Similar presentations:
Drugs blocking adrenoreceptors
1. Drugs blocking adrenoreceptors
Sympatholytics2.
3.
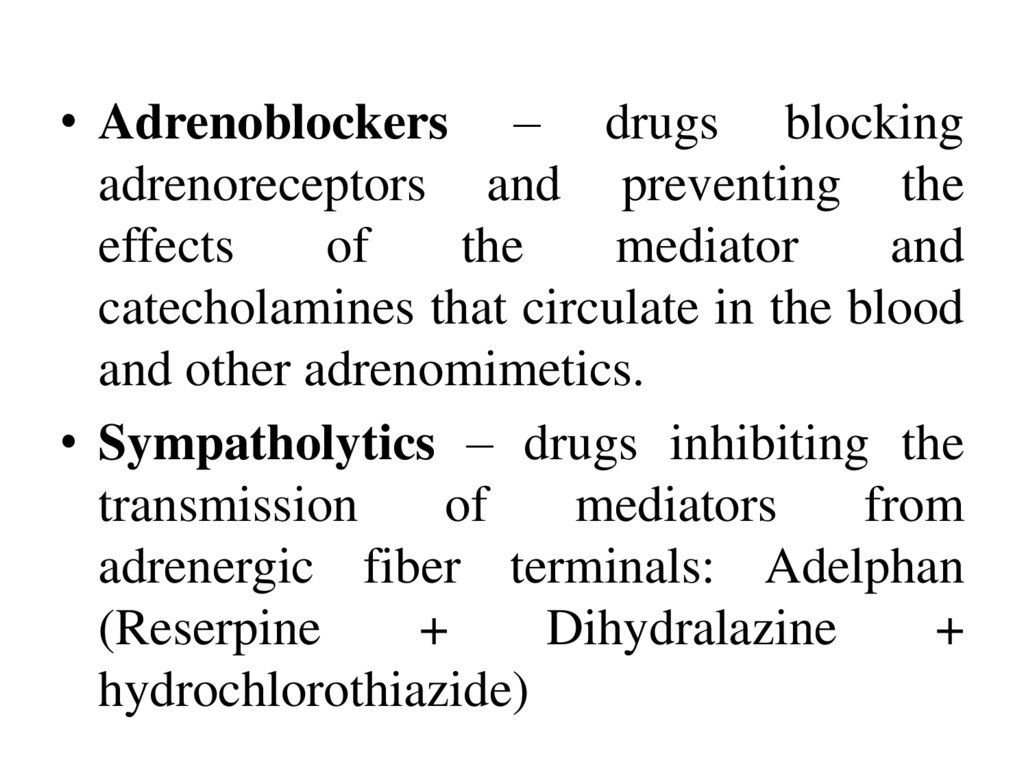
• Adrenoblockers – drugs blockingadrenoreceptors and preventing the
effects
of
the
mediator
and
catecholamines that circulate in the blood
and other adrenomimetics.
• Sympatholytics – drugs inhibiting the
transmission
of
mediators
from
adrenergic fiber terminals: Adelphan
(Reserpine
+
Dihydralazine
+
hydrochlorothiazide)
4.
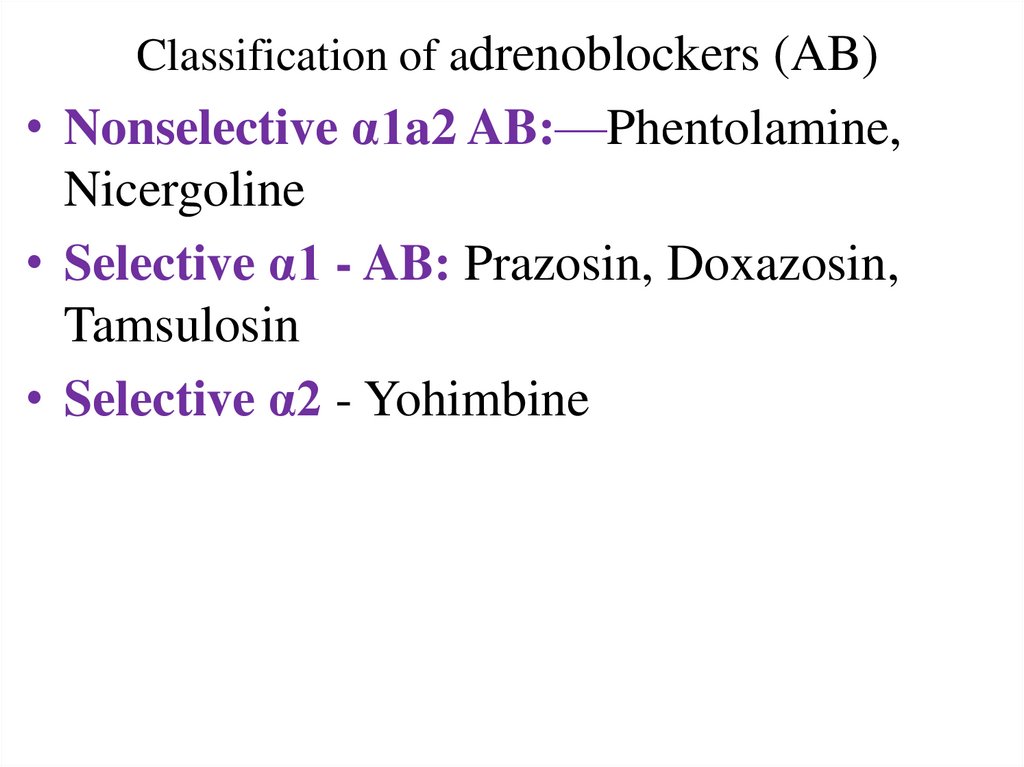
Classification of adrenoblockers (AB)• Nonselective α1a2 AB:—Phentolamine,
Nicergoline
• Selective α1 - AB: Prazosin, Doxazosin,
Tamsulosin
• Selective α2 - Yohimbine
5.
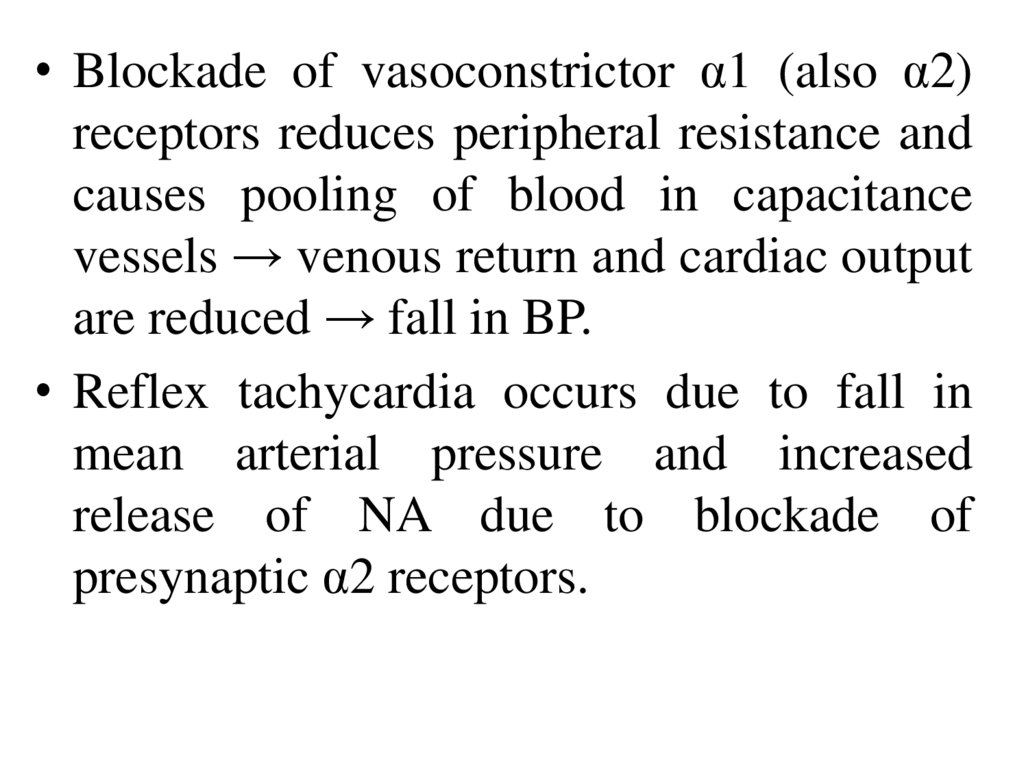
• Blockade of vasoconstrictor α1 (also α2)receptors reduces peripheral resistance and
causes pooling of blood in capacitance
vessels → venous return and cardiac output
are reduced → fall in BP.
