Similar presentations:
Рain-relieving drugs
1. PAIN-RELIEVING DRUGS
ANALGESICS - are drugs thatselectively inhibit pain sensitivity. They
do not affect consciousness and do not
inhibit other types of sensitivity.
2.
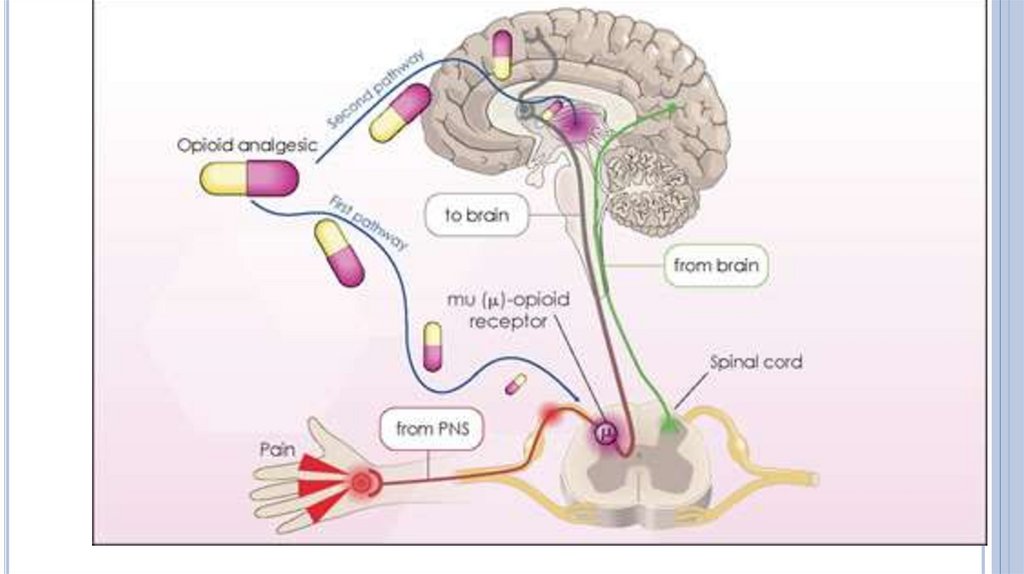
Damageto tissue causes the release of chemicals (e.g.
bradykinin, prostaglandins, adenosine triphosphate, protons)
that stimulate pain receptors or nociceptors. They are located
on the endings of afferent fibers in the skin, muscles, visceral
organs.
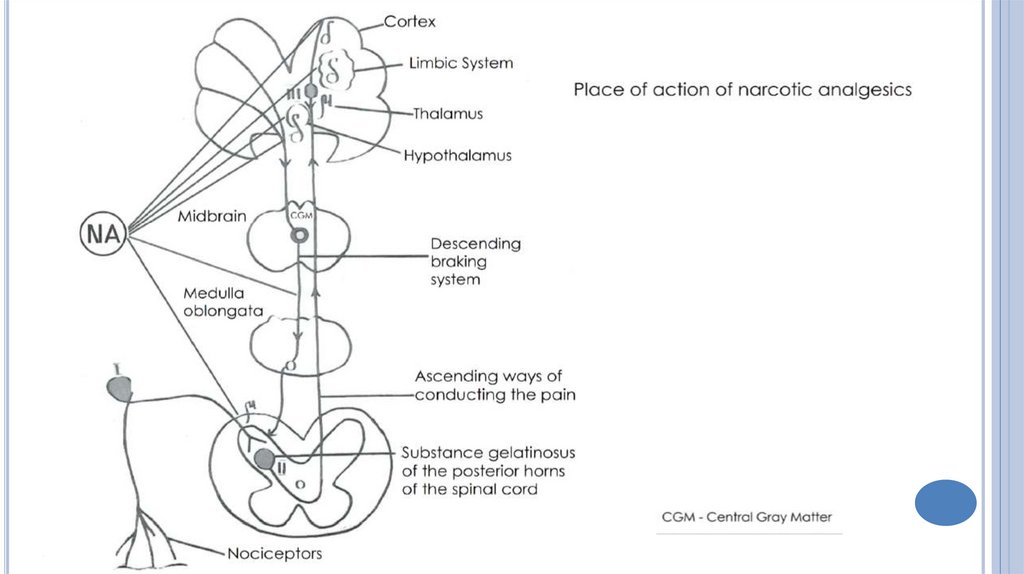
Impulses, caused by painful stimuli, spread along the C and A
fibers and enter the posterior horn of the spinal cord. The first
synaptic transmission from the afferent fibers to the
interneurons takes place. Impulses spread along a number of
pathways: to the higher CNS centers – reticular formation,
thalamus, hypothalamus, basal ganglia, limbic system,
cerebral cortex.
