Similar presentations:
Cardiogenic shock: the causes, mechanisms, pathophysiological stages
1.
SIWModule: “Cardio-vascular system”
Theme: “Cardiogenic shock: the causes,
mechanisms, pathophysiological stages”
2. Plan
IntroductionEtiology
Pathogenesis and mechanisms
Forms of cardiogenic shock
Conclusion
References
3. Introduction
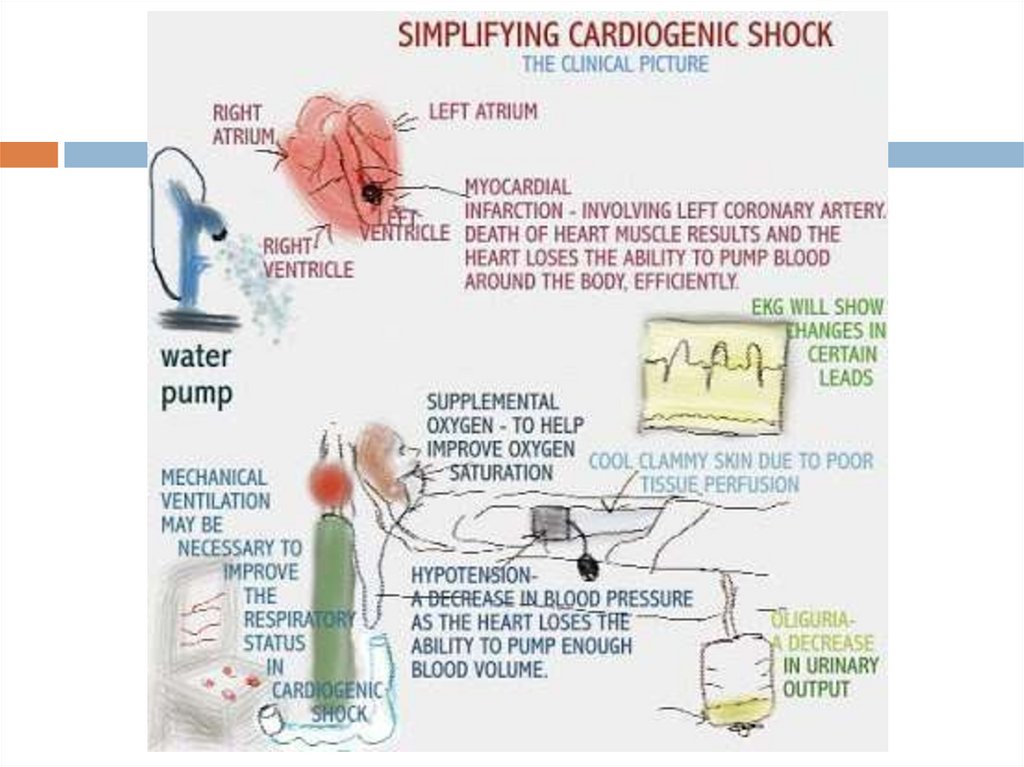
Cardiogenic shock - an extreme degree of leftventricular failure, characterized by a sharp
decrease in myocardial contractility (falling
ejection stroke and minute), which is not
compensated by an increase in vascular resistance
and leads to an inadequate blood supply to all
organs and tissues, primarily - the vital organs.
Most often, it develops as a complication of
myocardial infarction, myocarditis or less
cardiotoxic substances poisoning
4. There are four mechanisms that cause shock:
Upset pumping function of theheart muscle;
Severe cardiac arrhythmias;
Effusion or tamponade
ventricular bleeding heart bag;
Massive pulmonary embolism as
a special form of CABG.
5.