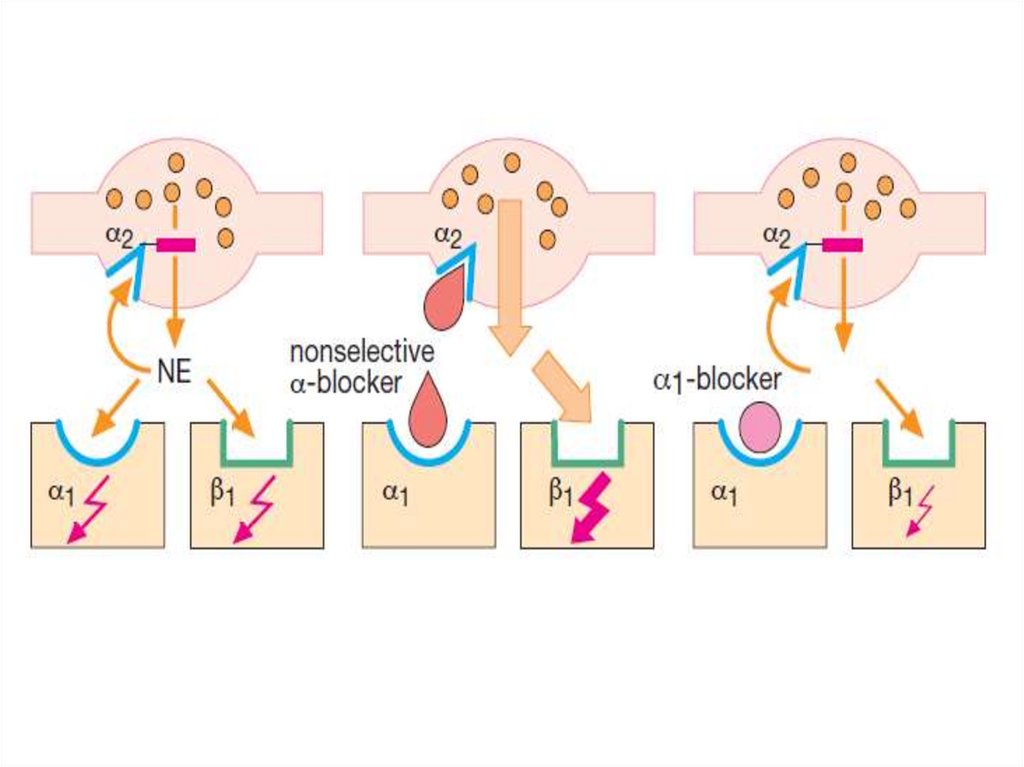
• Reflex tachycardia occurs due to fall in
mean arterial pressure and increased
release of NA due to blockade of
presynaptic α2 receptors.
6.
• Nasal stuffiness and miosis result fromblockade of α receptors in nasal blood
vessels and in radial muscles of iris.
• Intestinal motility is increased.
• Tone of smooth muscle in bladder trigone,
sphincter and prostate is reduced by
blockade of α1 receptors (mostly of the
α1A subtype) → urine flow in patients
with benign hypertrophy of prostate
(BHP) is improved.
7.
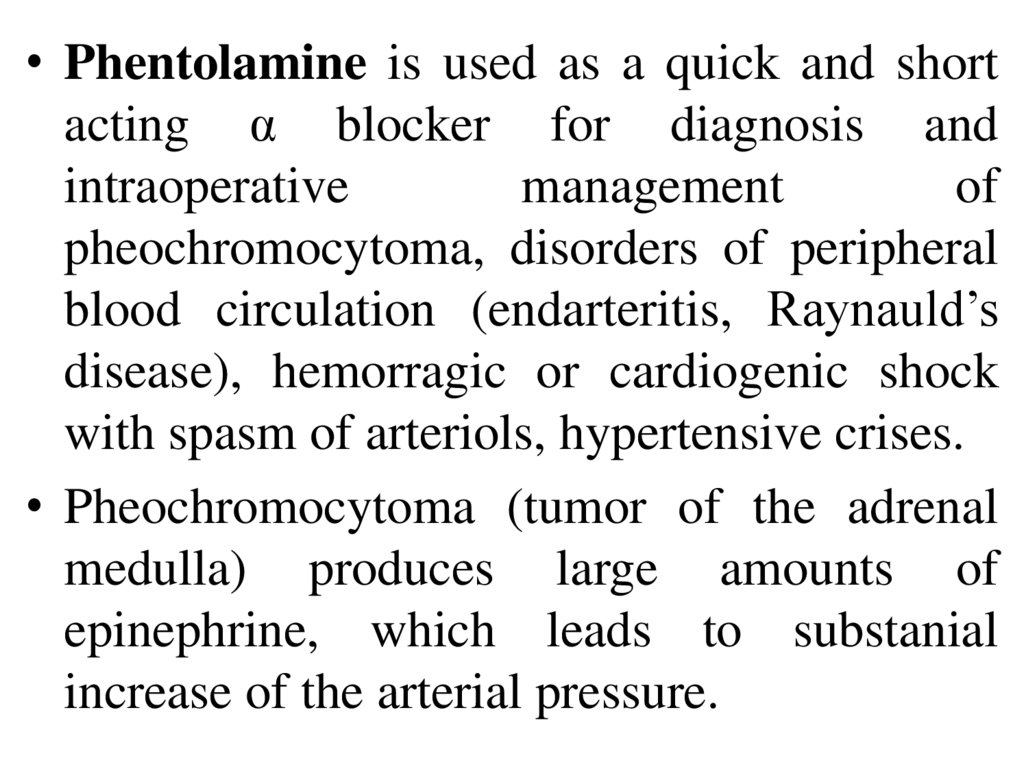
• Phentolamine is used as a quick and shortacting α blocker for diagnosis and
intraoperative
management
of
pheochromocytoma, disorders of peripheral
blood circulation (endarteritis, Raynauld’s
disease), hemorragic or cardiogenic shock
with spasm of arteriols, hypertensive crises.
• Pheochromocytoma (tumor of the adrenal
medulla) produces large amounts of
epinephrine, which leads to substanial
increase of the arterial pressure.
8.
• Side effects:the block
orthostatic
exacerbation
itching, skin
reactions.