3.
Thesecond pathway is transmission of impulses to the
motorneurons of the spinal cord, which is manifestered by
the motor reflex.
The third pathway is provided by the excitation of the
lateral horn neurons, leading to the activation of the
adrenergic (sympathetic) innervation.
4.
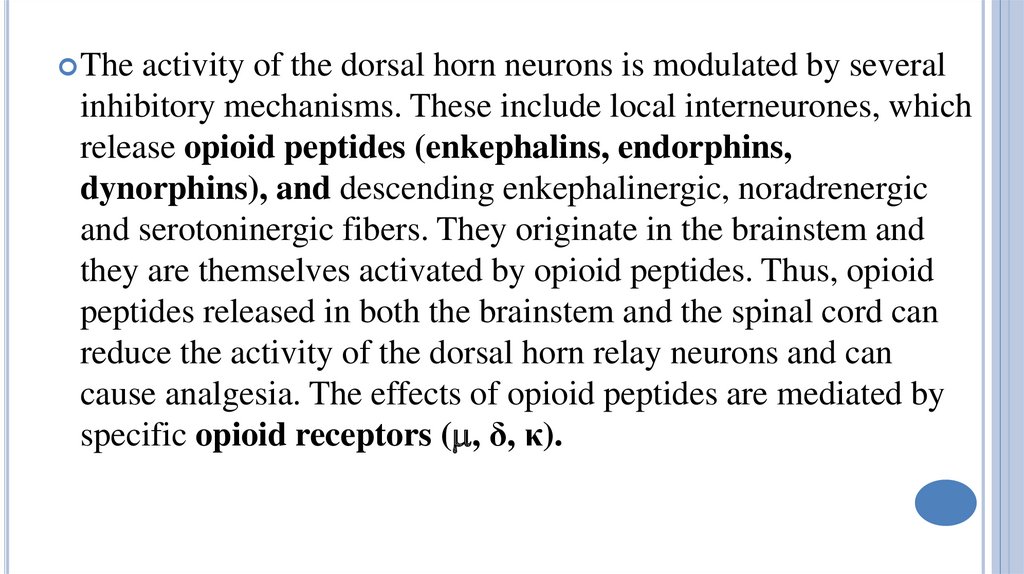
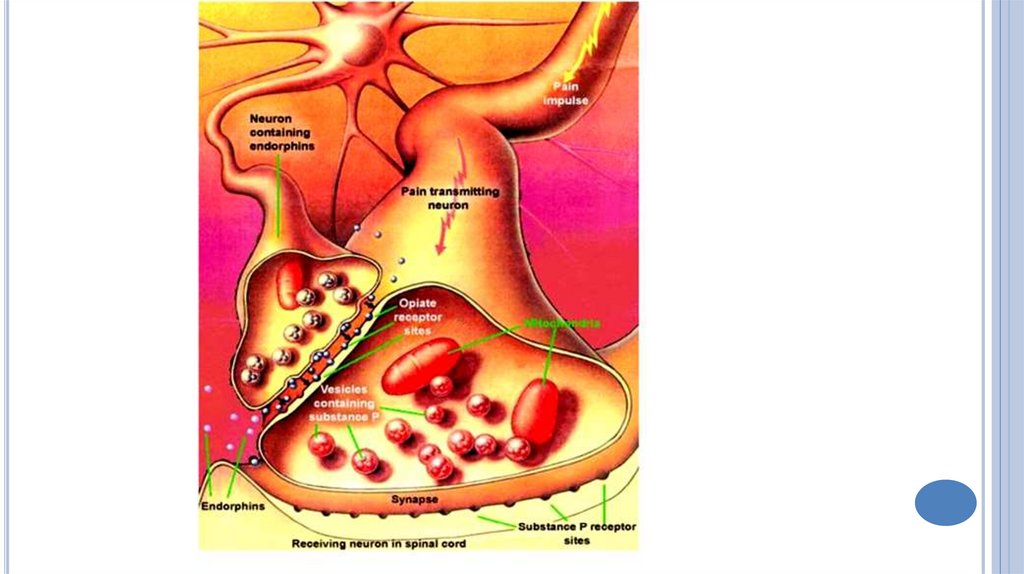
Theactivity of the dorsal horn neurons is modulated by several
inhibitory mechanisms. These include local interneurones, which
release opioid peptides (enkephalins, endorphins,
dynorphins), and descending enkephalinergic, noradrenergic
and serotoninergic fibers. They originate in the brainstem and
they are themselves activated by opioid peptides. Thus, opioid
peptides released in both the brainstem and the spinal cord can
reduce the activity of the dorsal horn relay neurons and can
cause analgesia. The effects of opioid peptides are mediated by
specific opioid receptors ( , δ, κ).