6. Etiology
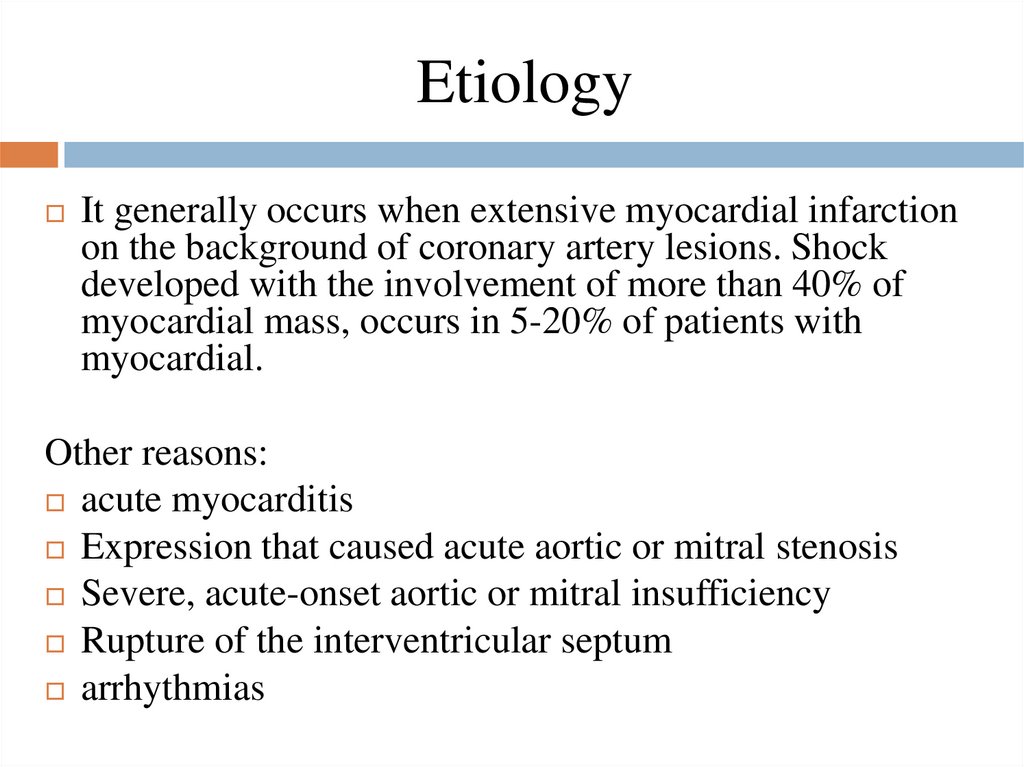
It generally occurs when extensive myocardial infarctionon the background of coronary artery lesions. Shock
developed with the involvement of more than 40% of