tachycardia partially due to
of presynaptic α₂-AR;
collapse,
dizziness,
of peptic ulcer, dyspepsia,
hyperemia. edema, allergic
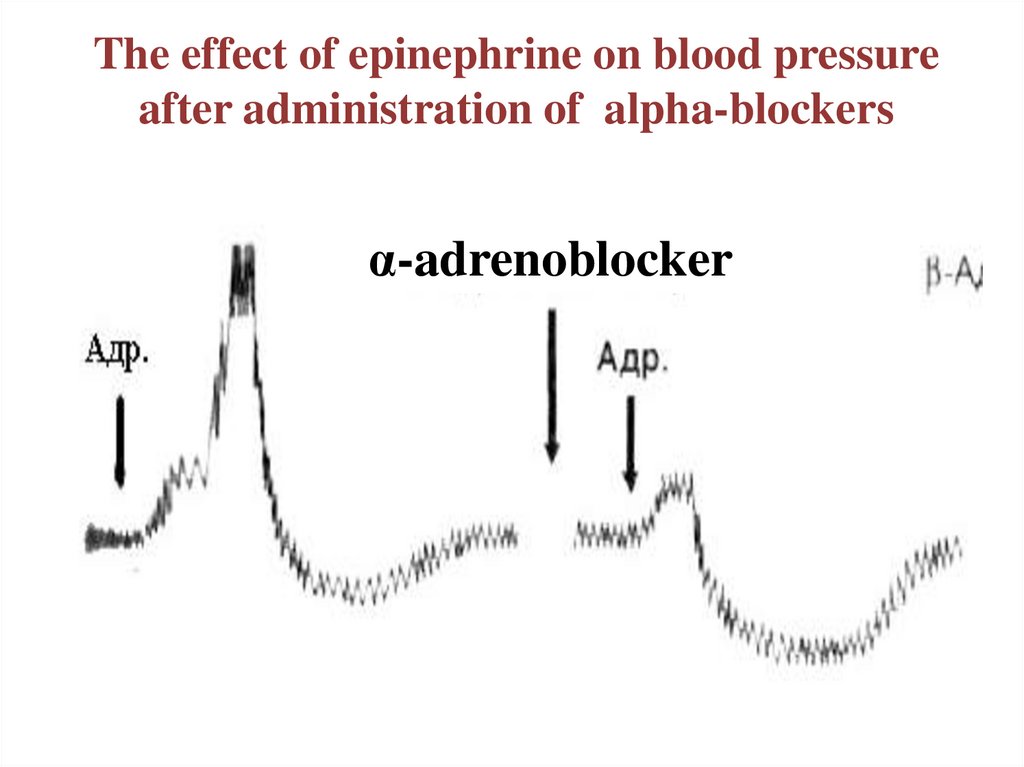
9. The effect of epinephrine on blood pressure after administration of alpha-blockers
α-adrenoblocker10.
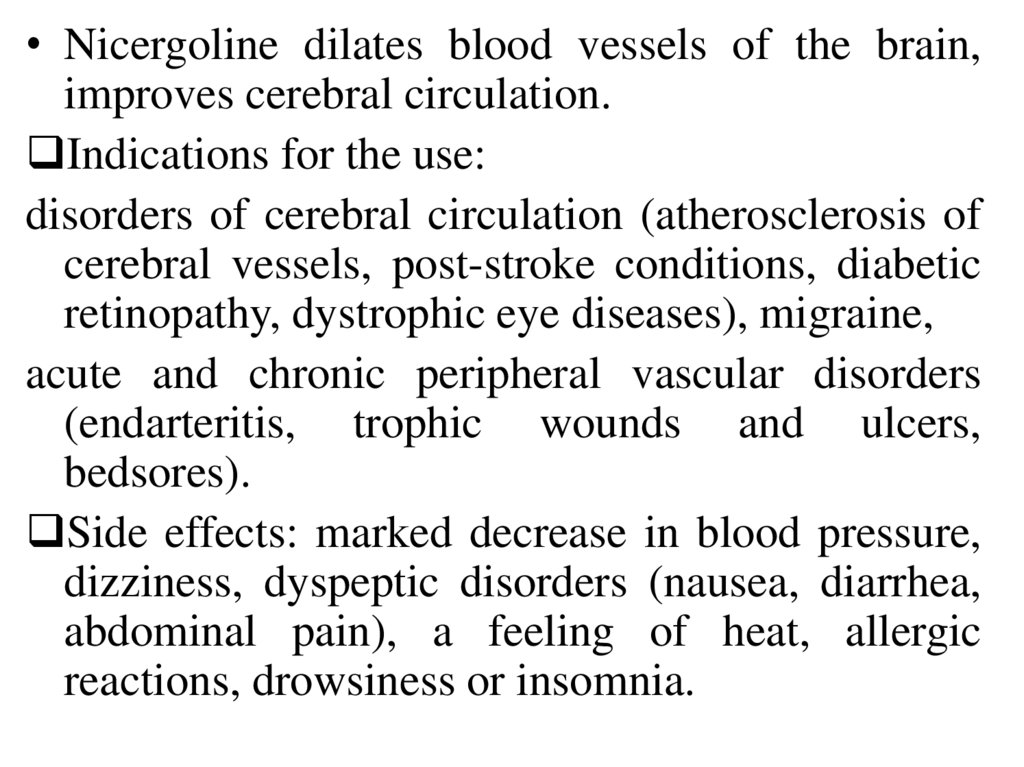
• Nicergoline dilates blood vessels of the brain,improves cerebral circulation.
Indications for the use:
disorders of cerebral circulation (atherosclerosis of
cerebral vessels, post-stroke conditions, diabetic
retinopathy, dystrophic eye diseases), migraine,
acute and chronic peripheral vascular disorders
(endarteritis, trophic wounds and ulcers,
bedsores).
Side effects: marked decrease in blood pressure,
dizziness, dyspeptic disorders (nausea, diarrhea,
abdominal pain), a feeling of heat, allergic
reactions, drowsiness or insomnia.
11.
12.
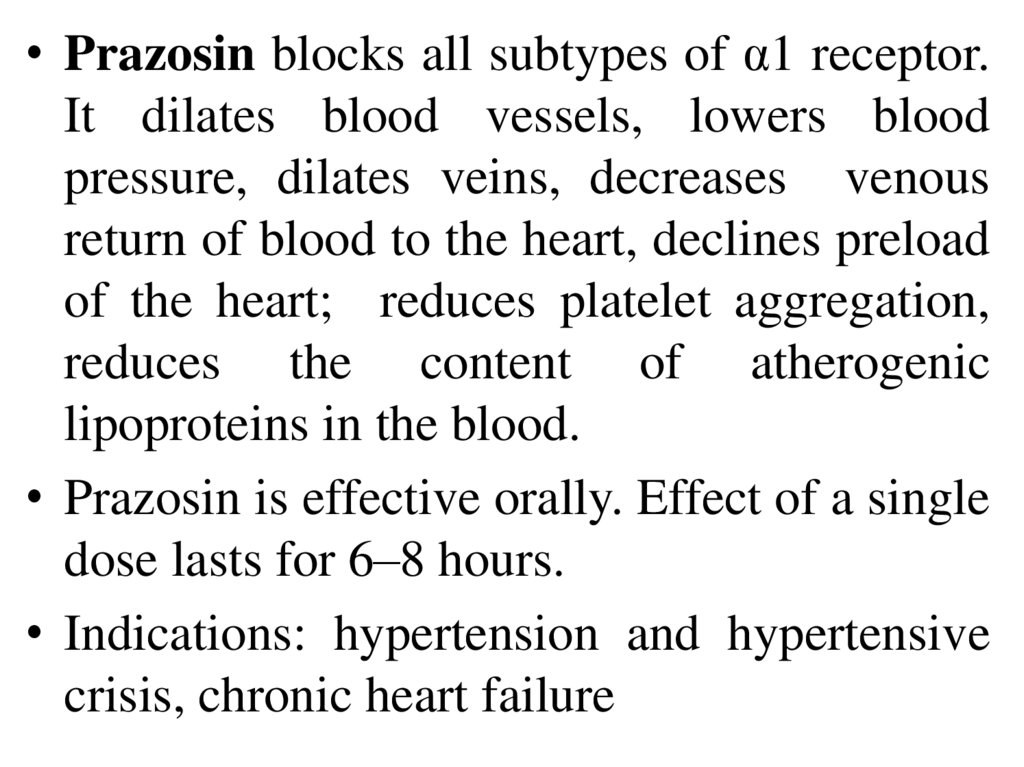
• Prazosin blocks all subtypes of α1 receptor.It dilates blood vessels, lowers blood
pressure, dilates veins, decreases venous
return of blood to the heart, declines preload
of the heart; reduces platelet aggregation,
reduces the content of atherogenic
lipoproteins in the blood.
• Prazosin is effective orally. Effect of a single
dose lasts for 6–8 hours.
• Indications: hypertension and hypertensive
crisis, chronic heart failure
13.