5.
6.
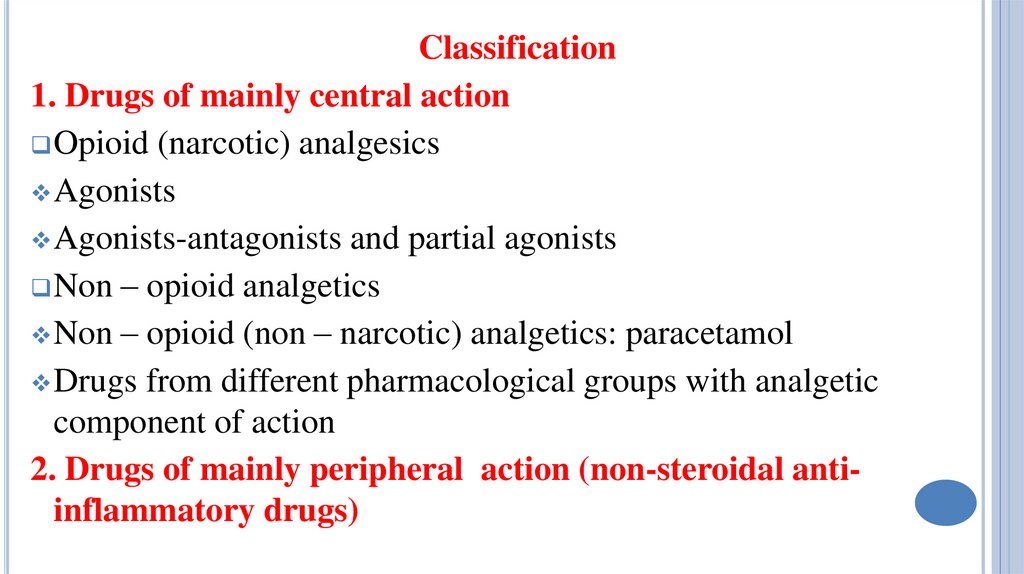
Classification1. Drugs of mainly central action
Opioid (narcotic) analgesics
Agonists
Agonists-antagonists and partial agonists
Non – opioid analgetics
Non – opioid (non – narcotic) analgetics: paracetamol
Drugs from different pharmacological groups with analgetic
component of action
2. Drugs of mainly peripheral action (non-steroidal antiinflammatory drugs)
7.
Opioidanalgesics are drugs that mimic endogenous
opioid peptides by causing a prolonged activation of
opioid receptors (usually μ‐receptors).
Opioid analgesics produce marked inhibitory effect on
the CNS. These include analgesia, drowsiness,
antitussive action. Most of them change mood (euphoria)
and cause drug dependence (psychological and
physical). Some of them are derived from plants and
some are synthesized.
8. Morphin is alkaloid of opium.
MORPHIN IS ALKALOID OF OPIUM.Papaver Somniferum
9.
Opium,selected for medical use, has to contain no
less than 10% morphine. Opium contains more than
20 alkaloids. According to the chemical structure,
some alkaloids are phenanthrene derivatives, other
- isoquinoline derivatives.
Phenanthrene derivatives are morphine, codeine.
Isoquinoline derivatives is papaverin
(antispasmodic drug).
10.
Agonistsof opioid receptors:
morphine, trimeperidine, fentanyl, codeine.
Agonist-antagonist and partial agonists:
buprenorphine, nalbuphine, butorphanole.