myocardial mass, occurs in 5-20% of patients with
myocardial.
Other reasons:
acute myocarditis
Expression that caused acute aortic or mitral stenosis
Severe, acute-onset aortic or mitral insufficiency
Rupture of the interventricular septum
arrhythmias
7.
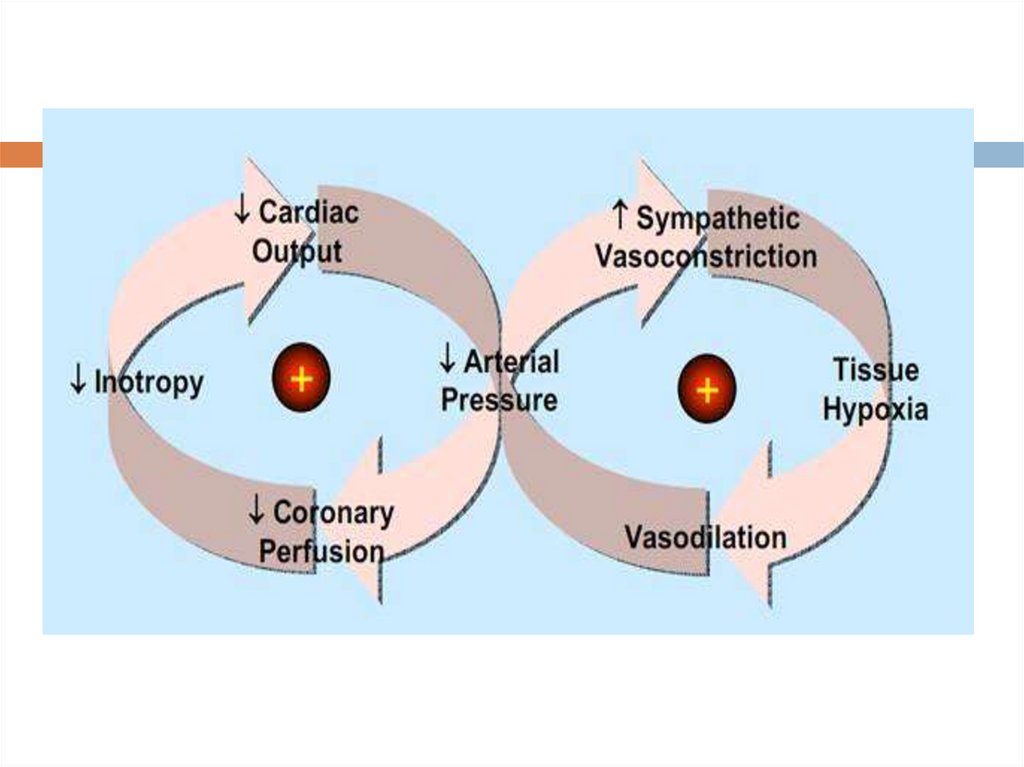
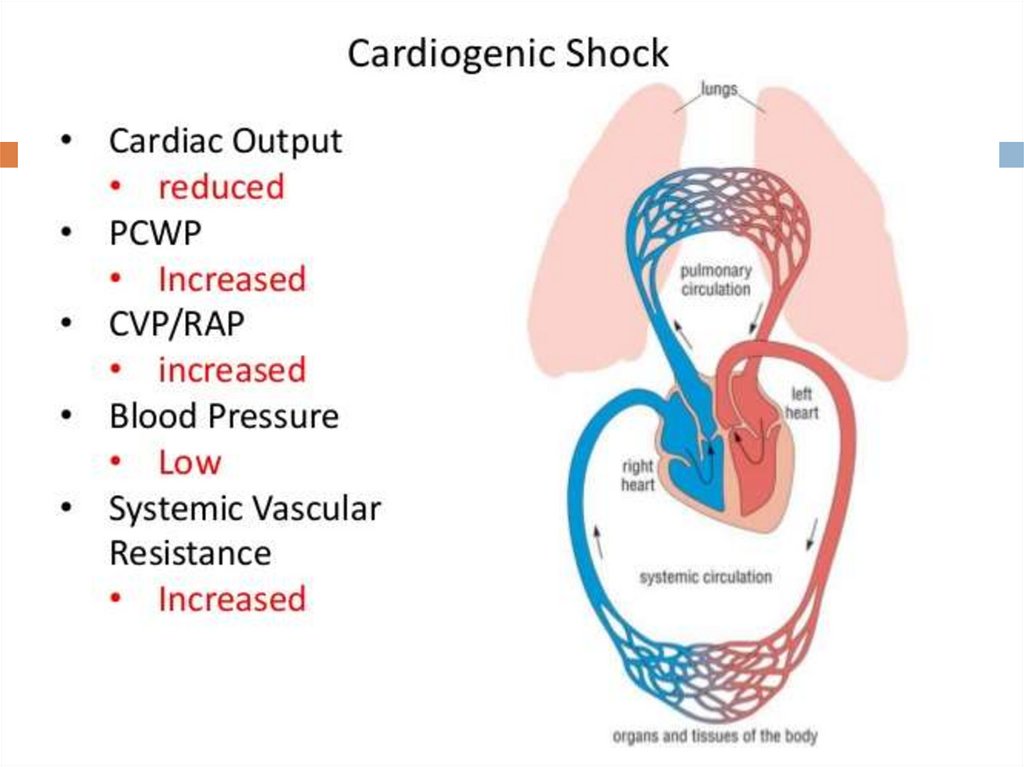
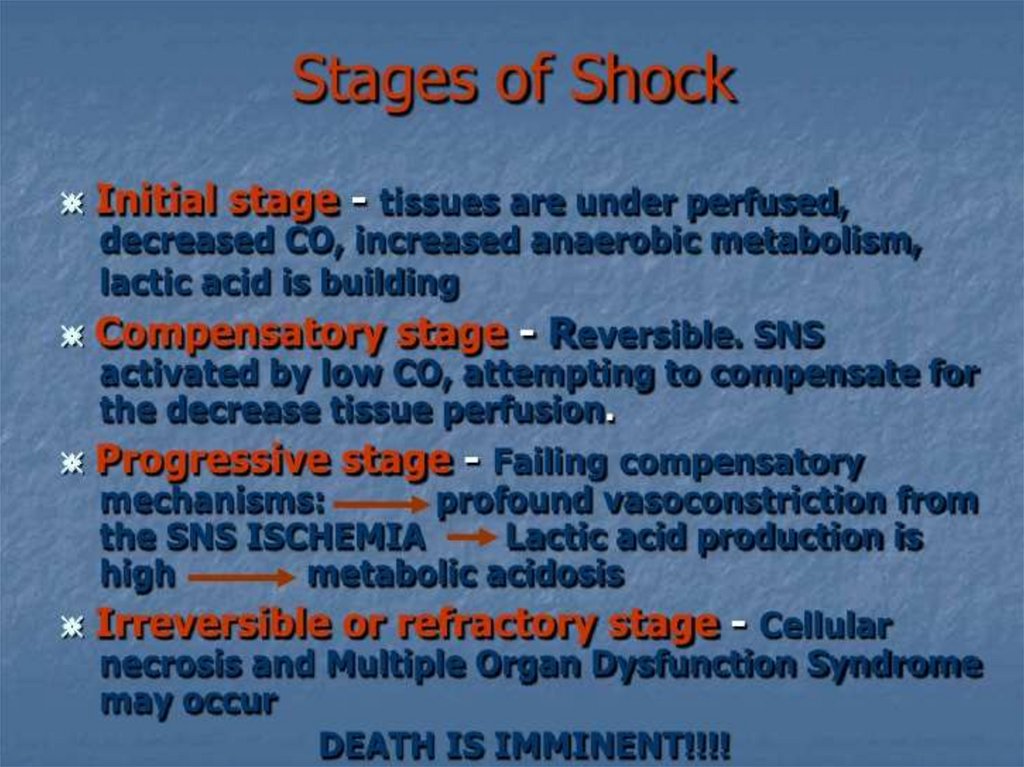
8. Pathophysiology
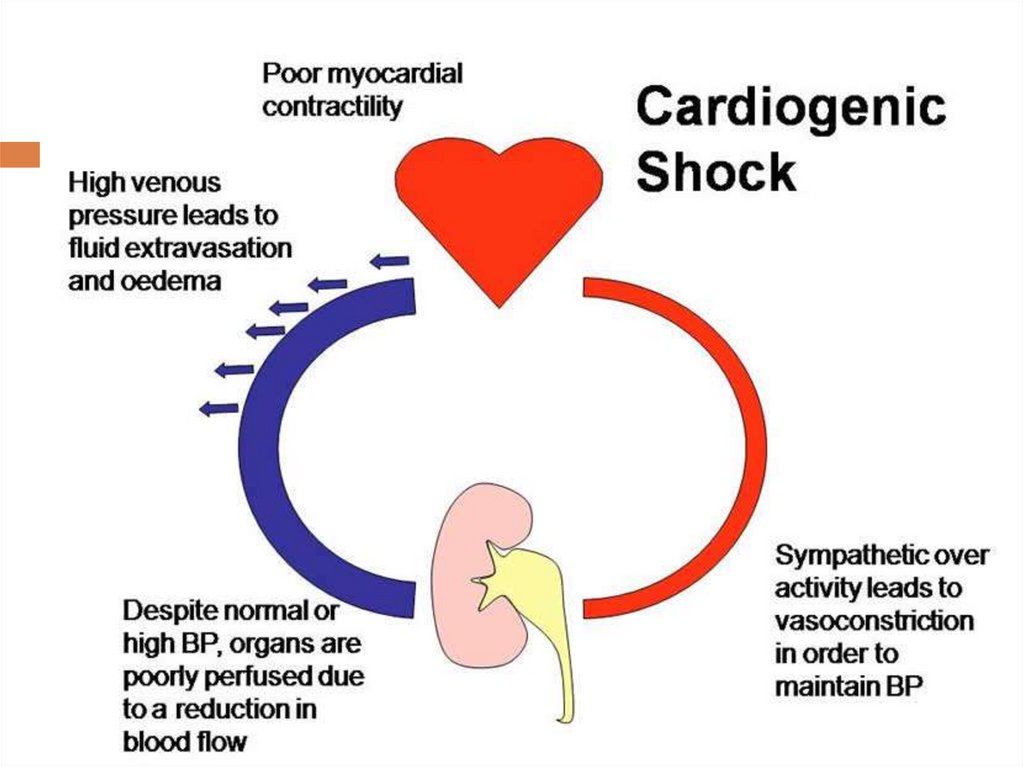
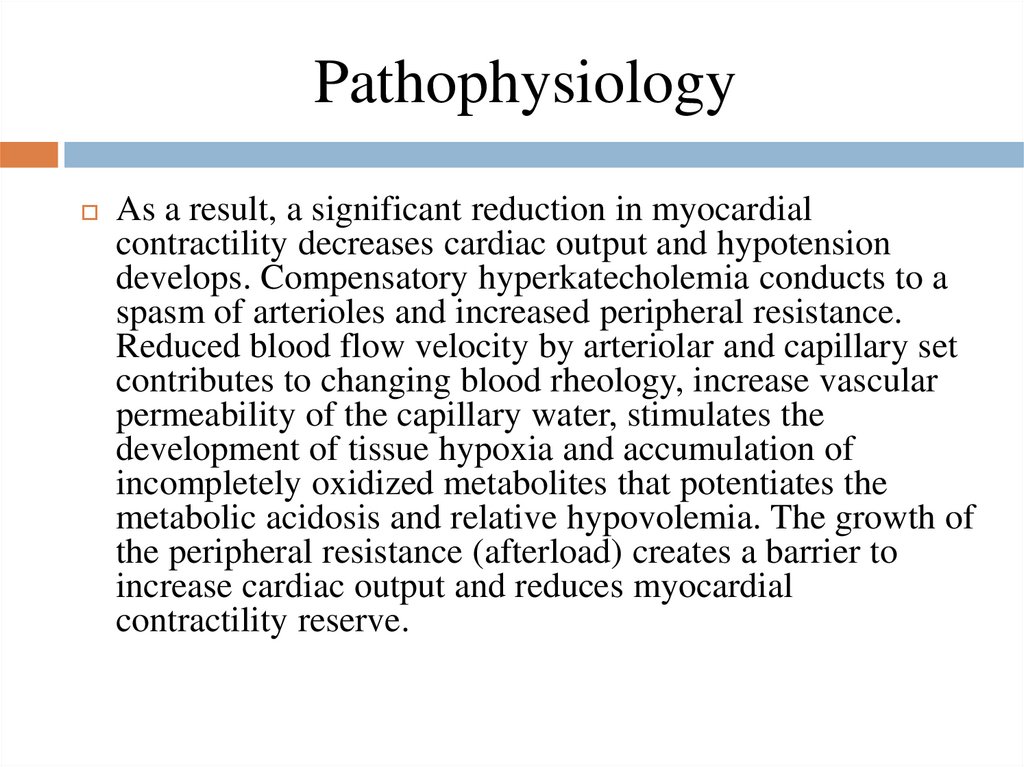
As a result, a significant reduction in myocardialcontractility decreases cardiac output and hypotension
develops. Compensatory hyperkatecholemia conducts to a
spasm of arterioles and increased peripheral resistance.