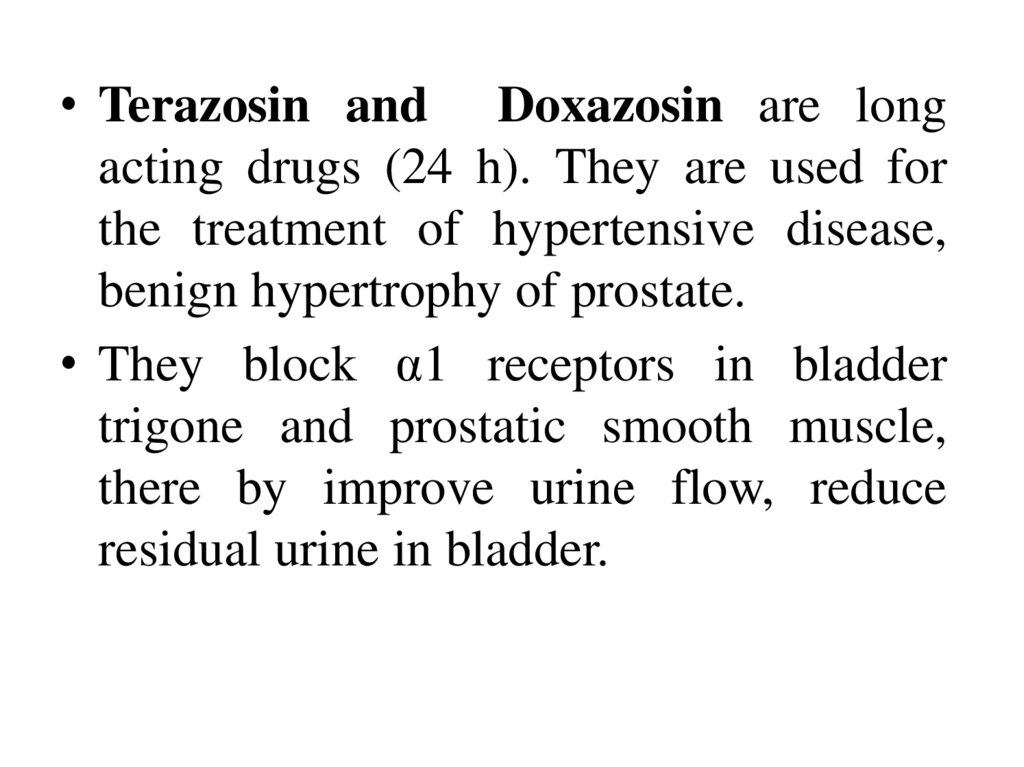
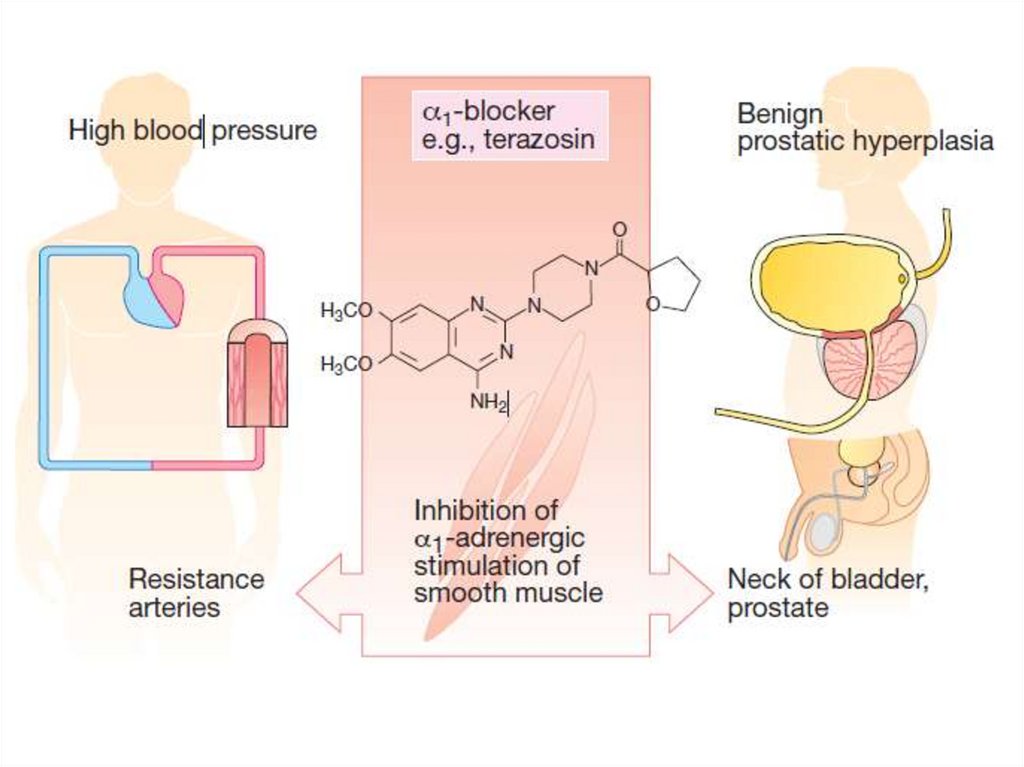
• Terazosin and Doxazosin are longacting drugs (24 h). They are used for
the treatment of hypertensive disease,
benign hypertrophy of prostate.
• They block α1 receptors in bladder
trigone and prostatic smooth muscle,
there by improve urine flow, reduce
residual urine in bladder.
14.
15.
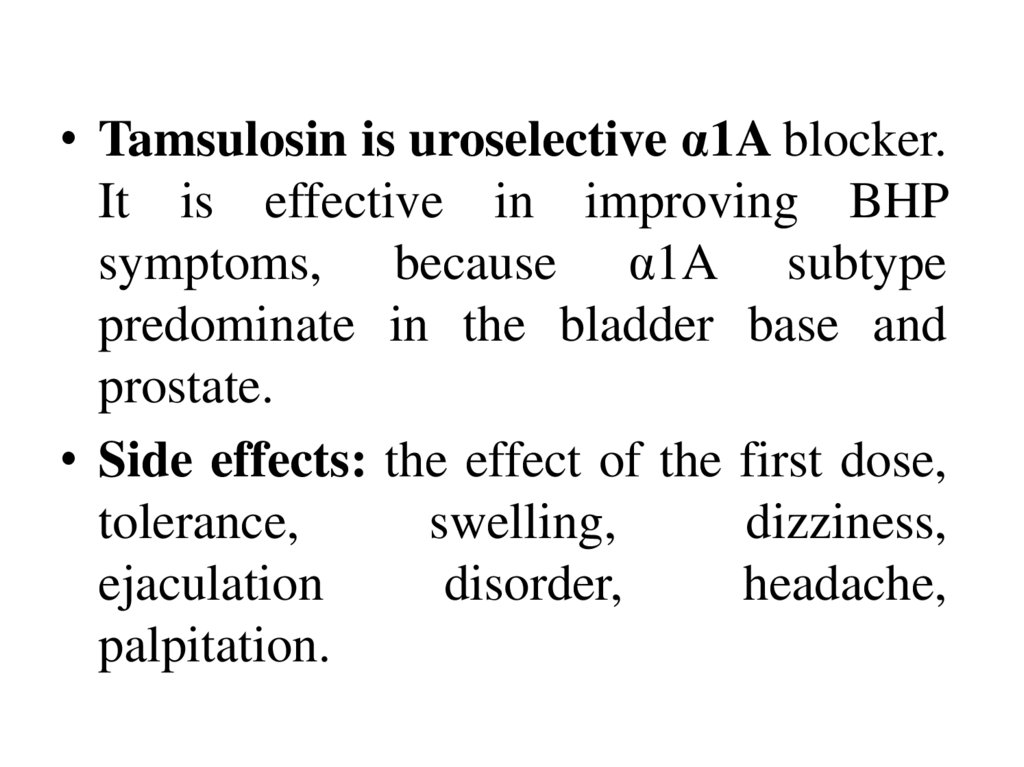
• Tamsulosin is uroselective α1A blocker.It is effective in improving BHP
symptoms, because α1A subtype
predominate in the bladder base and
prostate.
• Side effects: the effect of the first dose,
tolerance,
swelling,
dizziness,
ejaculation
disorder,
headache,
palpitation.
16.