Antagonist of opioid receptors:
naloxone, naltrexone
11.
The mechanism of morphine analgesic action:1. Inhibition of neurotransmission of pain stimuli in
the central part of the afferent pathway.
2. Impairment of subjective emotional perception of
pain, pain assessment and reaction to it.
12.
Stimulation of opioid receptors by morphine leads tothe activation of antinociceptive system and
disturbance of interneuronal transmission of pain
stimuli on different levels of the CNS.
Suppressive effect of morphine on the painful stimuli
transmission in the spinal cord from the primary
afferent fibers to the interneurones results from an
increase of descending inhibitory effects and direct
inhibitory action on the interneuronal transmission.
13.
14.
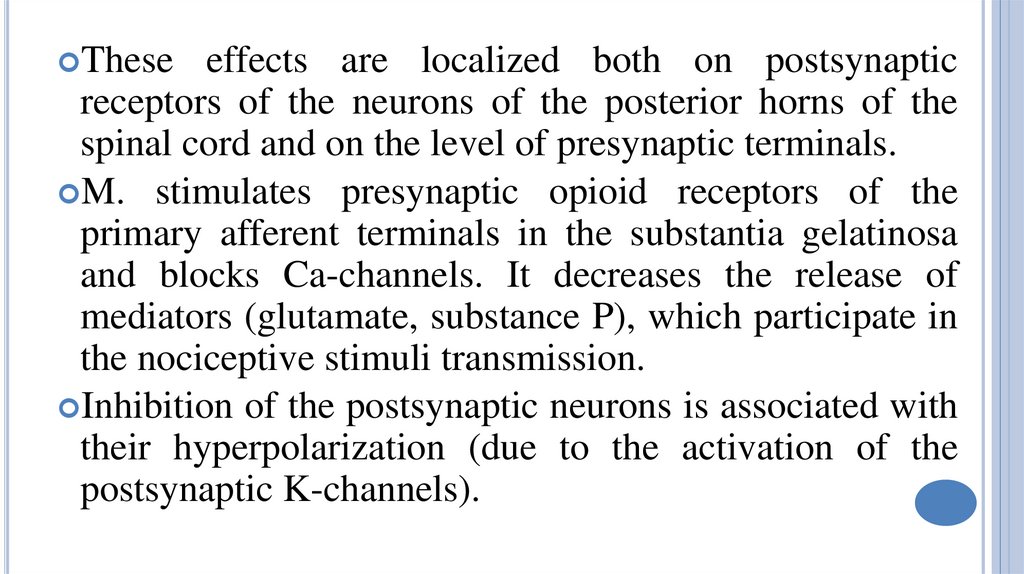
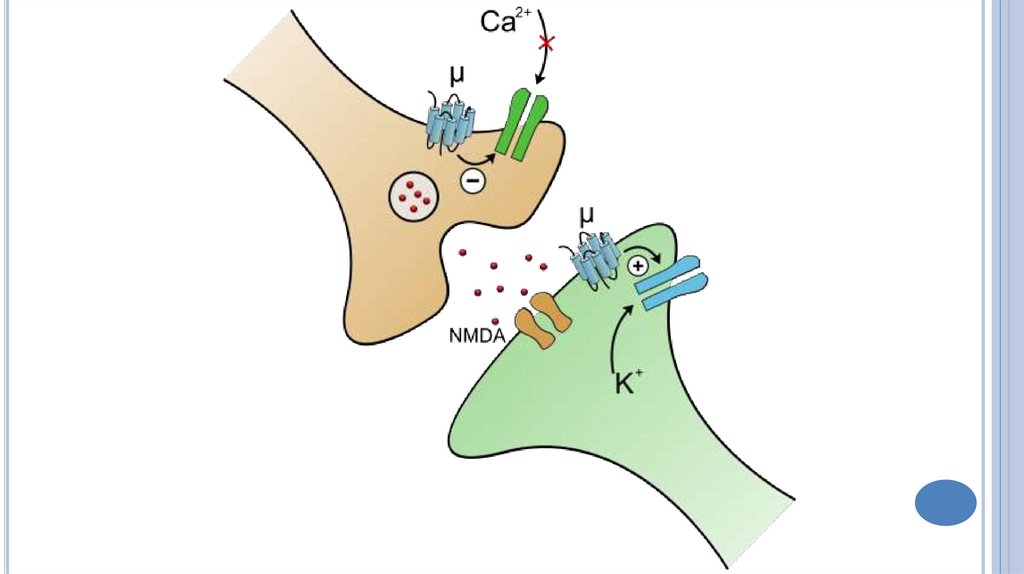
Theseeffects are localized both on postsynaptic
receptors of the neurons of the posterior horns of the
spinal cord and on the level of presynaptic terminals.
