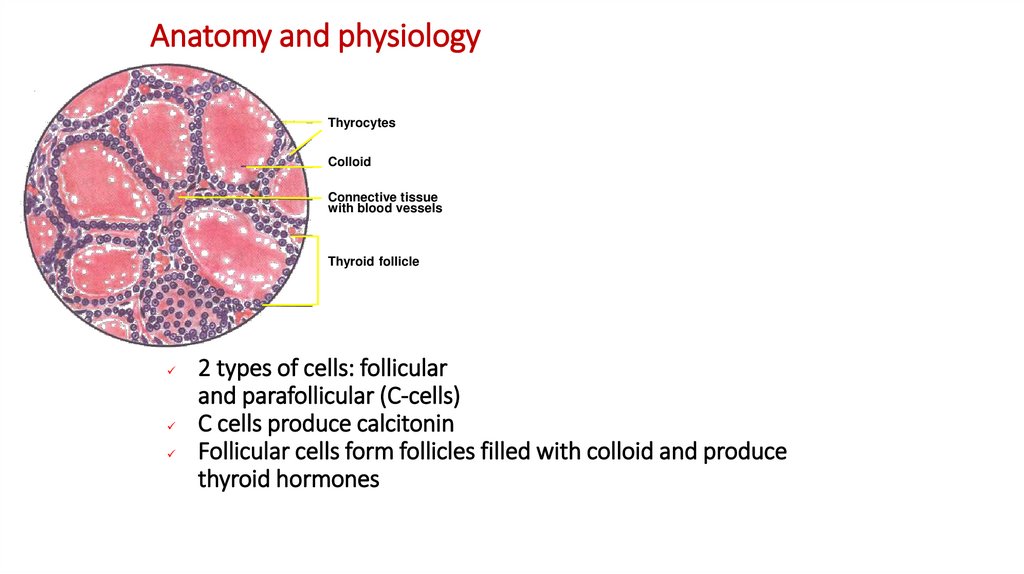
3. Anatomy and physiology
ThyrocytesColloid
Connective tissue
with blood vessels
Thyroid follicle
2 types of cells: follicular
and parafollicular (C-cells)
C cells produce calcitonin
Follicular cells form follicles filled with colloid and produce
thyroid hormones
4. Thyroid hormones
Synthesized from tyrosineT4 - tetraiodothyronine, levothyroxine
T3 - triiodothyronine
Present in serum in 2 forms:
Free
have hormonal activity
very low concentration (T4-0.03%; T3-0.3%)
Associated with transport proteins
thyroxine binding globulin
(T4-75%; T3-80%)
transthyretin and albumin (15% and 10%
respectively for T4; T3 does not communicate with them)
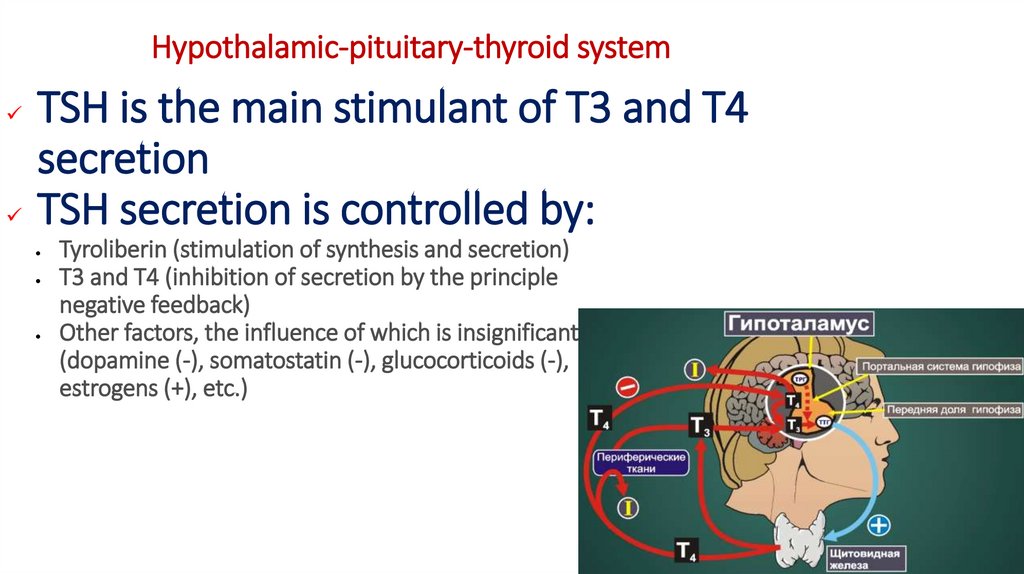
5. Hypothalamic-pituitary-thyroid system
TSH is the main stimulant of T3 and T4secretion
TSH secretion is controlled by:
Tyroliberin (stimulation of synthesis and secretion)
T3 and T4 (inhibition of secretion by the principle
negative feedback)
Other factors, the influence of which is insignificant
(dopamine (-), somatostatin (-), glucocorticoids (-),
estrogens (+), etc.)
6. Physiological effects of thyroid hormones
regulation of growth and developmentregulation of energy metabolism
regulation of protein, carbohydrate
and fat metabolism
effect on the cardiovascular system
effect on the musculoskeletal system
effect on the reproductive system
influence on the psyche
7. Iodine and thyroid hormones
necessary component of T4 and T3the thyroid gland is absorbed from the blood plasma only
inorganic
iodine transport is volatile (ATP)
and is carried out by a sodium iodide symporter
1 gram of thyroid tissue contains
about 300-600 mcg iodine
8. Iodine and thyroid hormones
Absorbed in the intestines and entersinto the inorganic iodine pool of extracellular fluid
Rapidly excreted by the kidneys
3 sources of iodine intake:
alimentary
deiodination of thyroid hormones
in peripheral tissues
"Leakage" of iodine from the thyroid gland
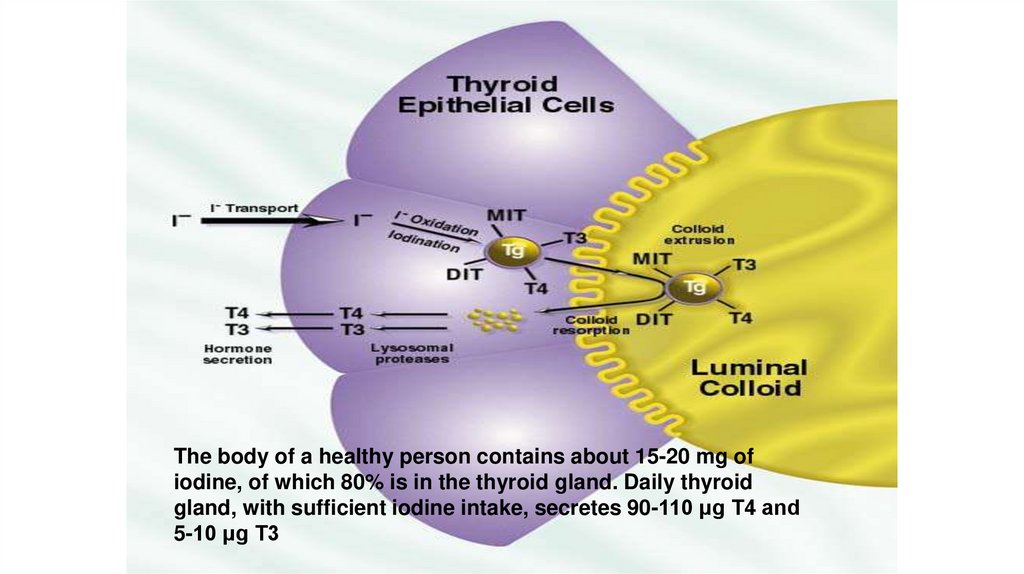
9.