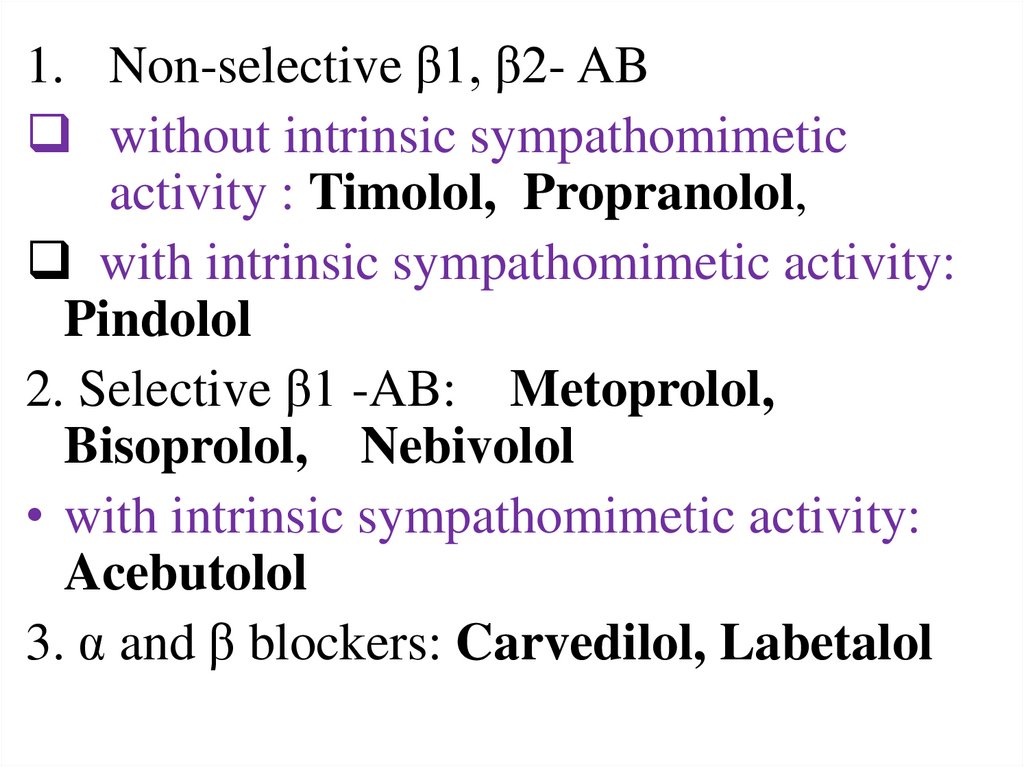
1. Non-selective β1, β2- ABwithout intrinsic sympathomimetic
activity : Timolol, Propranolol,
with intrinsic sympathomimetic activity:
Pindolol
2. Selective β1 -AB: Metoprolol,
Bisoprolol, Nebivolol
• with intrinsic sympathomimetic activity:
Acebutolol
3. α and β blockers: Carvedilol, Labetalol
17.
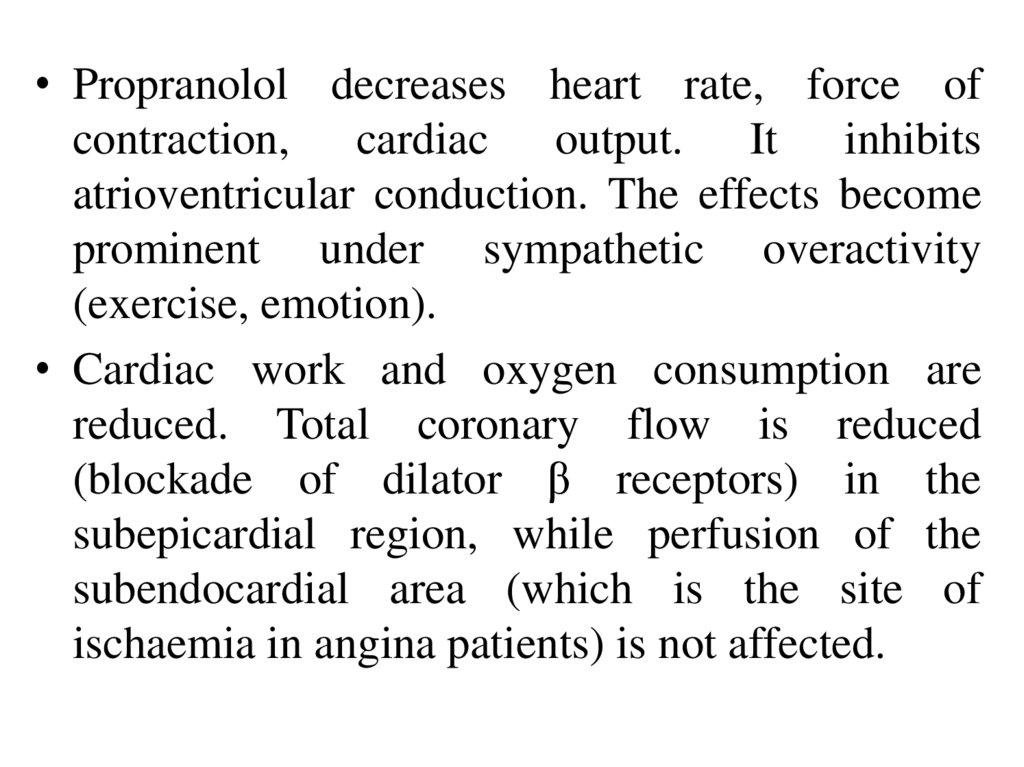
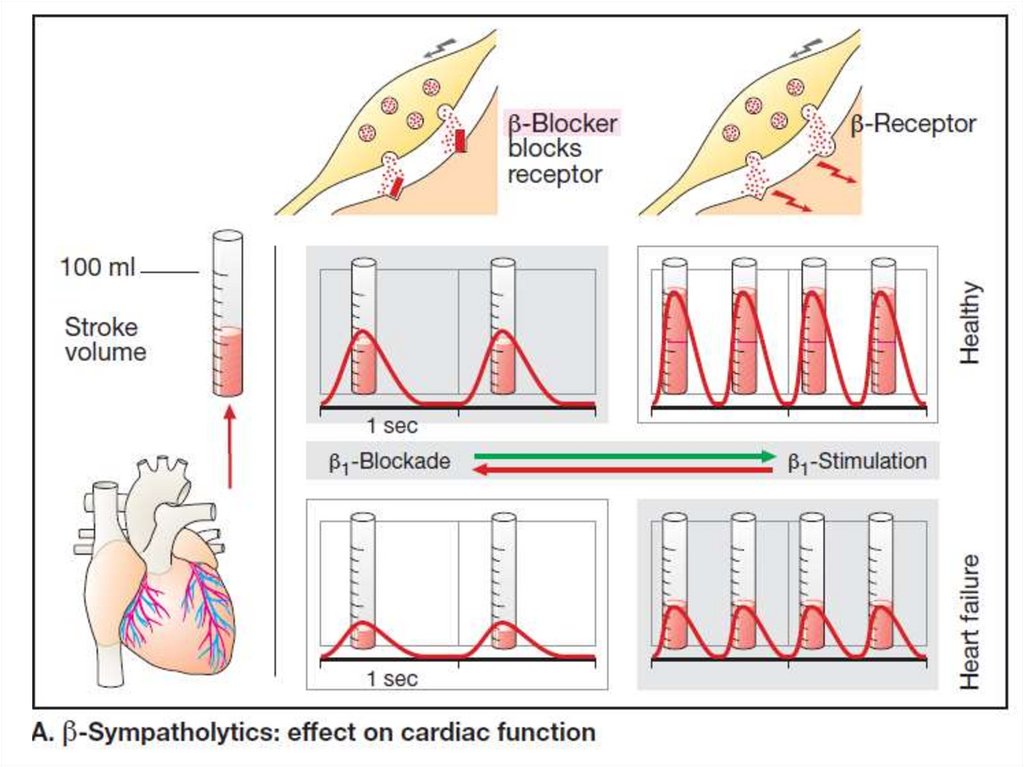
• Propranolol decreases heart rate, force ofcontraction, cardiac output. It inhibits
atrioventricular conduction. The effects become
prominent under sympathetic overactivity
(exercise, emotion).