M. stimulates presynaptic opioid receptors of the
primary afferent terminals in the substantia gelatinosa
and blocks Ca-channels. It decreases the release of
mediators (glutamate, substance P), which participate in
the nociceptive stimuli transmission.
Inhibition of the postsynaptic neurons is associated with
their hyperpolarization (due to the activation of the
postsynaptic K-channels).
15.
16.
17.
Depressionof the interneuronal transmission in the
spinal cord lowers impulse intensity in the
ascending afferent pathways and decreases motor
and autonomic responses.
M. blocks the transmission of pain in the thalamus,
reduces the summation of the pain impulses, and
increases pain threshold.
The sedation action of M. changes pain perception
and its emotional assessment also.
18.
19.
IndicationsAcute pain
Severe trauma, extensive burns,
Myocardial infarction, painful manipulation, birth;
Colic (renal, biliary, intestinal) – together with
antispasmodic (atropine and papaverine);
For sedation in anesthesia and in the postoperative period;
Neuroleptanalgesia, ataralgesia;
Chronic pain in incurable oncologic patients.
20. OTHER EFFECTS
Euphoria,which entails better mood, sensation of
psychological comfort, positive views of the surrounding
environment, a feeling that future is bright, irrespective
of reality. Some individuals develop an opposite effect:
feeling bad, negative emotions.
Sleep is usually superficial and easily interrupted by
external stimuli.
Decrease of the body temperature (inhibition of the
thermoregulation center, located in the hypothalamus).
21.
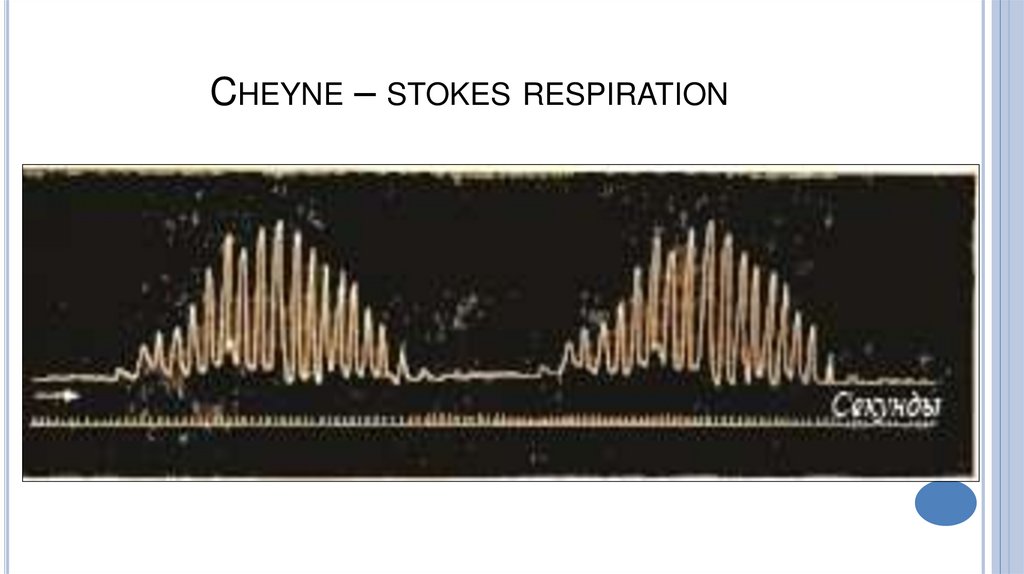
– excitation of the oculomotor center.M. inhibits the respiratory center of the medulla
oblongata and decreases its excitation in response to
carbon dioxide and reflex reactions. The respiratory rate
slows down, but amplitude increases.
With a higher dose, respiratory rhythm decreases even
more, the amplitude and minute volume decreases also.
Irregular respiratory rhythm occurs; periodic respiration
is possible.
