Similar presentations:
Tick borne enciphitalis
1.
TICK BORNE ENCIPHITALISMEDICAL ACADEMY NAMED BY SI
GEORGIEVISKIY CFU NAMED BY
V.I.VERANDSKIY
DEPARTMENT OF MEDICAL BIOLOGY
Riya lomas la1
1st course
Group 192 b
Submitted to mam Svetlana smirnova bright
2.
General characteristicsThe disease typically follows a biphasic pattern in 72–87% of patients
and the median incubation period is 8 days (range, 4–28 days) after tick
bite. Non-speci c symptoms of mild fever, malaise, headache, nausea,
vomiting and myalgias may be present as rst manifestation of the
disease and spontaneously resolve within 1 week. After another week the
patient may develop neurological symptoms.[4] The virus can result in
long neurological symptoms, infecting the brain (encephalitis),
the meninges (meningitis) or both (meningoencephalitis).[5] In general,
mortality is 1% to 2%, with deaths occurring 5 to 7 days after the onset of
neurologic signs.
In dogs, the disease also manifests as a neurological disorder with signs
varying from tremors to seizures and death.[3]
In ruminants, neurological disease is also present, and animals may
refuse to eat, appear lethargic, and also develop respiratory signs.
3.
CausesTBE is caused by tick-borne encephalitis virus, a member of the
genus Flavivirus in the family Flaviviridae. It was first isolated in 1937. Three
virus sub-types also exist: European or Western tick-borne encephalitis virus
(transmitted by Ixodes ricinus), Siberian tick-borne encephalitis virus
