Similar presentations:
Shock. Etiology, pathogenesis, intensive therapy
1. Shock. Etiology, pathogenesis, intensive therapy.
2.
Terminology: The word shock ( "choc " inFrench and "shock " in English) is translated as
stroke, shock. This term was used in the Middle
Ages called the state of the armor-clad knights
who fell into a stupor after impact of lance or
spear. For the first time, both the medical term
used a French military surgeon Le Dran in 1741.
Widely implemented in practice by James Latta
in 1743.
3.
Shock - critical condition which develops as aresult of impact on the body a factor (internal or
external), the force and/or the duration of which
exceeds the compensatory capacity of the
organism.
A physiologic state characterized by
Inadequate tissue perfusion
Clinically manifested by
Hemodynamic disturbances
Organ dysfunction
4.
Shock is not a disease entities, itdecompensation syndrome, which is
accompanied by a variety of pathological
conditions.
The diagnosis is a shock - about the danger
signal and the need for intensive care methods!
Basically, the shock is considered as
hemodynamic syndrome, i.e. reduction in the
systemic circulation, microcirculation
disturbances and tissue perfusion with
subsequent hypoxia and necrosis of cells
5.
6.
7.
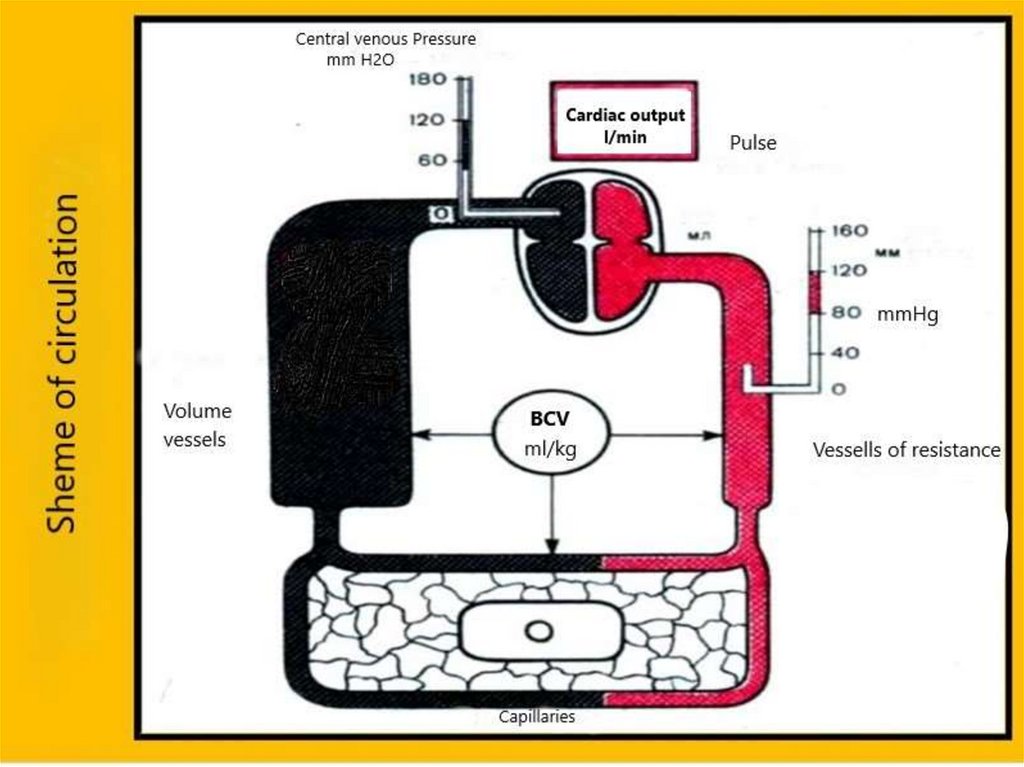
Physiological constantsBlood volume (CBV) - 70 ml / kg (males 70-75, 65-70
women).
Distribution of blood in the body:
Heart - 7%
Pulmonary circulation - 9%
The arteries of the systemic circulation - 15%
Capillaries of a large range of - 5%
Veins of large circle - 64%
Central venous pressure (CVP) - 60-120 mm H2O It
reflects the blood return to the right ventricle.