The body of a healthy person contains about 15-20 mg ofiodine, of which 80% is in the thyroid gland. Daily thyroid
gland, with sufficient iodine intake, secretes 90-110 μg T4 and
5-10 μg T3
10. Disease structure uoocyte in the Perm region
in 2016, 20.6 cases of thyroid diseases were registered per 1000 inhabitantsendemic goiter with iodine deficiency -20.9%
hypothyroidism -24.6%
thyroiditis - 14.3%
thyrotoxicosis - 5.9%
over the past 10 years, a pronounced increase in the incidence of the
thyroid gland by 2.5 times has been noted among all groups of the
population
11. Goiter - basic concepts
Goiter - an increase in thyroid volumeEndemic goiter is a diffuse increase in the thyroid gland that
occurs in the population of more than 5% of children of primary
and secondary school age. It is caused by a deficiency in iodine
intake or othergoitrogenic factors
Sporadic goiter is a diffuse increase in the thyroid gland that
occurs in the population of less than 5% of children of primary
and secondary school age. Caused by congenital or acquired
synthesis defectsthyroid hormones
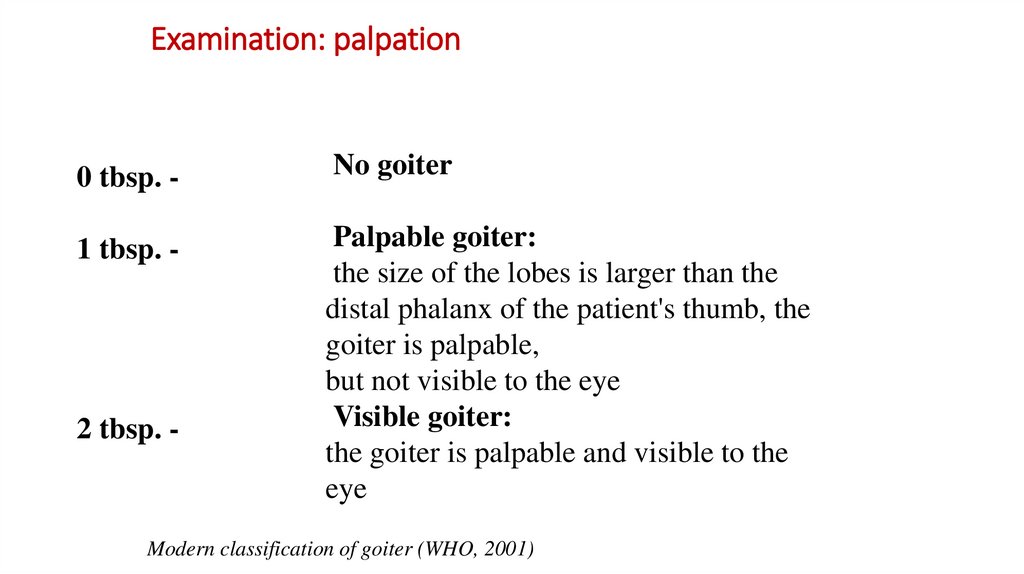
12. Examination: palpation
0 tbsp. -No goiter
1 tbsp. -
Palpable goiter:
the size of the lobes is larger than the
distal phalanx of the patient's thumb, the
goiter is palpable,
but not visible to the eye
Visible goiter:
the goiter is palpable and visible to the
eye
2 tbsp. -
Modern classification of goiter (WHO, 2001)
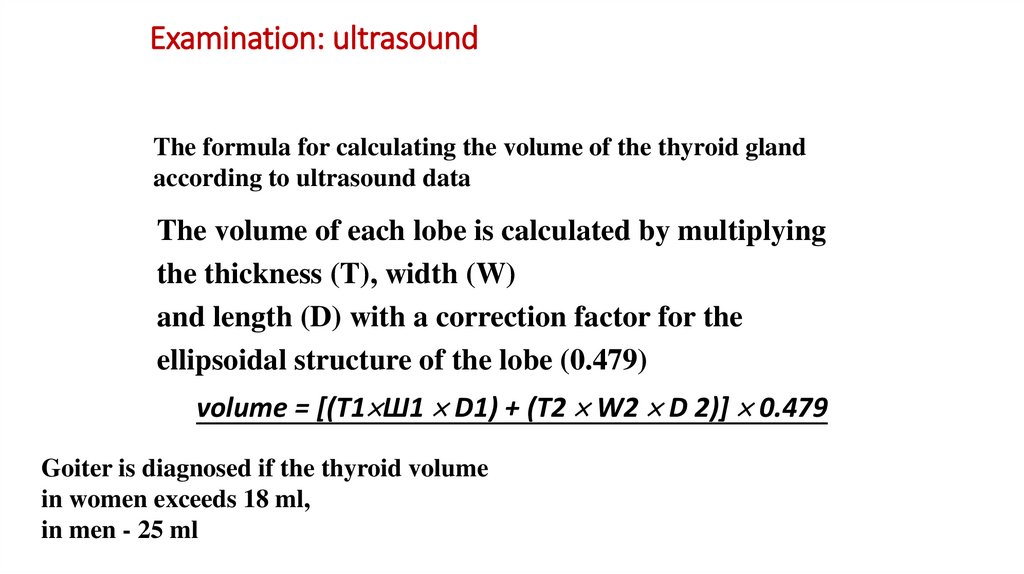
13. Examination: ultrasound
The formula for calculating the volume of the thyroid glandaccording to ultrasound data
The volume of each lobe is calculated by multiplying
the thickness (T), width (W)
and length (D) with a correction factor for the
ellipsoidal structure of the lobe (0.479)
volume = [(T1 Ш1 D1) + (T2 W2 D 2)] 0.479
Goiter is diagnosed if the thyroid volume
in women exceeds 18 ml,
in men - 25 ml
14. Laboratory tests of thyroid function
General T4the simplest and most common method,
based on radioisotope analysis (RIA)
does not always accurately reflect thyroid function
can change at non-thyroid diseases
depends on changes in the concentration of transport proteins
Free T4
the most accurate indicator of thyroid secretory function
and metabolic status of the body
the method takes into account the dependence of the content of svT4
from concentration thyroglobulin
determined by calculation method
Calculated wT4 = Total T4 (μg%, RIA) x Binding Index
15. Laboratory tests of thyroid function
Free T3the calculation method is also used
Calculated wT3 = Total T3 (μg%, RIA) x Binding Index
TSH
methods are used: RIA, immunoradiometric
analysis (IRA) and enzyme-linked immunosorbent assay (ELISA)
the sensitivity of IRA and ELISA is 2 times higher than that of RIA
TSH study is usually used in mass examinations
the determination of TSH alone is not enough to make a diagnosis; T4 and T3 tests are also
needed
16. Other methods for assessing thyroid function
Functional testsThe absorption of radioactive iodine by the thyroid gland
differential diagnosis of various forms of thyrotoxicosis
confirmation of the diagnosis of thyrotoxicosis in patients with thyrotoxicosis
Sample with thyroliberin
previously used to estimate the TSH reserve
and the degree of suppression of TSH secretion
Suppressive test with T3
used to check the autonomy of the thyroid gland
in the differential diagnosis of thyrotoxicosis
Serological tests
Thyroid autoimmune markers
Thyroid cancer markers
17. Other methods for assessing thyroid function
Scintigraphy (used for differential diagnosis"Hot", "warm" and "cold" nodes)
Puncture biopsy (fine needle, aspiration)
- carried out only under ultrasound control
- allows you to get a histological picture
nodal formation
X-ray fluorescent scanning,
CT, MRI
18.
Classification of thyroid diseasesThyroid function
1. Normal - euthyroidism
2. Increased - thyrotoxicosis (hyperthyroidism)
3. Decreased - hypothyroidism
Thyroid size
1. Normal
2. Enlarged - goiter
3. Reduced
19. Most common diseases of the thyroid gland
DNZ (diffuse non-toxic goiter),endemic goiter
Autoimmune thyroiditis
Nodular goiter
Congenital hypothyroidism
Diffuse toxic goiter
20. ICD 10 classification
E01 Diseases of the thyroid gland associated with iodine deficiency
and related conditions
E02 Subclinical hypothyroidism due to iodine deficiency
E03.9 Hypothyroidism unspecified
21.