(transmitted by I. persulcatus), and Far-Eastern tick-borne encephalitis virus,
formerly known as Russian spring summer encephalitis virus (transmitted
by I. persulcatus).[6][7]
Russia and Europe report about 5,000–7,000 human cases annually.[1][8]
The former Soviet Union conducted research on tick-borne diseases,
including the TBE viruses
4.
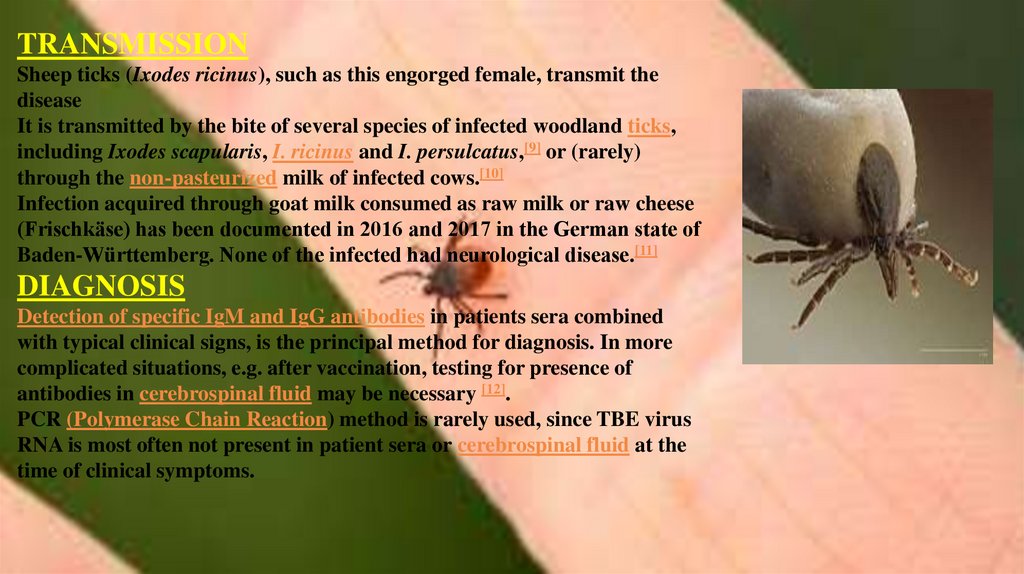
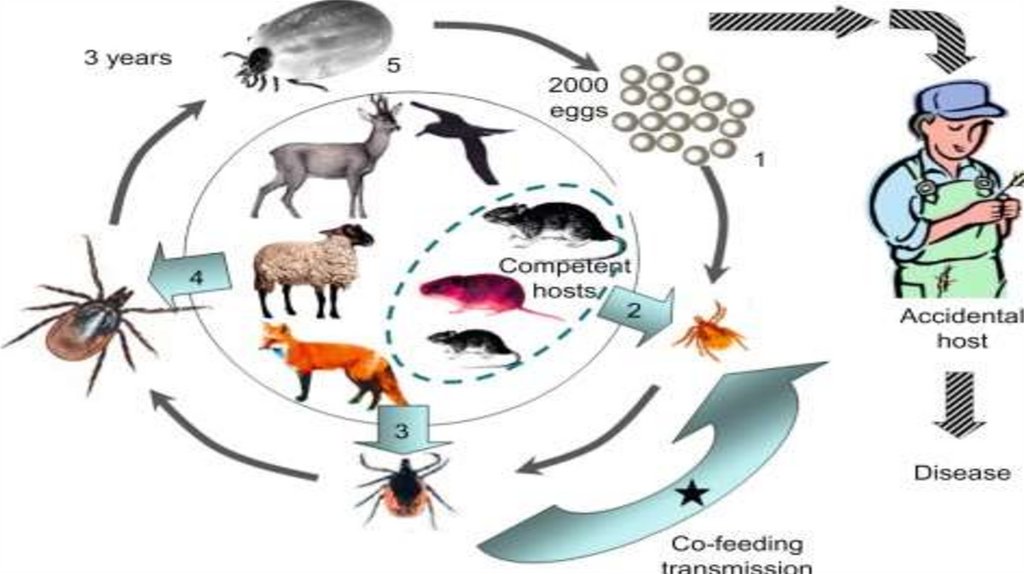
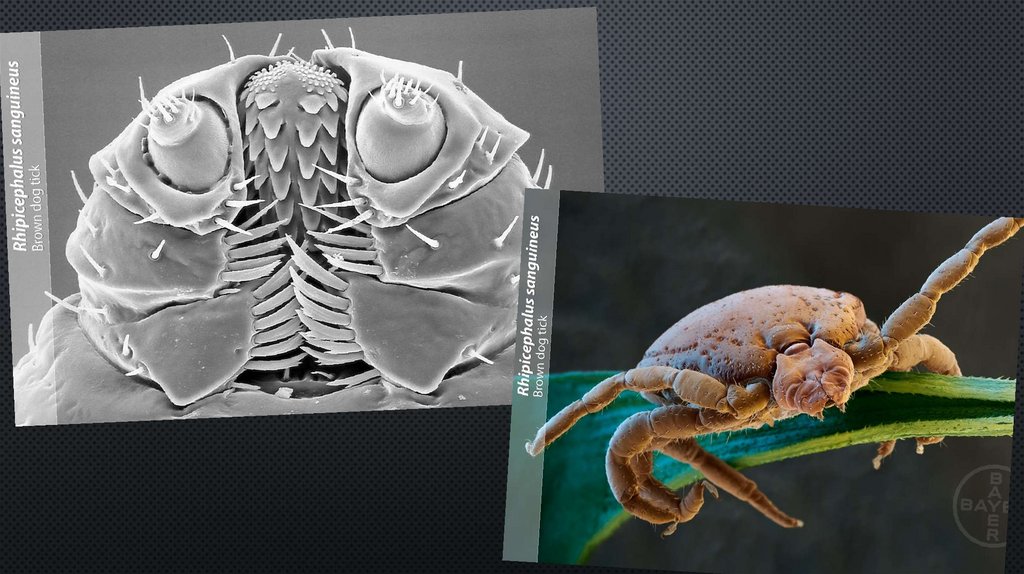
TRANSMISSIONSheep ticks (Ixodes ricinus), such as this engorged female, transmit the
disease
It is transmitted by the bite of several species of infected woodland ticks,
including Ixodes scapularis, I. ricinus and I. persulcatus,[9] or (rarely)
through the non-pasteurized milk of infected cows.[10]
Infection acquired through goat milk consumed as raw milk or raw cheese
(Frischkäse) has been documented in 2016 and 2017 in the German state of
Baden-Württemberg. None of the infected had neurological disease.[11]
DIAGNOSIS
Detection of specific IgM and IgG antibodies in patients sera combined
with typical clinical signs, is the principal method for diagnosis. In more
complicated situations, e.g. after vaccination, testing for presence of
antibodies in cerebrospinal fluid may be necessary [12].
PCR (Polymerase Chain Reaction) method is rarely used, since TBE virus
RNA is most often not present in patient sera or cerebrospinal fluid at the
time of clinical symptoms.
5.
6.
Transmission7.