8.
ClassificationAccording to the basic link of pathogenesis are
4 kinds of shock:
hypovolemic
cardiogenic
obstructive
distributive (vasogenic)
9.
1.Hypovolemic- it is based on reduction of CBV. Theseinclude: hemorrhagic, traumatic shock, burn shock,
dehydration shock
2. Cardiogenic - due to the failure of myocardial
contractile function
3.Obstruсtive- due to cardiac dysfunction from
extracardiac reasons (pulmonary embolism, cardiac
tamponade, tension pneumothorax) - caused by
vascular insufficiency.
4.Distributive (Vasogenic) - anaphylactic, endocrine
(adrenal insufficiency), neurogenic (spinal), septic.
10.
11.
12.
Keep in mind that, regardless of theprimary cause, in the final phases of the
shock pathophysiological mechanisms are
the same.
13.
Hypovolemic shock14.
Hypovolemic shockPathophysiology
Acute loss of more than 20% of the intravascular fluid due to blood
loss or dehydration.
One possible mechanism of development - occlusion of the vein,
thrombosis and embolism main veins, compression of the inferior
vena cava
Etiology
External bleeding
Plasma loss from burn surface
Multiple injuries
Gastrointestinal bleeding
Diabetic ketoacidosis
Pancreatitis
Heavy, frequent vomiting
Profuse diarrhea
15.
Blood lossFracture of pelvis in conjunction with damage to
internal organs - 3-3.5 liters (60-70% BCV).
Fracture of the femur - 0.5-1 l.
Fracture of the tibia - 0,3-0,75 l.
Traumatic separation of the tibia - 1.8 liters.
Fracture of the humerus - 0.3-0.5 liters.
Traumatic amputation of shoulder - 1.5 liters.
Fracture of forearm bones - 0.25-0.4 l.
Traumatic amputation arm-1,0 l.
16.
The clinical phase of development of ashock
erectile phase
excitation
heart rate acceleration
a transient increase of blood
pressure
microcirculation disturbance
dyspnea
torpid phase
inhibition of central nervous system
(Affected becomes adynamic, drowsy)
blood pressure drop
reduction of BCV,
pulse weak and thready
depressed reflexes.
terminal phase
Disruption of the body's compensatory capacities
The drop in blood pressure below a critical level
Pulsation peripheral vascular not determined
Skin become of marble color
17.
The pathogenesis of traumatic shockpain
decrease in BCV and myocardial contractility
microcirculation disorders, blood cell aggregation occurs, which clog the
capillary network;
disorders of pulmonary gas exchange, hypoxia, pulmonary shunts, the
deterioration of the function of the alveolar-capillary membrane formed
shock lung syndrome;
disorders tissue gas exchange due to reduction of blood flow volume of
tissue
changes in metabolism towards anaerobic path to form an excess of
lactate and other organic acids; acidosis, which results in deepening and
paresis vascular circulatory decompensation-vicious circle
development of "shock kidney" (pre-renal and renal oliguria) as a
consequence of renal hypoperfusion;
dysfunction of other organs (brain, liver, adrenal glands, intestine)
generalization of infection, and especially the intestinal flora;
the development of DIC;
breakdown of water-salt metabolism and protein balance.
long vasospasm also leads to the development of ulcers
stomach, hemorrhagic enteritis
18.
Vasoconstriction occurs within 30-60 seconds after theinjury.
Primarily reduced capacitance vessels (veins) and the
resistance vessels (arterioles).
Venous return to the right heart increases due to
contraction of the veins and narrowing of arterioles
causes blood flow redistribution. Blood passes
capillaries through arteriovenous anastomoses and
immediately returned to the vein.
Thus, the volume of the blood goes to the vital organs
(brain and heart) - developed circulatory centralization
19.
Next compensation mechanism that developswithin the first hour - interstitial fluid enters to
the bloodstream. This increases the BCV, at the
same time decreases the amount of interstitial
fluid.
Temp fluid intake can be up to 1 l / hr. Further
activation of the sympathoadrenal system
causes releasing of other hormones. Primarily
the level of vasopressin (ADH) increases and
RAAS activation starts.
20.