The main reasons for the development ofdiffuse non-toxic goiter
deficiency of iodine intake with food and water
goitrogenic substances in food and drinking water
hereditary disorders of hormone synthesis
initial manifestations autoimmune
thyroid pathology
22. Daily intake of iodine (WHO)
90 mcg - for children from 0 to 6 years old;120 mcg - for children from 7 to 12 years old;
150 mcg - for older children and adults;
200 mcg - for adolescents, pregnant women
and nursing women.
23. Iodine deficient diseases
Some of the most common noncommunicable diseases in humans (WHO)All in all on earth:
• 1.5 billion people live in the regions
with iodine deficiency
• 600 million have endemic goiter
• 40 million have pronounced mental
failure as a result iodine deficiency
24.
25.
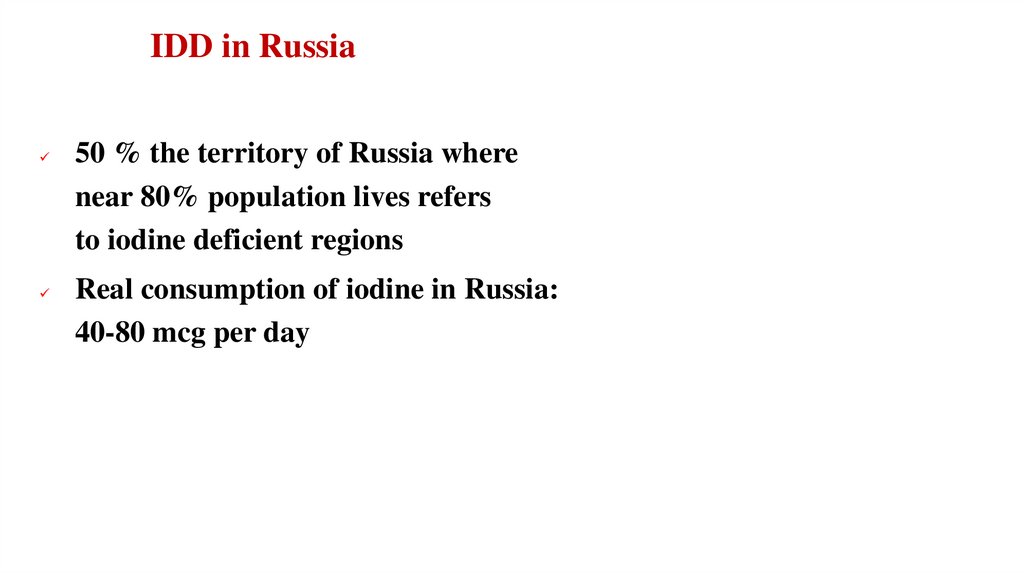
IDD in Russia50 % the territory of Russia where
near 80% population lives refers
to iodine deficient regions
Real consumption of iodine in Russia:
40-80 mcg per day
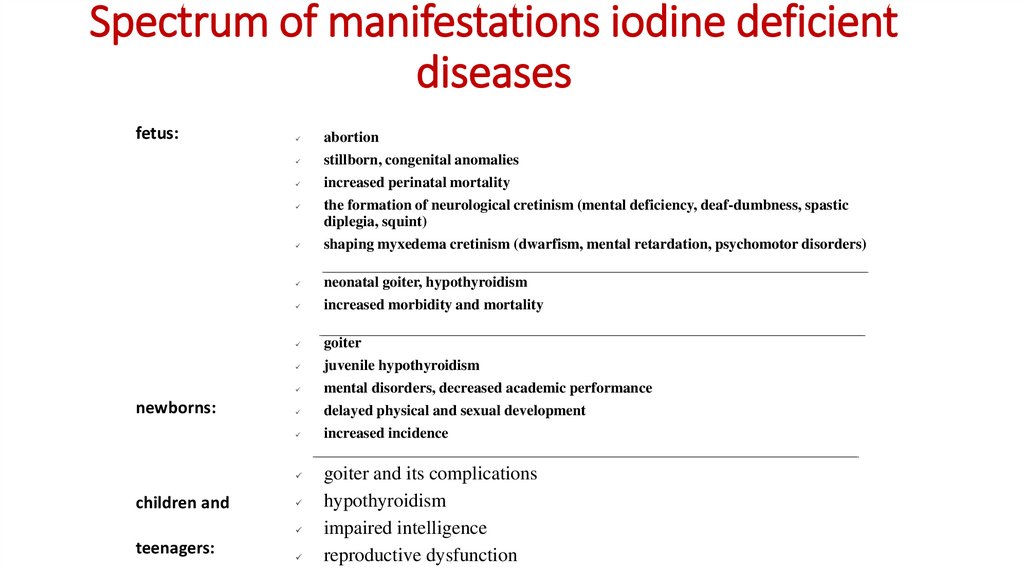
26. Spectrum of manifestations iodine deficient diseases
fetus:abortion
stillborn, congenital anomalies
increased perinatal mortality
newborns:
shaping myxedema cretinism (dwarfism, mental retardation, psychomotor disorders)
neonatal goiter, hypothyroidism
increased morbidity and mortality
goiter
juvenile hypothyroidism
mental disorders, decreased academic performance
delayed physical and sexual development
increased incidence
children and
teenagers:
the formation of neurological cretinism (mental deficiency, deaf-dumbness, spastic
diplegia, squint)
goiter and its complications
hypothyroidism
impaired intelligence
reproductive dysfunction
27.
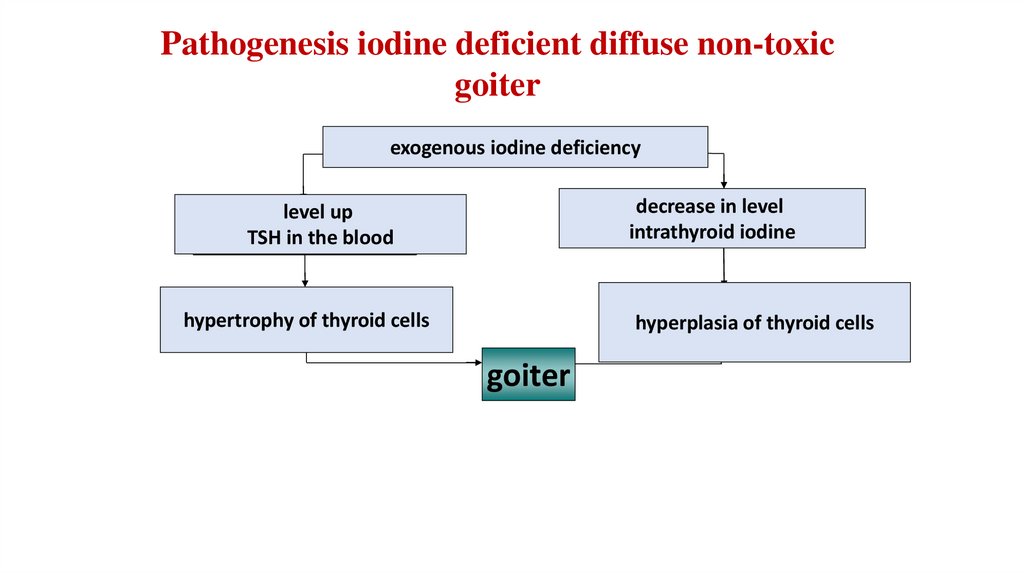
Pathogenesis iodine deficient diffuse non-toxicgoiter
exogenous iodine deficiency
decrease in level
decrease in level
intrathyroid iodine
level
increased
TSHup
levels
TSH
the blood
in in
blood
hypertrophy of thyroid cells
hyperplasia of thyroid cells
goiter
28. IDD risk groups
ChildrenTeenagers
Pregnant women
Lactating women
29.