Reduced blood flow velocity by arteriolar and capillary set
contributes to changing blood rheology, increase vascular
permeability of the capillary water, stimulates the
development of tissue hypoxia and accumulation of
incompletely oxidized metabolites that potentiates the
metabolic acidosis and relative hypovolemia. The growth of
the peripheral resistance (afterload) creates a barrier to
increase cardiac output and reduces myocardial
contractility reserve.
9.
10.
11.
The syndrome of small output and hypovolemiasupports sustainable vasospasm. In turn acidotic
disclosure precapillary sphincters promotes
transition and deposition of blood in them,
exacerbating its thickening (increased hematocrit)
due to the transition of water from the vascular to
the interstitial space.
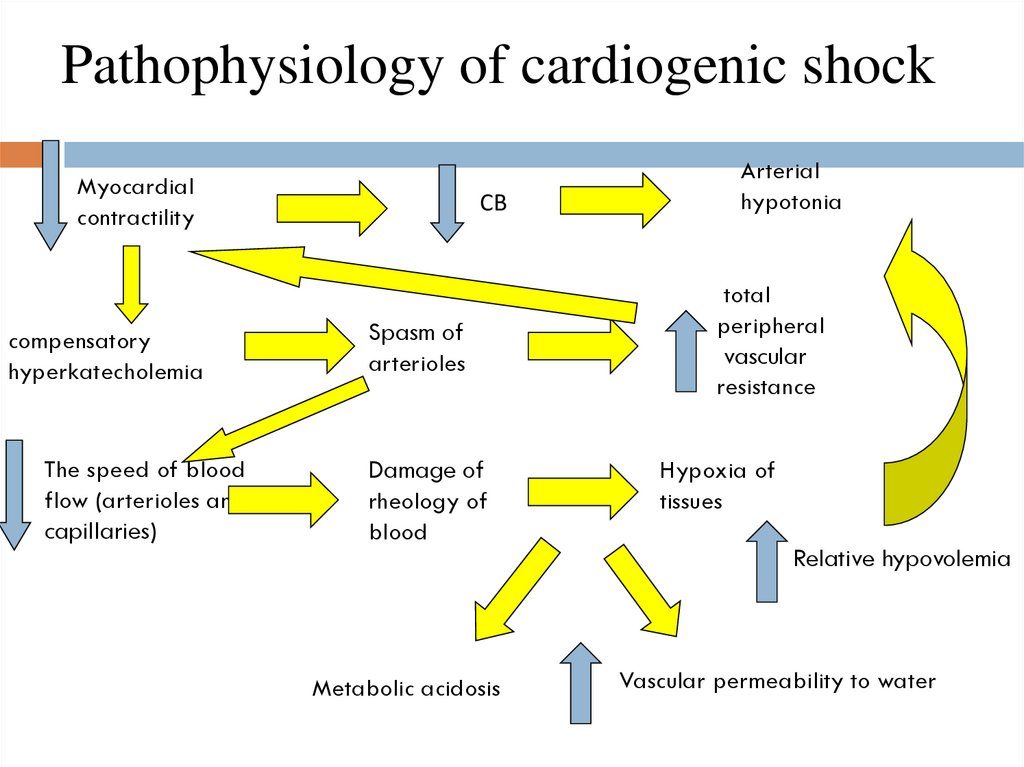
12. Pathophysiology of cardiogenic shock
Myocardialcontractility
compensatory
hyperkatecholemia
The speed of blood
flow (arterioles and
capillaries)
СВ
Spasm of
arterioles
Damage of
rheology of
blood
Metabolic acidosis
Arterial
hypotonia
total
peripheral
vascular
resistance
Hypoxia of
tissues
Relative hypovolemia
Vascular permeability to water
13. Forms of cardiogenic shock
When the type of hypovolemic circulatory amarked muscular and mental weakness, cyanosis.