Total effects ADH and RAAS leads to adecrease in diuresis. Retention of water and
salts increases BCV and volume of interstitial
space, enhance circulatory centralization.
The next stage - the synthesis of red blood
cells by the bone marrow begins within a few
hours, but it takes a long time (up to 2 months)
21.
Hemodynamics and survey data fizikalgolow CVP
Low cardiac output
High peripheral vascular resistance
Jugular veins distansion
Cold sweat
Slow capillary refill of the nail
22.
Shock index Algovepathe ratio of heart rate to blood pressure.
In a normal heart rate for 60 minutes, systolic
AD 120 mm Hg. Art. index is0.5 - 0.54.
Shock degree I - index of from 0.8 to 0.9;
Shock II degree - 0.9 - 1.2;
Shock III degree - 1.3 or higher.
The symptom of "white spot".
When you press on the nail of the thumb, it becomes
pale and restored its original color longer than 2
seconds - a symptom is considered positive.
23.
24.
"Small" signs of shockpale skin
conjunctival pallor
cold sticky sweat
mouth dryness
thirst
a symptom of "white spots" - more than 2
seconds.
decreased urine output-less than 30 ml / h
25.
Reduction of hemoglobin, hematocrit,red blood cells in peripheral blood
does not develop immediately (the
need for dilution of extracellular fluid),
so that a proper evaluation requires
dynamic control of these parameters
26.
Stages of shockI st- compensated - loss of 20% of BCV systolic BP 90-100 mmHg, pulse rate 100 / min,
Shock index of about 1.
RR = 20-22 / min. Consciousness is clear,
oliguria is absent
II st subcompensated - loss of 25-30% of BCV systolic BP 70-90 mmHg, pulse rate 120 / min.
shock index of about 1.5, RR up to 30/min, CVP
decreased, consciousness is not broken,
oliguria
27.
III st- decompensated reversible - loss of 30-40% ofBCV - systolic BP 50-70 mmHg, pulse rate 120/min,
shock index of 2 or more, RR over 30 / min, CVP
negative, consciousness broken (stunning), significant
oliguria or anuria.
IV st- refractory irreversible (terminal) - BCV loss of
more than 40% -50% - BP lower than 50 mmHg, item or
not is determined, the pulse on peripheral arteries
"filiform" or not is determined, a heart rate more
140/min. Growing bradycardia is a sign of a quick stop
of the heart, RR more than 40/min, profound
disturbance of consciousness, anuria.
28.
Treatment ofhemorrhagic and
traumatic shock
29.
The main anti-shock activityHemostasis
Providing free airway patency
Anesthesia (drugs)
Installation of central venous access (subclavian vein catheterization)
infusion solutions (saline, colloid) and blood products (in the absence of signs
of pulmonary edema)
vasopressors (dopamine to 10 mkg / kg / min, or epinephrine, or
norepinephrine 0.01-0.1 mkg / kg / min).
30.
Prehospital aidPartially revised the tactics of
infusion-transfusion therapy in the
prehospital phase. If bleeding is not
stopped, massive fluid therapy
increases BP, it’і can lead to revival
bleeding and prognosis.
31.
Adequate consciousness, sufficient diuresis (30ml / hr), the absence of a severe tachycardia
and hyperventilation, stable BP (systolic of at
least 80 mm Hg) - signs of adequate gas
exchange, when the patient should be left alone
in the literal and figurative sense. Working
muscles require 20 times more blood than the
muscle at rest.
32.
When a shock is suspected:identify the specific cause and severity of
the condition
carry out the necessary treatment with
the appropriate specialist
Urgent surgical intervention, including
hemostasis, drainage of tension
pneumothorax, cardiac tamponade
liquidation carried out immediately
simultaneously with intensive care
33.
General principles of treatmentThe basis of any treatment of hypovolemic
shock is fluid resuscitation, i.e filling the BCV,
which has the advantage over the administration
of vasopressors.
When treating patients with any shocks is
necessary to observe the principle of "three
catheters" - a catheter into a vein, the
introduction of nasogastric tube, a catheter into
the bladder. It is also advantageous to use
oxygen nasal catheter or mask
34.