Iodine prophylaxis methodsMass - iodization of food,
primarily table salt
Group - taking iodine-containing drugs by "risk
groups" for the development of IDD
Individual - preventive administration of dosed
drugs that provide a physiological daily dose of
iodine.
30.
Safety of physiological doses ofpotassium iodide
1 drop Lugol's solution
1 ml alcoholic tincture
of iodine
6.3 mg iodine
40 mg iodine
31.5 tablets "Yodida 200"
200 tablets "Yodida 200"
31.
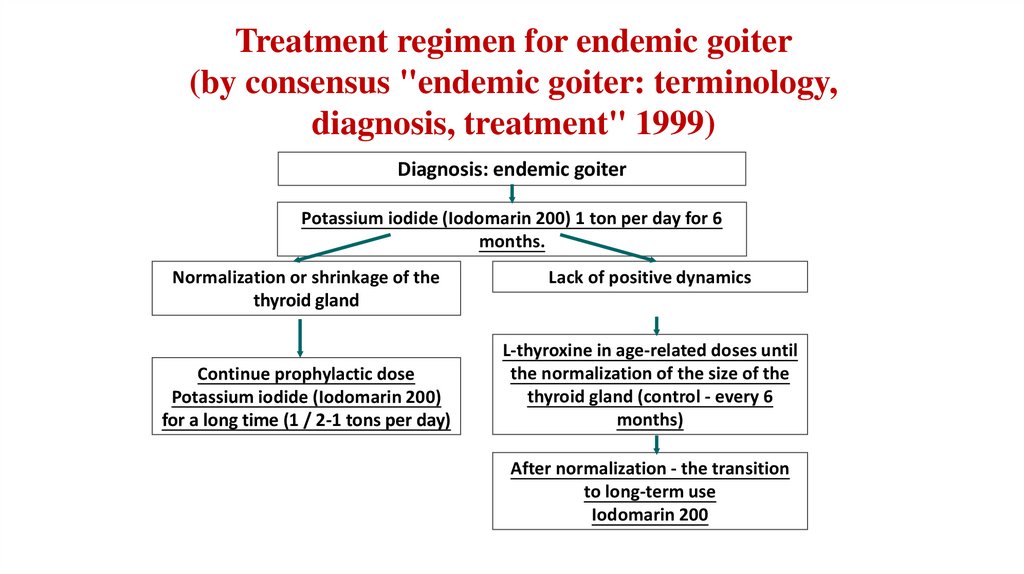
Treatment regimen for endemic goiter(by consensus "endemic goiter: terminology,
diagnosis, treatment" 1999)
Diagnosis: endemic goiter
Potassium iodide (Iodomarin 200) 1 ton per day for 6
months.
Normalization or shrinkage of the
thyroid gland
Continue prophylactic dose
Potassium iodide (Iodomarin 200)
for a long time (1 / 2-1 tons per day)
Lack of positive dynamics
L-thyroxine in age-related doses until
the normalization of the size of the
thyroid gland (control - every 6
months)
After normalization - the transition
to long-term use
Iodomarin 200
32. Thyroiditis
Subacute thyroiditisChronic autoimmune thyroiditis
(thyroiditis Hashimoto) (hypertrophic form)
Atrophic thyroiditis
Juvenile thyroiditis
Postpartum thyroiditis
Focal thyroiditis
33. Thyroiditis
Amiodarone-induced thyroiditis - a group of diseases accompanied by
thyroid dysfunction resulting from the use of amiodarone...
Cytokine-induced thyroiditis - thyroid diseases, most often of a
destructive nature, resulting from the use of drugs based on cytokines...
Thyroiditis as a result of the use of agents containing lithium - a group of
diseases accompanied by thyroid dysfunction resulting from the use of
drugs lithium.
Thyroiditis Riedel- a rare disease characterized by extensive fibrosis,
often affecting, in addition to the thyroid gland, the surrounding
structures
Clinical guidelines 2020
34. According to the functional state of the thyroid gland:
1.Destructive thyroiditis
-
subacute, granulomatous thyroiditis (thyroiditis de Kervain);
-
subacute sporadic lymphocytic thyroiditis (painless, "Dumb");
-
postpartum thyroiditis;
-
amiodarone-induced thyroiditis 2nd type;
-
cytokine-induced thyroiditis;
-
lithium - associated thyroiditis;
-
thyroiditis due to the use radiopaque iodinesubstances; - thyrotoxic
phase of chronic autoimmunethyroiditis ;
35. Subacute thyroiditis (thyroiditis de Kervain)
- inflammatory a thyroid disease that occurs after aviral infection and proceeds with the destruction of
thyroid cells.
- in It develops 5 times more often in women.
- indawns on after a viral infection, more often after
2-3 weeks...
36. etiology
Suspected pathogens: mumps virus, virus Coxsackie, adenoviruses,ECHO viruses, influenza viruses, including H1N1, Epstein virus -Barr...
The mumps virus is cultured directly from thyroid tissue caused by
subacutethyroiditis, apparently, being a special etiological factor. In
addition, PT has been associated with other viral conditions such as
infectious mononucleosis,HIV
Clinical guidelines 2020
37. Subacute thyroiditis stages
initial stage has a duration of 4-8 weeks, they are characterized by the appearance of pain in the
thyroid gland, tenderness of the gland on palpation.
At this stage, there is a massive death of cells in the lesion focus, accumulated in which hormones
begin to quickly enter the blood after the destruction of the cell membrane.
At the initial stage, symptoms of thyrotoxicosis are characteristic (sweating, fever, rapid pulse,
nervousness, etc.), increased blood ESR (usually more than 50 mm / h), (3-10 weeks).
euthyroid stagecharacterized by a gradual normalization of the level of thyroid hormones. At
this stage, the soreness of the gland may persist, but the symptoms of excess hormones in the
blood disappear (1-3 weeks).
Hypothyroid stage... During this stage, the defects in the thyroid tissue gradually heal. The level
of thyroid hormones at this moment may decrease (2-6month)
recovery. Instead of recovery, permanent primary hypothyroidism may develop. This
phenomenon is observed in approximately 5-25% of patients.... In 1-4% of cases,
there is a relapse of the disease
38. Subacute thyroiditis treatment
The mainstay of treatment is the use of glucocorticoid drugs (most often
prednisolone).
The standard dose of prednisolone in the treatment of subacute
thyroiditisis 20 mg per day (two doses of 10 mg). Immediately after the
start of taking prednisolone, the symptoms begin to subside, and by the
end of 3 days after the onset of the pain, the pain should completely
disappear.
Once symptoms have been resolved, it is important to slowly withdraw
prednisone. Complete withdrawal of prednisolone is usually carried out in
1-2 months. It is important not to taper the dose quickly, as this often
leads torecurrencesymptoms. When the symptoms of the disease worsen,
the dose of prednisolone is increased again and then reduced at a very
slow pace.
39. Chronic autoimmune thyroiditis
Etiology• hereditary predisposition
• other autoimmune diseases
• previous pregnancy
Classification
• hypertrophic form (Hashimoto) - 90%
–
diffuse
–
diffuse nodular
–
nodal
• atrophic form - 10%
40. Chronic autoimmune thyroiditis
Flow stages:Hyperthyroidism (Hashitoxicosis) - rarely (10% of cases), is of a
transient nature (no more than 6 months)
Euthyroidism (long asymptomatic course)
Hypothyroidism
41. Consensus: AIT in adults
The diagnosis of AIT cannot be established only on the basis of palpationof the thyroid gland,
as well as detecting increase or decrease
its volume.
The "big" diagnostic signs, the combination of which makes it possible to
establish the diagnosis of AIT, are:
• primary hypothyroidism (manifest
or persistent subclinical);
• the presence of antibodies to thyroid tissue
and ultrasound signs of autoimmune
pathology;
In the absence of at least one of the "large" diagnostic signs, the diagnosis
of AIT is only probabilistic;
42. Consensus: AIT in adults
When hypothyroidism is detected (subclinicalor manifest) diagnostics of AIT makes it possible to establish the nature of the
decrease in the function of the thyroid gland, but practically does not affect the tactics
of treatment, which implies substitution therapy with drugs
thyroid hormones.