• Cardiac work and oxygen consumption are
reduced. Total coronary flow is reduced
(blockade of dilator β receptors) in the
subepicardial region, while perfusion of the
subendocardial area (which is the site of
ischaemia in angina patients) is not affected.
18.
19.
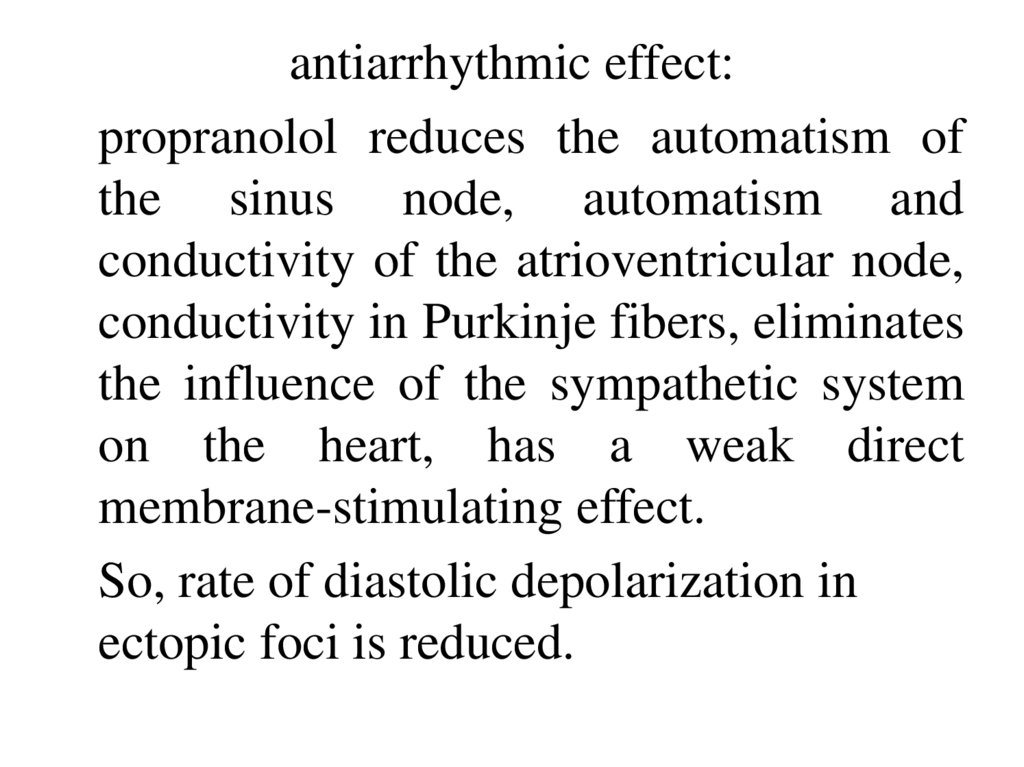
antiarrhythmic effect:propranolol reduces the automatism of
the sinus node, automatism and
conductivity of the atrioventricular node,
conductivity in Purkinje fibers, eliminates
the influence of the sympathetic system
on the heart, has a weak direct
membrane-stimulating effect.
So, rate of diastolic depolarization in
ectopic foci is reduced.
20.
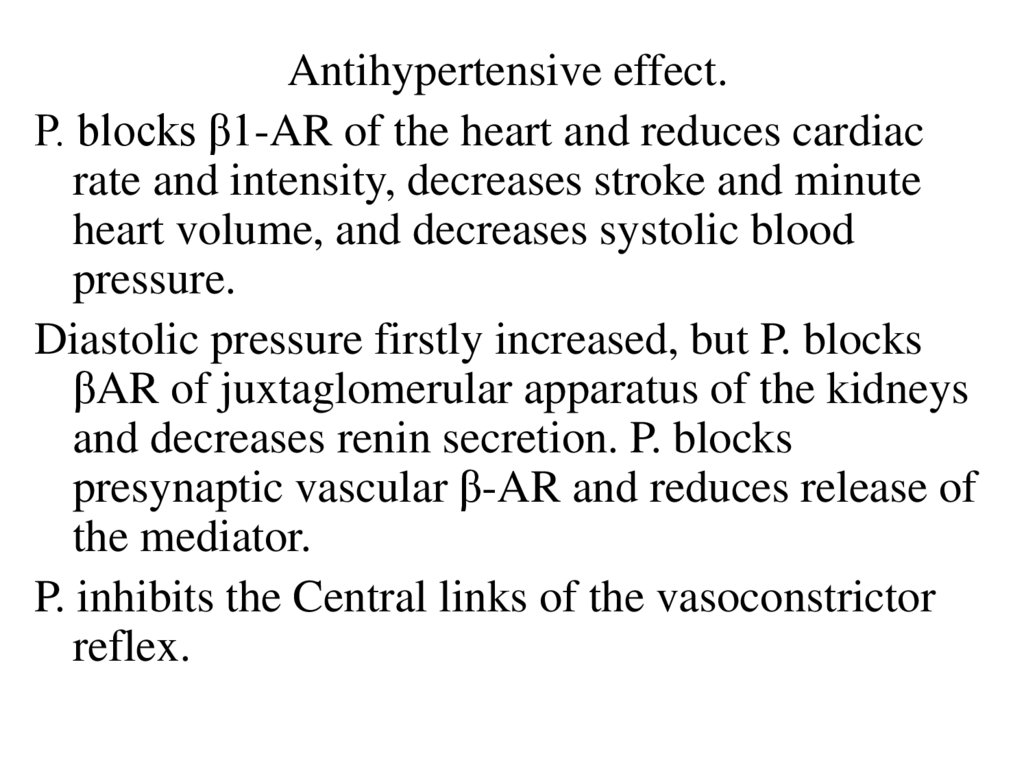
Antihypertensive effect.P. blocks β1-AR of the heart and reduces cardiac
rate and intensity, decreases stroke and minute
heart volume, and decreases systolic blood
pressure.
Diastolic pressure firstly increased, but P. blocks
βAR of juxtaglomerular apparatus of the kidneys
and decreases renin secretion. P. blocks
presynaptic vascular β-AR and reduces release of
the mediator.
P. inhibits the Central links of the vasoconstrictor
reflex.
21. The effect of epinephrine on blood pressure after administration of β-AB
β-adrenoblocker22.
Indication for use:angina pectoris,
hypertension
supraventricular tachycardia, atrial fibrillation,
tachycardia in mitral stenosis, thyrotoxicosis.
23.
Side effects:
cardiac failure, cardiac block, bronchospasm,
increase in peripheral vessels tone (numbness
of limbs, cold hands and feet),
increased hypoglycemia in patients with
diabetes mellitus, increased blood levels of
atherogenic lipoproteins,
drowsiness, lethargy, reduced reactions rate,
edema, dyspepsia, increasing the tone of the
uterus
24.
25.