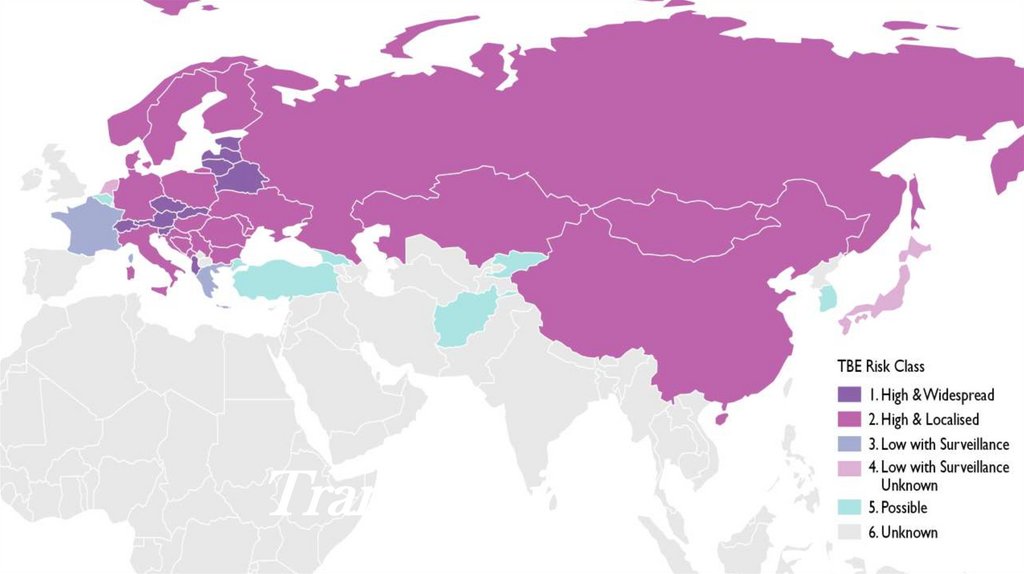
EpidemiologyAs of 2011, the disease was most common in Central and Eastern Europe, and Northern Asia. About ten to twelve
thousand cases are documented a year but the rates vary widely from one region to another.[16] Most of the variation
has been the result of variation in host population, particularly that of deer. In Austria, an extensive free vaccination
program since the 1960s reduced the incidence in 2013 by roughly 85%.[17]
In Germany, during the 2010s, there have been a minimum of 95 (2012) and a maximum of 584 cases (2018) of TBE
(or FSME as it is known in German). More than half of the reported cases from 2019 had meningitis, encephalitis or
myelitis. The risk of infection was noted to be increasing with age, especially in people older than 40 years and it was
greater in men than women. Most cases were acquired in Bavaria (46 %) and Baden-Württemberg (37%), much less in
Saxonia, Hesse, Niedersachsen and other states. Altogether 164 Landkreise are designated FSME-risk areas, including
all of Baden-Württemberg except for the city of Heilbronn.[11]
In Sweden, most cases of TBE occur in a band running from Stockholm to the west, especially around lakes and the
nearby region of the Baltic sea.[18][19] It reflects the greater population involved in outdoor activities in these areas.
Overall, for Europe, the estimated risk is roughly 1 case per 10,000 human-months of woodland activity. Although in
some regions of Russia and Slovenia, the prevalence of cases can be as high as 70 cases per 100,000 people per
year. [17][20] Travelers to endemic regions do not often become cases, with only 5 cases reported among U.S. travelers
returning from Eurasia between 2000 and 2011, a rate so low that as of 2016 the U.S. Centers for Disease Control and
Prevention recommended vaccination only for those who will be extensively exposed in high risk areas.[21]
8.
TreatmentThe disease is incurable once manifested, so there is no specific drug therapy for TBE. Symptomatic brain
damage requires hospitalization and supportive care based on syndrome severity. Anti-inflammatory drugs,
such as corticosteroids, may be considered under specific circumstances for symptomatic relief. Tracheal
intubation and respiratory support may be necessary.
Since there is no chemotherapy or specific treatment available targeting the TBE virus itself,
symptomatic or supportive treatment (e.g. maintenance of the water and electrolyte balances) is
required. This lack of targeting treatment emphasizes the necessity of tick prophylaxis. Repellent
parasiticides may be the right choice to minimize attachment and subsequent feeding of the tick
vector.
In the case of diseased dogs emphasis has to be put on preventing secondary harm to the patient
itself as well as the owner during convulsions and aggressive behavior. For that reason, therapy
should include resting as well as anticonvulsive and sedative medication (Pfeffer and Dobler, 2011).
Non-steroidal anti-inflammatory drugs (NSAID) are best used to combat the high fever, and
antibiotics should be given to prevent secondary bacterial infections, in particular pneumonia (Kritz
et al., 2001). Most of the few dogs, that survived a clinical TBE needed between a hal
9.
10.
Clinical SignsCanine TBE
The incubation period for canine TBE in most cases is between 7 and 14 days. Clinical canine TBE is a
febrile illness with multifunctional neurological manifestations such as ataxia, uncoordinated movements,
abnormal reflexes, convulsions, tremor, paresis, paralysis, and cranial nerve deficits such as facial
paresis. The neurobiological signs are often progressive and TBE may lead to death.