Puncture biopsy of the thyroid gland
AIT is not indicated to confirm the diagnosis.
It is mainly carried out as part of a diagnostic search for nodular goiter.
The study of the dynamics of the level of circulating antibodies to the thyroid gland in
order to assess the development and progression of AIT has no diagnostic and
prognostic value
43.
Consensus: AIT in adultsTreatment
Currently, there are no methods of influencing the autoimmune
process itself.
in the thyroid gland (preparations of thyroid hormones,
immunosuppressants, immunomodulators, glucocorticoids,
plasmapheresis
etc.) proved to be effective.
When manifesto hypothyroidism (increased TSH levels and decreased
T4 levels), replacement therapy is indicated levothyroxine in the
middle a dose of 1.6-1.8 mcg / kg of body weight the patient. The
criterion for the adequacy of this therapy is the persistent
maintenance of a normal level of TSH in the blood.
44.
Consensus: AIT in adultsWith subclinical hypothyroidism (increased TSH levels in combination with
normal blood T4 levels) recommended:
repeated hormonal test after 3-6 months
in order to confirm the persistent nature of the thyroid dysfunction; if
subclinical hypothyroidism is detected during pregnancy,
therapylevothyroxine in full replacement dose
appointed immediately;
substitution therapy L-thyroxine is indicated for persistent subclinical
hypothyroidism (an increase in the level of TSH in the blood by more
than 10 honey/ l, as well as in the case of at least two-fold detection
of the TSH level between 5-10 honey/ l
the criterion for the adequacy of substitution therapy for subclinical
hypothyroidism is the persistent maintenance of a normal level of
TSH in the blood.
45.
Consensus: AIT in adultsPrescribing drugs levothyroxinewith AIT (the presence of antibodies to
thyroid tissue and / or ultrasound signs of autoimmune pathology)
without dysfunction of the thyroid gland (normal level of TSH in the
blood) is inappropriate. It can be discussed only in relatively rare cases
of significant thyroid enlargement caused by AIT.
Physiological doses of iodine (about 200 mcg / day)
unable to induce the development of hypothyroidism
and do not adversely affect the function of the thyroid gland in preexisting hypothyroidism caused by AIT.
46. Indications for hospitalization
Acute thyroiditis- in all cases...
-
at conservative treatment after antibiotic therapy with a positive result of treatment and elimination of the threat of
relapse and persistence of the disease.
Indications to discharge: - after surgical treatment with radical elimination of the lesion;
Subacute thyroiditis
Expressed pain syndrome;
Expressed symptoms of thyrotoxicosis.
Indications for discharging a patient from a medical organization for PT:
one) Relief of pain syndrome;
2) Elimination of severe symptoms of thyrotoxicosis.
47. Indications for hospitalization
Amiodarone-induced thyroiditis1)
Amiodarone-induced thyrotoxicosis, severe course (planned or emergency).
Indications for discharge of a patient with amiodarone-induced thyroiditis from a medical organization:
1)
Improvement of well-being;
2) Achievement of target indicators of blood pressure and heart rate;
3) Decrease in the level of free fractions thyroid hormones during treatment.
Cytokine-induced thyroiditis
-
severity symptoms of thyrotoxicosis (severe course);
-
violation thyroid function, not amenable to correction at the outpatient stage;
Indications to discharge from a medical organization (hospital):
- improvement of the condition when the patient can continue treatment in an outpatient clinic or at home without harm to health
48. Hypothyroidism syndromes
Hypothermal exchange syndrome:obesity,
lowering body temperature.
It is important to remember the following: although patients with hypothyroidism
often have moderate excess body weight, their appetite is reduced, which, combined
with depression, prevents significant weight gain, and significant obesity cannot be
caused by hypothyroidism itself.
Impairments of lipid metabolism are accompanied by a change in both the synthesis
and degradation of lipids, and since the impairment of degradation predominates, as a
result, the level of triglycerides increases and lipoproteinslow density, i.e. prerequisites
for the development and progression of atherosclerosis are created.
49. Hypothyroidism syndromes
Hypothyroid dermopathy and syndrome ectodermal violations:myxedema (face, limbs)
periorbital edema,
yellowness of the skin caused by hypercarotenemia,
fragility and hair loss on the lateral parts of the eyebrows, head, up to
alopecia areata and alopecia...
Changes in appearance caused by hypothyroidism sometimes resemble
the degree of coarseness of facial features that occurs with
acromegaly...
With concomitant anemia, the skin color approaches waxy.
50. Hypothyroidism syndromes
Sensory Disorder Syndrome:difficulty in nasal breathing (due to swelling of the nasal mucosa),
hearing impairment (associated with edema of the auditory tube
and middle ear organs),
hoarse voice (due to edema and thickening of the vocal cords).
The deterioration of night vision is revealed.
51. Hypothyroidism syndromes
Syndrome of lesion of the central and peripheral nervous system:drowsiness,
lethargy,
memory loss,
muscle pain
paresthesia,
decreased tendon reflexes,
polyneuropathy...
Development of depression is possible, delirious states (myxedema delirium), increased drowsiness is
typical, bradyphrenia...
paroxysms of panic attacks with recurrent attacks of tachycardia.
52. Hypothyroidism syndromes
Syndrome of damage to the cardiovascular system:myxedema heart (bradycardia, low voltage, negative T wave on the
electrocardiogram, circulatory failure),
hypotension,
polyserositis;
atypical options (with hypertension, without bradycardia; with
tachycardia in case of circulatory failure).
It is important to remember that for myxedema heart rate typically
increased KFK, AST, LDG!!!
53. Hypothyroidism syndromes
Digestive system affection syndrome:hepatomegaly,
dyskinesia biliary tract,
dyskinesia colon,
tendency to constipation,
decreased appetite
atrophy of the gastric mucosa.
54. Hypothyroidism syndromes
Syndrome hyperprolactinemic hypogonadism:
hyperproduction thyrotropin-releasing hormone (TRH) hypothalamus
with hypothyroxinemia increases emission adenohypophysis not only
TSH, but also prolactin...
Clinical syndrome hyperprolactinemic hypogonadism with primary
hypothyroidism,
oligoopomenorrhea or amenorrhea
galactorrhea,
secondary polycystic ovaries.
55. Hypothyroidism syndromes
Obstructive hypoxemic syndrome:sleep apnea syndromedeveloping due to myxedema infiltration of mucous membranes and disorders chemosensitivity
respiratory center.
Myxedema damage to the respiratory muscles with a decrease in tidal volumes and alveolar hypoventilation is one of
the reasons for the accumulation of CO2leading to myxedema coma.
Anemic syndrome
normochromic normocytic,
hypochromic iron deficiency,
macrocytic, IN12- deficiency anemia.
Characteristic of hypothyroidism violations platelet sprout lead to decrease platelet aggregation, which, in combination
with a decrease in plasma levels of factors VIII and IX, as well as increased capillary fragility, aggravates bleeding.
56.
57.