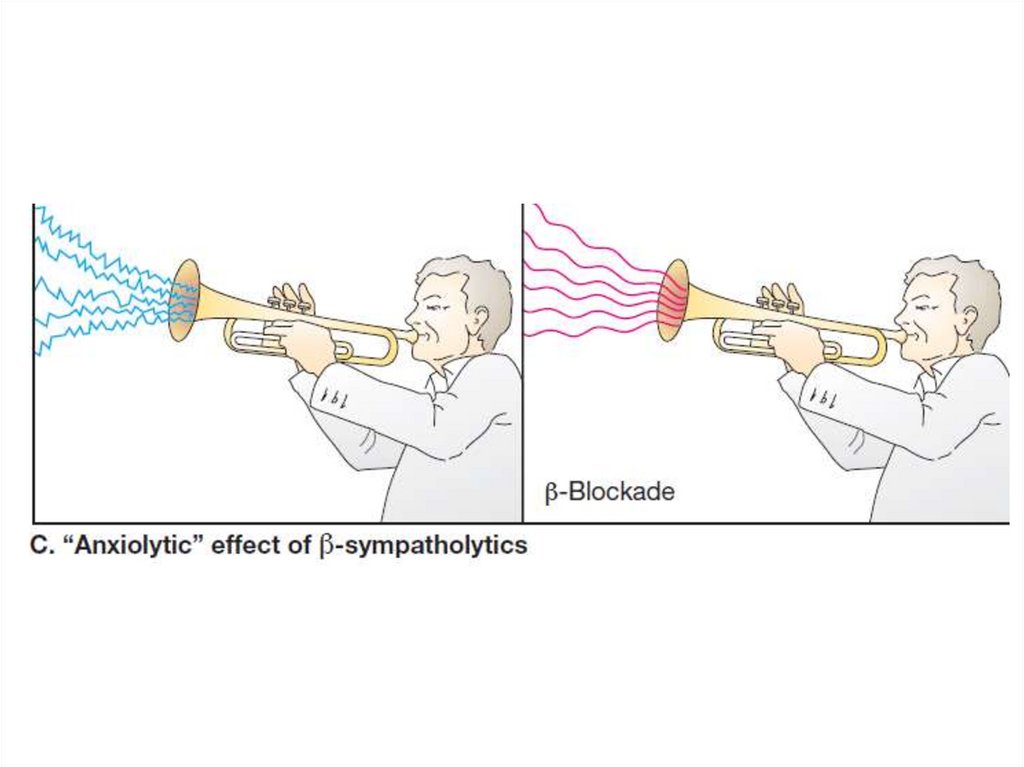
• Lipophilic substances penetrate the BBB,reduce fear, anxiety, panic, aggression, prevent
the activating effect of the Central nervous
system on the cardiovascular system. They can
be used for fear of public speaking, at stress.
• Propranolol inhibits adrenergically provoked
tremor.
• Propranolol and some other β blockers reduces
secretion of aqueous humor; intraocular
pressure is lowered.
26.
27.
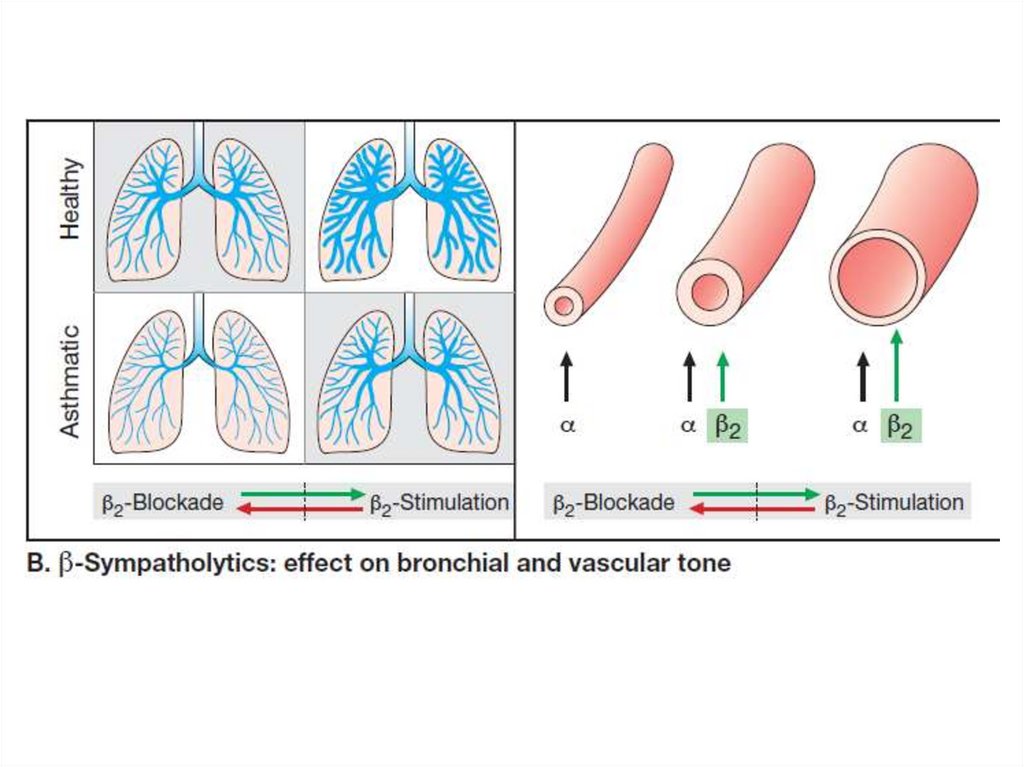
• Cardioselective b. are more potent in blockingcardiac (β1) than bronchial (β2) receptors.
However, selectivity is only relative and is lost at
high doses.
Their features are:
• Lower propensity to cause bronchoconstriction,
• Less interference with carbohydrate metabolism
and less inhibition of glycogenolysis during
hypoglycaemia—safer in diabetics.
• Lower incidence of cold hands and feet, Raynaud’s
phenomenon.
• No/less deleterious effect on blood lipid profile.
28.
Partialagonistic
(intrinsic
sympathomimetic) action (acebutolol).
These drugs themselves activate β1 and/or
β2 receptors submaximally.
The benefits of this property:
Bradycardia and depression of contractility
at rest are not prominent, but exercise
tachycardia is blocked.
They can be used in elderly patients, with sick
sinus.
29.
Pharmacokinetics• Lipophilic (propranolol, metoprolol) are
metabolized in the liver, undergoes
presystemic metabolism, pass through the
BBB
• Lipo / hydrophilic (bisoprolol, nebivolol,
carvedilol) are eliminated by kidneys and
liver.
• Hydrophilic (atenolol) are not metabolized
in the liver, excreted mainly by the kidneys.
30.
• Nebivolol is a highly selective β1 blocker. It alsoacts as a NO donor, produces vasodilatation and
improves endothelial function, which may delay
atherosclerosis.
• It has not effect on plasma lipids and on
carbohydrate metabolism.
• In contrast to older β blockers, hypotensive
response to nebivolol has a rapid onset. It is used
in hypertension and CHF.
31.
• Carvedilol is a β1 + β2 + α1adrenoceptor blocker. It reduces the work
of the heart, dilates blood vessels, reduces
the secretion of renin, reduces preload
and postload of the heart.
• It is used in hypertension, coronary artery
disease, chronic heart failure.
• Side effects: headache, bronchospasm,
allergic reactions.
It is used 1-2 times a day.
32.