Miosis
22. Cheyne – stokes respiration
CHEYNE – STOKES RESPIRATION23.
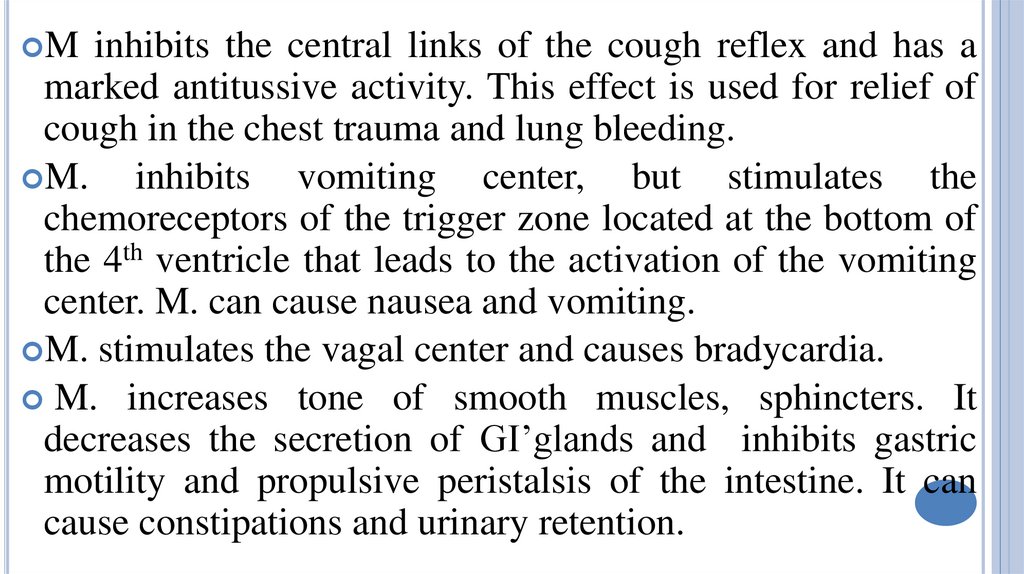
Minhibits the central links of the cough reflex and has a
marked antitussive activity. This effect is used for relief of
cough in the chest trauma and lung bleeding.
M.
inhibits vomiting center, but stimulates the
chemoreceptors of the trigger zone located at the bottom of
the 4th ventricle that leads to the activation of the vomiting
center. M. can cause nausea and vomiting.
M. stimulates the vagal center and causes bradycardia.
M. increases tone of smooth muscles, sphincters. It
decreases the secretion of GI’glands and inhibits gastric
motility and propulsive peristalsis of the intestine. It can
cause constipations and urinary retention.
24. contraindications
CONTRAINDICATIONSEarly
children up to 3 years old;
The elderly;
Pregnancy, childbirth (with the exception of
trimeperidin);
Different types of respiratory failure;
Severe head injury
Remember: tolerance (including cross-tolerance) and
drug dependence develops with all agonists of opioid
receptors.
25.
Trimeperidineis less active than m. The duration
of action is 3-4 hours.
T. depresses the respiratory center to a lesser
degree than m.
It decreases the tone of the smooth muscles organs
(ureters and bronchi), but also increases it
(intestine, bile ducts). It is inferior to m. in its
spasmogenic effect. It slightly intensifies
contractility of the myometrium.
26. fentanyl
FENTANYL27.
Fentanylis more active than M. (by 100-400 times).
Duration of pain relief is about 20-30 minutes after iv
administration.
But duration of action after application of transdermal
system is more than 72 hours.
F. causes a marked depression of the respiratory tract.
It increases the tone of the thoracic muscles. This
worsens pulmonary ventilation.
Talamonal is the combination of F. and droperidole.
28. Buprenorphine
BUPRENORPHINE29.
is a partial agonist of -receptors. It surpassesm. by 20-60 times in its analgesic activity and also
has a longer action. The effect develops slower
than the effect of M.
It affects the gastrointestinal tract less than m.
Dependence potential is relatively low. The drug
causes abstinence less than morphin.
B.
30. butorphanole - is an agonist of δ and κ –receptors, but weak antagonist of -receptors.