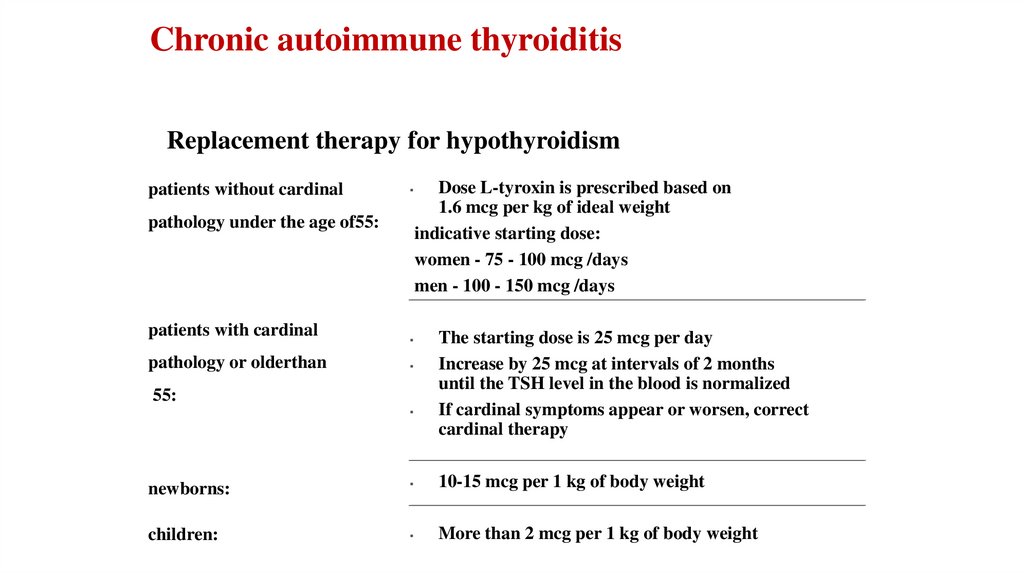
Chronic autoimmune thyroiditisReplacement therapy for hypothyroidism
patients without cardinal
pathology under the age of55:
patients with cardinal
pathology or olderthan
55:
newborns:
children:
Dose L-tyroxin is prescribed based on
1.6 mcg per kg of ideal weight
indicative starting dose:
women - 75 - 100 mcg /days
men - 100 - 150 mcg /days
The starting dose is 25 mcg per day
Increase by 25 mcg at intervals of 2 months
until the TSH level in the blood is normalized
If cardinal symptoms appear or worsen, correct
cardinal therapy
10-15 mcg per 1 kg of body weight
More than 2 mcg per 1 kg of body weight
58. nodular goiter
The prevalence of diffuse endemic goiter indifferent regions of Russia varies from 5.2 to
70% and the national average is 31%.
Have in women, goiter develops 2-3 times
more often than in men. In regions with
iodine deficiency, the prevalence of CCD is
30% in people over 35 and more than 50% in
people over 50. The prevalence of thyroid
cancer among the nodular goiter is about 510%.
nodular
goiter
59. Nodular goiter
The term "node" in clinical practice means a formation in thethyroid gland of any size, defined palpation
and / or using an imaging study
"Nodular goiter" - a collective term used by clinicians prior to
cytological verification of a diagnosis
Thyroid nodules:
• nodular colloid, varying degrees of proliferating goiter
• thyroid tumors (benign and malignant)
60. Nodular goiter
The main link in pathogenesis is a relative lack thyroid hormones, which occursagainst the background of iodine deficiency, leading to hyperproduction TSH
by the pituitary gland followed by proliferation thyrocytes and the
accumulation of colloid.
Survey methods:
The main:
Ultrasound of the thyroid gland
Fine needle biopsy
Determination of the level thyroid hormones and TSH
Additional:
Determination of the level of antithyroid antibodies
Radioisotope scanning
Contrast chest X-ray
barium esophagus
61. NODE GOITER DIAGNOSTICS indications for TAB
- nodal thyroid masses equal to or exceeding 1 cm in diameter;- nodules less than 1 cm, if the patient belongs to the risk group for the presence of aggressive forms of thyroid cancer in the presence of
the following factors:
- basal or stimulated level calcitonin more than 100 pg/ ml;
- the presence of enlarged regional lymph nodes;
- history of head and neck irradiation; - family history of MTC;
- vocal cord paralysis; - thyroid nodules accidentally detected by PET;
- the age of the patients is under 20 years old; at changes in the ultrasound structure of benign thyroid nodules (during dynamic
observation) or when enlarged or altered cervical lymph nodes appear.
-
If ultrasound detects altered regional lymph nodes, their targeted TAB is shown with a study of flushing from the needle on
thyroglobulin or calcitonin depending on the expected morphological form of thyroid cancer.
If a basal level calcitonin above 100 pg/ ml, this is highly suspicious for medullary thyroid cancer.
62. DIAGNOSTICS OF THE NODE indications for TAB
When formations less than 1 cm, if the patient does not belong to the risk group for the presence ofaggressive forms of thyroid cancer, TAB is impractical regardless of the ultrasound characteristics of the
thyroid nodule, except for patients under 20 years of age...
Magnification the size of a benign nodule in itself, in most cases, is not an indication for repeated TAB...
TAB is a method of primary morphological diagnosis, but not a method of dynamic observation in
cytologically verified benign thyroid nodules.
When obtaining a benign cytological report from a node with obvious suspicious ultrasound signs of TAB
must be repeated in the near future...
With cystic anechoic nodes, regardless of the size of the TAB, has no diagnostic value, but can be
performed for the therapeutic purpose of evacuating fluid and eliminating a cosmetic defect or
compression syndrome of surrounding organs.
63. TREATMENT AND SUPERVISION
Tumors of the thyroid gland and presumptive (intermediate) diagnosesthyroidectomy with a central cervical lymphadenectomy followed by 131I
therapy and lifelong dynamic observation in the background substitutive
suppressive drug therapy thyroid hormones.
Colloidal, varying degrees of proliferating goiter
when identifying the nodal (multinode) proliferating goiter, active drug and,
especially, invasive intervention (surgery, sclerotherapy etc.) is optional in most
cases.
Radioactive iodine therapy recommended as an alternative method in the
presence of indications for surgical treatment for benign thyroid tumors,
verified according to TAB data, with a high operational risk. With functional
thyroid autonomy, radioactive iodine therapy is the method of choice.
64. TREATMENT AND SUPERVISION
Dynamic observationDynamic observation implies periodic assessment of thyroid function
(determination of the TSH level) and the size of the nodules (ultrasound).
When the absence of an increase in the size of the nodules, there is no
need for repeated TAB...
In general, it should be borne in mind that gradual, slow growth is
characteristic (but not necessary) for most cases of colloidal proliferating
goiter and by itself it does not yet indicate the malignancy of the nodule.
65. TREATMENT AND SUPERVISION
Surgical treatmentSurgical treatment for nodular (multi-node) euthyroid colloid proliferating goiter is indicated
in the case of:
Nodal (multinode) a goiter with existing signs of compression of surrounding organs
and / or a cosmetic defect.
Nodal (multinode) goiter in the presence of decompensated functional autonomy of
the thyroid gland (toxic goiter) or with a high risk of its decompensation.
The volume of surgical intervention for the nodal (multi-node) goiter is the subject of
ongoing debate, however, it should be noted that the expediency of carrying out
organ-preserving operations in case of changes in both lobes of the thyroid gland is
doubtful and not justified pathogenetically...
66.