Jugular vein slept. Moderate tachycardia, blood
pressure is reduced
Stagnant circulation type
-is characterized by marked cyanosis, orthopnea,
dyspnea. Jugular veins swollen. Blood pressure
varies. Allocate the following forms of cardiogenic
shock: reflex, arrhythmogenic, and true refractory or
unresponsiveness.
14.
Reflex form of shockcaused mainly not severe myocardial damage, and
the lack of a compensatory increase in systemic
vascular resistance, which in this case is reduced and
accompanied by sinus bradycardia.
Eliminating the reflex forms of shock pain relief is
achieved by introducing agonists, fibrinolytics and
heparin. After stabilization of hemodynamic
parameters of relapse of severe hypotension is not
usually the case
15.
Arrhythmogenic formoften caused by ventricular tachycardia or complete atrioventricular blockade. In the presence of a complete transverse
heart block, or bradi- tachycardia should define the indications
for pacing or defibrillation urgent implementation. In relieving
heart rhythm disorders of left ventricular pump function is
reduced and shock phenomena cropped.
The reason for the true development of cardiogenic shock is
a sharp decline in the pumping function of the left ventricle,
which arose as a complication of myocardial infarction, the
anterior wall of the left ventricle, or a massive heart attack
posteroinferior wall. The mass of necrotic myocardium of
the left ventricle is usually 40-50%.
16. Stages
I.II.
III.
By severity Vinogradov, VG Popov offered
are 3 degrees of Cardiogenic shock:
a relatively an easy (I degree)
moderate (II degree)
very heavy (III degree).
17. I stage
Duration Cardiogenic shock I leveldoes not usually exceed 3-5 hours blood pressure varies
between 85 / 50-60 / 40 mm Hg. Most of the patients
have sustained rapid pressor response (30-60 minutes
after a range of therapeutic interventions). In some
cases, especially in the elderly, a positive pressor
response may be slightly delayed, sometimes followed
by brief decrease in blood pressure and peripheral signs
of resumption of Cardiogenic shock
18. II stage
Duration Cardiogenic shock II degreefrom 5 to 10 hours blood pressure - in the range of 80 /
50-40 / 20 mm Hg peripheral signs of shock expressed
considerably and are often combined with symptoms of
acute left ventricular failure (shortness of breath at rest,
acrocyanosis, stagnant wheezing in the lungs , 20% of
patients - alveolar pulmonary edema). Pressor response to
complex therapy slowed and unstable during the first day
of the disease is noted repeatedly lowering blood pressure
with the resumption of peripheral signs of shock.
19. III stage
Cardiogenic shock III degreediffers extremely severe and prolonged course with a
sharp drop in blood pressure (up to 60/50 mm Hg and
below) and pulse pressure (less than 15 mm Hg), the
progression of disorders of peripheral circulation and the
growth effects of acute heart failure. In 70% of patients
experiencing a rapid development of the alveolar
pulmonary edema. Application adrenomimetics means
prevents positive effect pressor response is absent in most
cases. The duration of such unresponsiveness shock
ranges of 24-72 hours, sometimes it gets over undulating
and protracted nature and usually ends in death.
20.
21. Conclusion
Cardiogenic shock is uncommon, but when itdoes occur, it’s a serious medical emergency.
According to the National Institutes of Health,
almost no one survived cardiogenic shock in the
past. Today, more than 50 percent of people who
experience cardiogenic shock survive. This is due
to improved treatments and quicker recognition
of symptoms.
22. References
↑ Munkholm H, Hansen HHT, Rasmussen K. Coenzyme Q10treatment in serious heart failure. Ann Intern Med
1999;9:285-9.
↑ Sander S, Coleman CI, Patel AA, Kluger J, White CM. The
impact of coenzyme Q10 on systolic function in patients with
chronic heart failure. J Card Fail 2006;12:464-72.
↑ Soja AM, Mortensen SA. Treatment of congestive heart
failure with coenzyme Q 10 illuminated by meta-analyses
of clinical trials. Mol Aspects Med 1997;18:s159-68
Google.com
WWW.WIKIPEDIA.COM
 medicine
medicine