In general the risk for a tick-infected dog to develop clinical manifest TBE is very small. A serological
survey performed in dogs from Sweden in 1992 proved 18 of 225 dogs (8%) to be seropositive and 16 of
these 18 dogs showing neurological signs (Bjöersdorff, 2002).
Human TBE
The incubation period is between 3 and 28 days. The course of disease is often asymptomatic. An
estimated 30% will exhibit clinical disease, mainly as a feverish flu-like disease. 10-15% of cases
(increasing rate with age) will have neurological disorders with the most severe form of persisting paresis
and psychiatric sequelae.
In central Europe, the typical case of encephalitis has a biphasic course, with an early, viremic, flu-like
stage, followed about a week later by the appearance of signs of meningoencephalitis. CNS disease is
relatively mild, but occasional severe motor dysfunction and permanent disability occur. The case fatality
rate is 1% to 5%.
Russian spring-summer encephalitis (sometimes referred to as the "Far Eastern form") normally does not
show a biphasic course but is characterized by massive headache, high fever, nausea, and vomiting.
Delirium, coma, paralysis, and death may follow; the mortality rate is approximately 25% to 30%.
Louping ill infection is generally mild and also displays a biphasic pattern. The virus infects sheep; few
cases are reported in humans.
11.
Human Tick ParalysisIn humans, tick paralysis is most likely to be seen in children. The symptoms in humans
are similar to the clinical signs in dogs. About two thirds of human cases are seen in
young females. The tick bites are most often found at the head and there at the transition
of hair and neck. The clinical presentation appears as typical ascending flaccid paralysis.
After aprodromal phase (paraesthesias, restlessness, irritaility, fatigue, and myalgias)
neurological symptoms will start with paralysis of the lower extremities. The deep tendon
reflexes are weak or absent. Duirng the next 12 to 24 hours the muscles innervated by
facial nerves become weak. Without removal of the tick, finally the respiratory muscles will
fail and the patient will die of respiratory failure. Rare forms of illness include focal
muscles paralysis (facial muscles, arm muscles, pupillary dilation, and acute cerebellar
syndrome). Sensory findings are generally absent and therefore form an important
differential diagnostic symptom to the Guillain-Barré syndrome where sensory findings are
frquently found during the prodromal stage of disease.
12.
How many tick borne diseases are there?A recent CDC report showed that vector-borne diseases - those transmitted by ticks, mosquitoes, and fleas -tripled to roughly 650,000 cases between 2004 and
2016. The vast majority -- or 75% -- were caused by
ticks. The report says seven new tickcaused illnesses were discovered between 2004 and 2016.
13.
Encephalitis is an inflammation ofthe brain, usually caused by a
viral infection. Although rare, it is
potentially life-threatening, and
may lead to permanent brain
damage or death.
14.
Some forms of encephalitis are more severethan others. For example, herpes simplex
encephalitis (HSE) has a mortality rate of
up to 30% even with specific anti-viral
treatment, and 70-80% without the
treatment. When death happens it is usually
because of the brain swelling as a result of
its severe inflammation.
15.
Lyme encephalopathy is a rareneuropsychiatric disorder,
predominantly affecting memory and
concentration [3–7]. Other associated
symptoms and signs may include
headache, mild depression, irritability,
fatigue, or excessive daytime sleepiness
16.
The prognosis for a personwith encephalitis varies according to the
age of the patient – with the very young
and very old particularly at risk – and
the particular virus that caused the
disease. While many people make a full
recovery, in severe cases, the illness may
be fatal or result in brain damage.
17.
The contagious period and incubationperiod for encephalitis depends on the
underlying cause of encephalitis. For
example, some herpesviruses have
an incubation period of about three to seven
days on average but may range from about
one to three weeks.
18.
https://youtu.be/Bv3hQZVtE6Yhttps://youtu.be/ENmVXtwsKE8
19.
• FURTHER INFORMATION• EDLOW JA, MCGILLICUDDY DC: TICK PARALYSIS. INF DIS CLIN NORTH AM. 2008, 22,
397-414
• GORDON BM, GIZA CC: TICK PARALYSIS PRESENTING IN AN URBAN ENVIRONMENT.
PEDIATR NEUROL. 2004, 30, 122-4
• MALIK R, FARROW BR: TICK PARALYSIS IN NORTH AMERICA AND AUSTRALIA. VET CLIN
NORTH AM SMALL ANIM PRACT. 1991, 21, 157-71
• WRIGHT IG, STONE BF, NEISH AL: TICK (IXODES HOLOCYCLUS) PARALYSIS IN THE DOG –
INDUCTION OF IMMUNITY BY INJECTION OF TOXIN. AUST VET J. 1983, 60, 69-70















 biology
biology