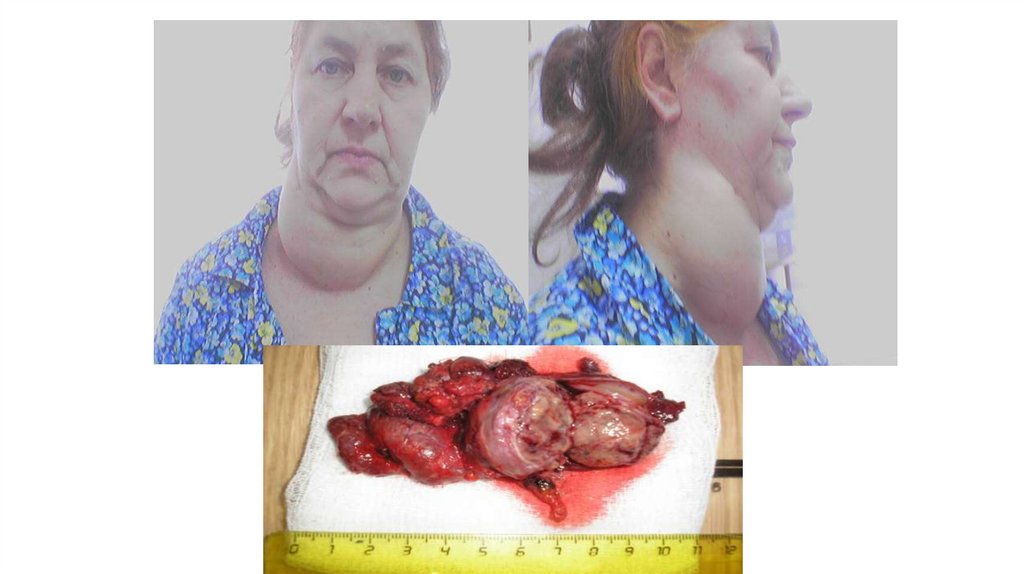
67. Thyrotoxicosis syndrome
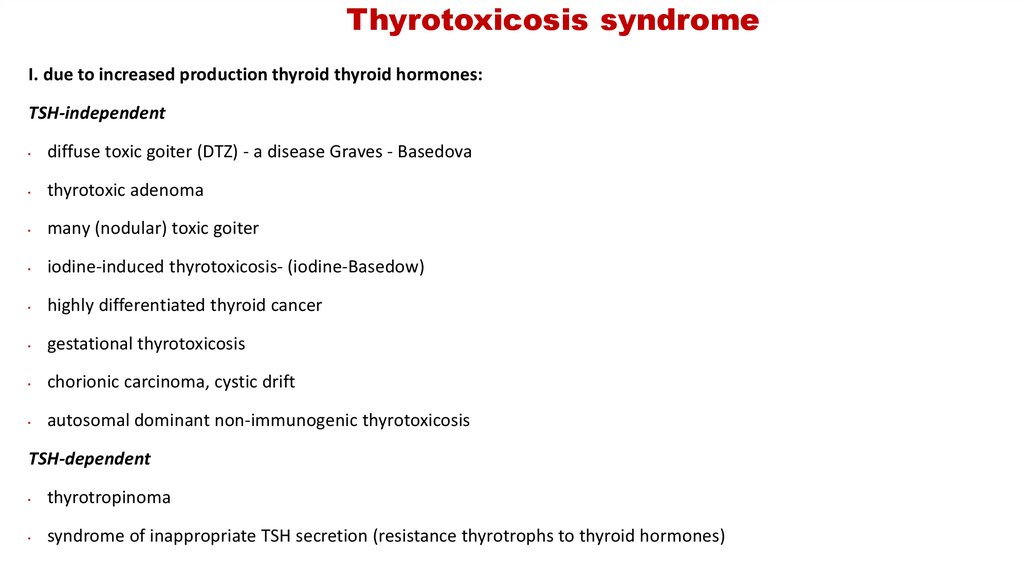
68. Thyrotoxicosis syndrome
I. due to increased production thyroid thyroid hormones:TSH-independent
diffuse toxic goiter (DTZ) - a disease Graves - Basedova
thyrotoxic adenoma
many (nodular) toxic goiter
iodine-induced thyrotoxicosis- (iodine-Basedow)
highly differentiated thyroid cancer
gestational thyrotoxicosis
chorionic carcinoma, cystic drift
autosomal dominant non-immunogenic thyrotoxicosis
TSH-dependent
thyrotropinoma
syndrome of inappropriate TSH secretion (resistance thyrotrophs to thyroid hormones)
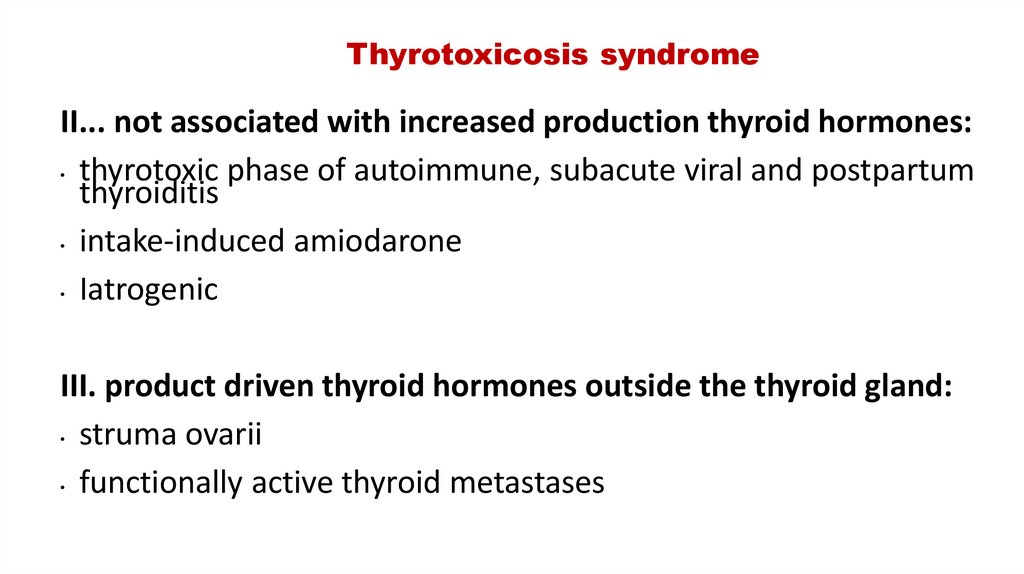
69. Thyrotoxicosis syndrome
II... not associated with increased production thyroid hormones:• thyrotoxic phase of autoimmune, subacute viral and postpartum
thyroiditis
• intake-induced amiodarone
• Iatrogenic
III. product driven thyroid hormones outside the thyroid gland:
• struma ovarii
• functionally active thyroid metastases
70. DTZ
In 1802. - Flayani;
In 1825. - Caleb Parry;
In 1835. - Robert Graves
In 1840. - Carl von Basedow;
71. DTZ- it is an organ-specific autoimmune disease characterized by persistent pathological hypersecretion thyroid hormones,
usually adiffusely enlarged thyroid gland...
Pathogenesis: produced thyroid-stimulating autoantibodies to
TSH receptorsprobably as a result of a congenital defect in the
immune system.
IN 50% reveals similar antibodies in relatives, often found
haplotype HLA DR3, is often combined with other autoimmune
pathology.
72. clinical picture of thyrotoxicosis
one. Damage to the cardiovascular system1.1. Heart rhythm disorders:
Constant sinus tachycardia.
Constant atrial tachyarrhythmia...
Paroxysms atrial tachyarrhythmias against the background of sinus tachycardia.
Paroxysms atrial tachyarrhythmias against the background of normal sinus
rhythm, extrasystole is possible.
1.2. High pulse pressure.
1.3. Circulatory failure due to developmentdyshormonal myocardial dystrophy.
73. clinical picture of thyrotoxicosis
2. Syndrome of catabolic disordersWeight loss with increased appetite.
Subfebrile body temperature.
Muscle weakness.
Thyrogenic osteoporosis.
74. clinical picture of thyrotoxicosis
Damage to the peripheral and central nervous system.Increased excitability and fatigue.
Tearfulness... Disorder sleep.
Tremor body (syndrome of "telegraph pillar ")
Increased sweating
Persistent red dermographism.
Enhancement tendon reflexes.
Ophthalmic symptoms of thyrotoxicosis (Grefe, Kocher, Dalrymple,
Moebius, Geoffroy, Botkin, etc..).
4. Syndrome ectodermal violations.
Delamination and increased fragility nail
Fragility and hair loss.
75. clinical picture of thyrotoxicosis
5.The lesion of the gastrointestinal tract.
Unstable frequent stools (hyperdefecation).
Liver dysfunction up to hepatitis.
76. clinical picture of thyrotoxicosis
6. Damage to other endocrine glandsDevelopment of adrenal insufficiency.
Ovarian dysfunction (menstrual irregularities up to amenorrhea, miscarriage
pregnancy).
Lesion of the mammary and mammary glands (fibrocystic mastopathy,
gynecomastia in men).
Violation of carbohydrate tolerance, the development of diabetes mellitus.
77.