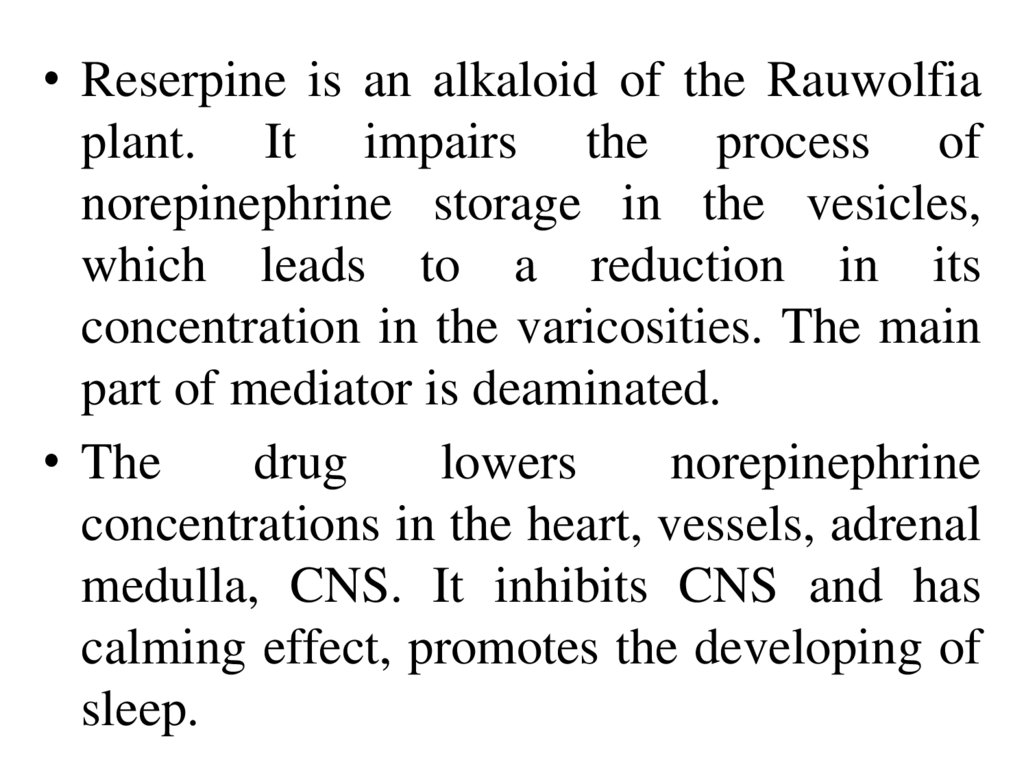
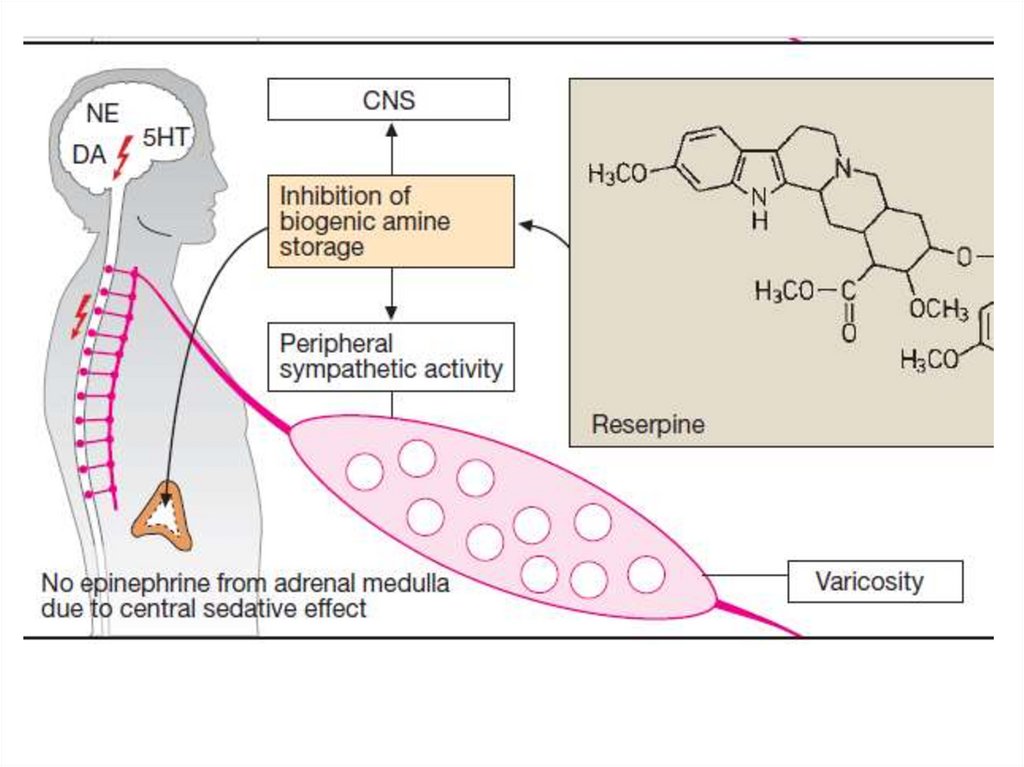
• Reserpine is an alkaloid of the Rauwolfiaplant. It impairs the process of
norepinephrine storage in the vesicles,
which leads to a reduction in its
concentration in the varicosities. The main
part of mediator is deaminated.
• The
drug
lowers
norepinephrine
concentrations in the heart, vessels, adrenal
medulla, CNS. It inhibits CNS and has
calming effect, promotes the developing of
sleep.
33.
34.
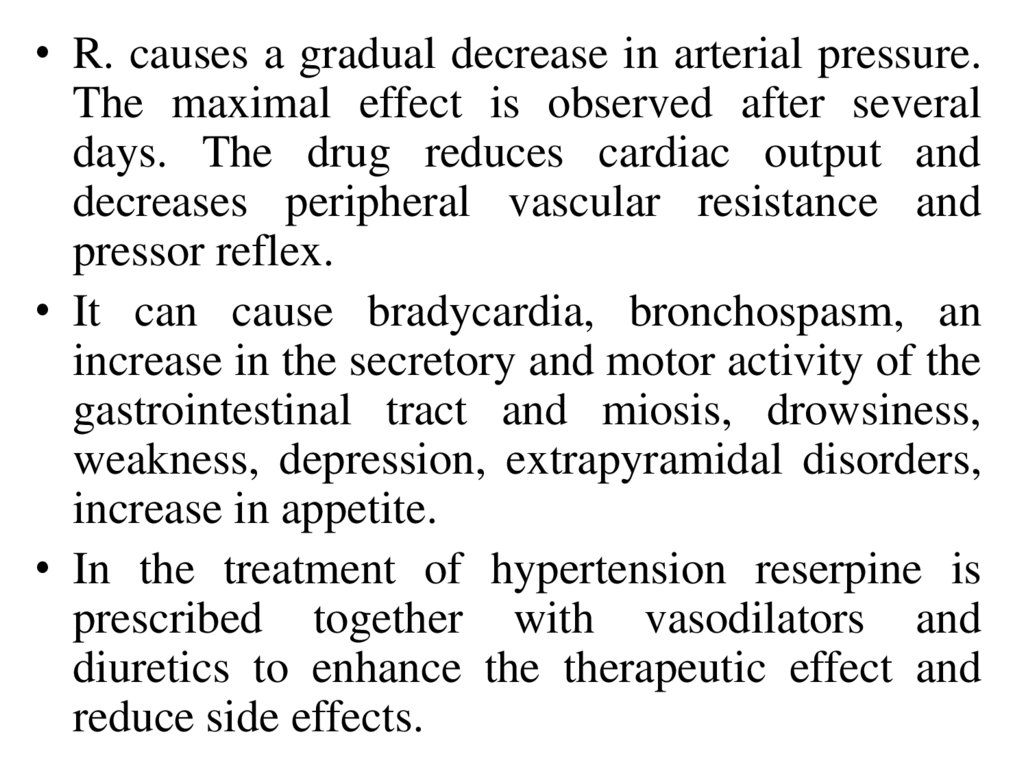
• R. causes a gradual decrease in arterial pressure.The maximal effect is observed after several
days. The drug reduces cardiac output and
decreases peripheral vascular resistance and
pressor reflex.
• It can cause bradycardia, bronchospasm, an
increase in the secretory and motor activity of the
gastrointestinal tract and miosis, drowsiness,
weakness, depression, extrapyramidal disorders,
increase in appetite.
• In the treatment of hypertension reserpine is
prescribed together with vasodilators and
diuretics to enhance the therapeutic effect and
reduce side effects.
35. Literature
1. Tripathi K.D. Essentials of Medical Pharmacology. Eighth Edition. -2019.- JaypeeBrothers Medical Publishers. The Health Sciences Publisher. -New Delhi. London. Panama
2. D.A.Kharkevich. Pharmacology. Textbook for medical students. Translation of 12th
edition of Russion textbook “Pharmacology” (2017). – М., ГЭОТАР-Медиа, 2017.
3. Review of pharmacology. Gobind Rai Garg, Sparsh Gupta. 13th edition. - 2019.- Jaypee
Brothers Medical Publishers. The Health Sciences Publisher. -New Delhi. London. Panama
4. Whalen Karen. Lippincott Illustrated Reviews: Pharmacology. Sixth Edition. - Wolters
Kluwer. - 2015.-Philadelphia
5. Color Atlas of Pharmacology. 2nd edition, revised and expanded. Heinz Lüllmann.- 2000
Thieme
6. Pharmacology Examination & Board Review. Tenth Edition. Trevor Anthony J.,
Katzung Bertram G., Kruidering-Hall Marieke, Susan B. Masters. - a LANGE medical
book. - 2013.-New York
7. Medical Pharmacology at a Glance. Eighth Edition. Neal Michael J. – 2016. John Wiley
& Sons, Ltd.
8. USMLE Step 1. Lecture Notes. Pharmacology. Lionel P.Raymon and others.- Kaplan
Medical.Inc. -2009





 medicine
medicine