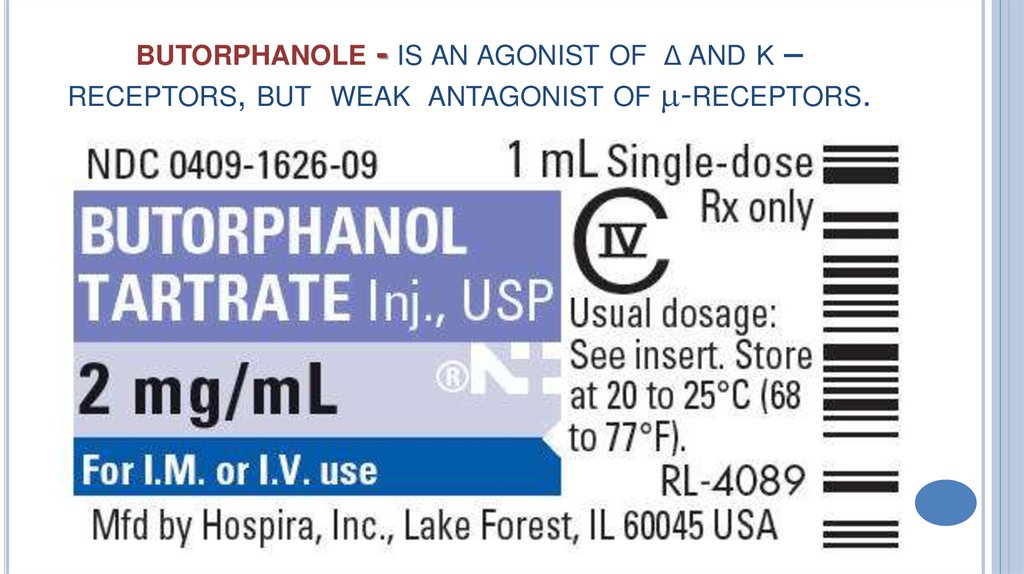
BUTORPHANOLE- IS AN AGONIST OF
RECEPTORS, BUT WEAK ANTAGONIST OF
Δ AND Κ
–
-RECEPTORS.
31.
Itis 3-5 times more active
than m.
It increases pulmonary artery
pressure and cardiac work
and is not recommended for
use in myocardial infarction.
Depresses respiration to a
less degree than M.
Causes drug addiction more
rarely.
32. Nalbuphine -is an agonist of δ and κ –receptors, but weak antagonist of -receptors.
NALBUPHINE -IS AN AGONIST OF Δ AND Κ –RECEPTORS,BUT WEAK ANTAGONIST OF -RECEPTORS.
It
is similar to M. in its
activity.
It rarely causes drug
dependence.
It has almost no effect on
hemodynamic.
33. symptoms of acute poisoning
SYMPTOMS OF ACUTE POISONINGA loss
of consciousness progressing into coma.
Irregular and periodic respiration;
Skin is pale, cold and moist, and the mucous
membranes are cyanotic.
Marked miosis;
Bradycardia;
Increased knee-jerk.
Body temperature is falling.
34. Treatment of acute poisoning
TREATMENT OF ACUTE POISONINGGastric
lavage (KMnO4);
Administration of adsorbents and saline laxatives
(MgSO4) .
Special antagonists are used. They block all types of
opioid receptors, and eliminate all effects of N.A.
Antagonists are naloxone and naltrexone.
35. Drug dependence
DRUG DEPENDENCENA cause euphoria. The unpleasant emotions and tiredness are
eliminated, and good mood, self-reliance appears.
Abrupt discontinuation of the administration of the drug results in
withdrawal syndrome (abstinence).
Fear, anxiety, depression, sleeplessness, aggressiveness appear.
Most physiologic functions are disturbed. Sometimes collapse
occurs; in severe cases abstinence can be the cause of lethal
outcome.
Introduction of NA eliminates withdrawal syndrome.
Symptoms of chronic poisoning: decreasing of mental and physical
abilities, weight loss, thirst, constipation, hair loss.
36.
– is analgetic with mixed mechanism ofaction. It interacts with opioid receptors. It reduces the
neuronal uptake of serotonin and norepinephrine and so
intensifies spinal inhibitory serotoninergic and
adrenergic effects on the interneuronal transmission of
the nociceptive impulses.
It minimally affects respiration and gastrointestinal
functions.
Dependence potential is much lower than for opioid
receptors agonists.
Tramadol




 medicine
medicine