Autoimmune ophthalmopathy - an independent disease ofautoimmune genesis with a lesion periorbital fabrics. 90% of cases are
combined with DTZ, in 5% - with AIT, in 5-10% - without thyroid pathology.
Severity:
1. Swelling of the eyelids, feeling of "sand", lacrimation in the absence of
diplopia.
2.Diplopia, limitation of abduction of the eyeballs, paresis of the gaze upward
3.Incomplete closure of the palpebral fissure, ulceration of the cornea,
atrophy of the optic nerve.
78.
Eye symptomsAutoimmune ophthalmopathy
Grefe - lagging of the upper eyelid from the iris when looking up
Kocher - lagging of the upper eyelid from the iris when looking down
Moebius - loss of the ability to fix a gaze at close range
Geoffroy - absence wrinkles forehead when looking up
Shtelvag - rare blinking
Dalrymple - expansion of the palpebral fissure with the appearance of a
white stripe of the sclera between the iris and and upper eyelid
79.
80.
81. DTD diagnostics
1.2.
3.
prove thyrotoxicosis syndrome: definition of TSH (always
lowered!) and over T3 and over T4 (increased or normal)
prove the presence of a goiter (Ultrasound with gland volume
counting)
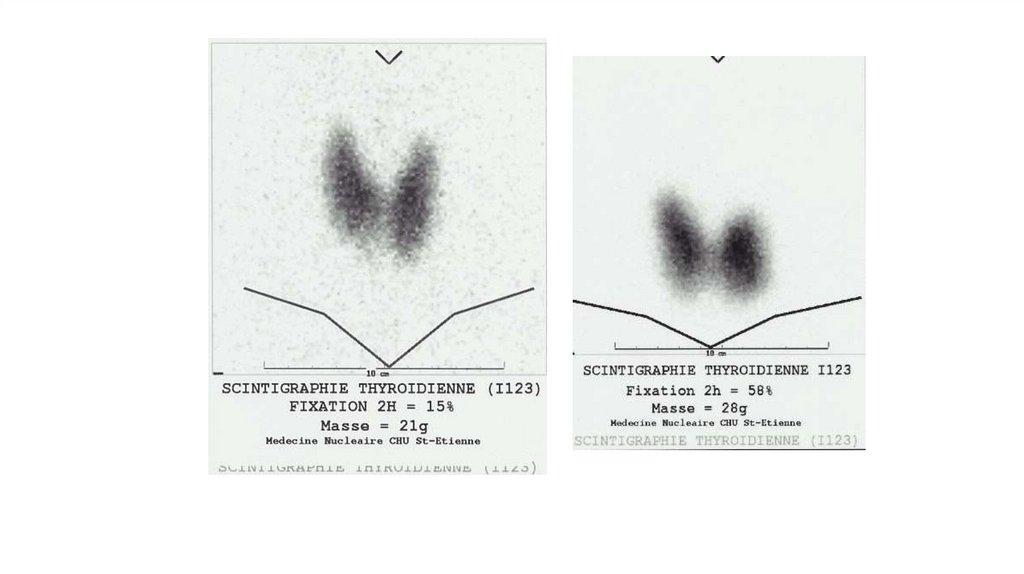
prove that goiter is diffuse (Ultrasound or for differential
diagnosis with functional autonomy or suspected retrosternal
location - scintigraphy Thyroid gland with J 123)
82.
83.
84. Severity of thyrotoxicosis
Option A:
easy - The heart rate is 80-120 per minute, there is no sharp decrease in body weight, there is no
rhythm disturbance, the working capacity is slightly reduced.
Average - Heart rate 100-120 / min., Weight loss up to 10 kg., Reduced efficiency.
Heavy - Heart rate 120 and more beats per minute, MA, psychosis, body weight reduced by more than
10 kg., Dystrophic changes in parenchymal organs, disability is lost.
Option B:
Light (subclinical thyrotoxicosis)-erased clinical picture, the diagnosis is established on the basis of
the hormonal spectrum (reduced TSH and the norm of T4 and T3).
Average (manifest)- there is a detailed clinical picture of the disease (reduced TSH and high T4 and
T3).
Severe (complicated)- there are complications (MA, HF, adrenal insufficiency, psychosis, etc.)
85. DTD treatment (1)
Conservative:derivatives thiourea - mercaptoimidazole (mercazolil, thiamazole, tyrosol, metizol) and
propylthiouracil (propicil)
initial dose
tyrosol 20-60mg /days, propitsila 200-600mg /days
before reaching euthyroidism (2-4 weeks)
gradual dose reduction thyrostatics by 1 tab 1 time per week before supporting (propicil 100mg,
tyrosol - 10 mg),
a plus levothyroxine 50-75 mg /days...
Supportive therapy is carried out 12-18 months
glucocorticoids only when the development of adrenal insufficiency and endocrine ophthalmopathy...Beta-blockers at the
first stage of treatment according to indications (heart rate, blood pressure).
86. complications of conservative therapy
Agranulocytosis (less than 1% of cases), mainly when taking mercaptoimidazole
(control of the level of leukocytes at the beginning of treatment 1 time in 10-14 days, 1
time per month against the background of maintenance therapy. It is not recommended
to take drugs that inhibit hematopoiesis - analgin, amidopyrine, butadion, sulfonamides,
etc.)
vasculitis
cholestatic jaundice, hepatitis (5%)
allergic reactions - rash, itching, urticaria (1-5% of cases, mainly when taking
mercaptoimidazole)
during pregnancy, the drug of choice is propylthiouracil (does not cross the placenta)
with a thyrotoxic crisis, the drug of choice is propylthiouracil (prevents the conversion of T4
to T3)
relapse rate after conservative therapy -40% -60%
87. DTD treatment (2)
Surgical (subtotal subfascial resection of the thyroid gland):combination of DTZ with nodes
large goiter (more than 45 ml), signs of compression of surrounding organs
retrosternally located goiter
lack of a lasting effect of conservative therapy
intolerance thyrostatics
development of complications thyrostatic therapy
postoperative recurrence rate 5-10%
Complications:
recurrent nerve injury with laryngeal paresis
Hypoparathyroidism
88. DTD treatment (3)
Radioactive iodine therapy (J131 10-30 milicurie)indications (Russia):
postoperative relapse of DTG
elderly age
severe concomitant pathology
refusal of the patient from surgery
# in the presence of DTD, 20% of people received radioactive iodine treatment in Europe and
Japan, in the USA - 70%, and in Russia less than 1%.
Relapse occurs in less than 2% of cases.
NB! Woman treated J131 must not breastfeed, be pregnant at the time of treatment, or
become pregnant for years. for menwho have received this treatment are not recommended
to conceive for 120 days. Whole urine of treated patientsJ131 must be in the sewer.
89.
Dispensary follow-upEuthyroiddiffuse goiter II-III degree (D III) endocrinologist 2 times a year. Surgeon - according to indications
With improvement of clinical indicators - transfer to group D II of dispensary observation
Enlargement of the thyroid gland I-II degree without the phenomena of induration and thyrotoxicosis (D II):
therapist - once every six months. Endocrinologist - according to indications
Diffuse toxic goiter (D III): endocrinologist to achieve remission. -Stable remission -Transfer to group D II
Diffuse or nodular toxic goiter after surgical treatment (D III) stable remission: endocrinologist. A year after
the operation, transfer to group D II of dispensary observation
Nodal euthyroidgoiter (without signs of malignancy) after surgery (D III) - 2 times a year surgeon, oncologist according to indications. No relapse - transfer to group D II of dispensary observation
Persons who have undergone surgery on the thyroid gland, in the stage of persistent remission (D II):
therapist once a year. Endocrinologist - according to indications
The presence of grade 1 nodes in the thyroid gland (D II) Endocrinologist 1 time in six months
Hypothyroidism (D III) - According to indications - at least 1 time in 3 months in the dose selection mode.
Surgeon - according to indications












 medicine
medicine