Following questions need to be decidedbefore planning treatment
where
what
how much and in what order of
entering into the bloodstream
35.
Crystalloid infusion solutions or colloidsand crystalloids simultaneously insert at
the beginning. If rapid infusion in a
volume of 800-1200 ml does not increase
the BP, it is advisable to start introduction
of sympathomimetics: dopamine in
moderate doses, norepinephrine,
mezaton.
36.
Blood transfusion, especially red bloodcell mass is advisable to begin only after
the full recovery of BCV and
microcirculation, otherwise it simply will
not be able to perform its function.
Blood transfusion may be replaced or
supplemented perfluorane infusions.
37.
Classification of plasma substitutes38.
Crystalloid solutions:drugs with low molecular weight
quickly leave the bloodstream and move into the
interstitial space.
in the bloodstream leaves 1/3 - 1/4 of the
administered volume.
duration of circulation in the bloodstream is
about 30 minutes
Examples: isotonic sodium chloride solution,
Ringer’s sol, Ringer-lactate sol, Trisol,
Reosorbilact etc.
39.
2. The colloid plasma expandersThis solution of high molecular weight, which for a
long time (4-6 hours) are contained in the lumen
of the vessel and thereby maintain the BCV
Examples:
a. dextran derivatives - Poliglyukin, Reopoligljukin
b. gelatin derivatives - Zhelatinol
c. hydroxyethyl starch derivatives - Refortan, Stabizol, Gekodez,
Refordez, Voluven®
d. plasma expanders with the function of oxygen transport Perftoran.
e. natural colloids - fresh frozen plasma, packed red blood cells,
albumin
40.
Hydroxyethyl starch derivatives:low MW (130,000) It belongs to the
pharmacological group "Tetrastarch "Voluven®, Volyutenz
Average MW (200000) - to the group
"Pentastarch “-Stabizol, Plazmasteril
High MW (450,000) - to the group "Hetastarch "
- Refortan, Gekodez
Hetakrahmal compared with tetra and pentastarch causes a longer
plasma-effect, but can sometimes have a negative impact on blood
clotting
41.
Algorithms infusion-transfusion therapy fordifferent amounts of blood loss
1.Blood loss up to 10% VBC does not require
replacement.
2. Loss 10-15% volume - crystalloid infusion
solutions. The volume of crystalloid infusion
should exceed 3 times the volume of blood loss
(300% of the amount of blood loss).
3. Blood loss 15-20% VBC compensates by
combination of synthetic colloids and
crystalloids in a ratio of 1: 2.Volume infusion 200% VBC loss.
42.
4.Defitsit VBC 20-30% - synthetic colloids,crystalloids plasma expanders. The ratio of
colloids - crystalloids 1: 1. Infusion Volume 180-200% of deficit. According to current
guidelines, blood loss up to 30% of VBC does
not require blood transfusion therapy.
5. Deficit 30-40%BCC - the volume of the
infusion 200-250% of deficit. Included
crystalloids, synthetic colloids, fresh frozen
plasma, packed red blood cells. The ratio is 1:
1: 1: 1
43.
In the treatment of traumatic shock should notforget the need for adequate immobilization and
full anesthesia. Anesthesia implements by
narcotic, non-narcotic analgesics, ketamine and
different types of local anesthesia.
The introduction of narcotic analgesics is
contraindicated in patients with head injury
and with suspected injury to the abdominal
organs.
44.
Clinic of shock depends on the reasons thatcause shock and localization of the injury.
Traumatic brain injury is often masks the shock
clinic due to symptomatic hypertension. On the
other hand significant hemodynamic disorders
can lead to disturbance of consciousness.
Empirically, it is believed that when the systolic
BP less than 70 mm, and the patient has
consciousness, it does not have a serious head
injury.
45.
Criteria of efficiency antishock therapy1. In patients without cardiac disease:
Mean blood pressure> 60 mm Hg;
CVP> 2 cm H2O;
Diuresis> 50 ml / h
2. In case of doubt:
Sample load volume with: for 15-20 min poured 400-500 ml
crystalloid and observing the dynamics of CVP and diuresis
-Significant increased CVP without increasing urine output suspected heart failure.
- CVP and diuresis remain low - most likely hypovolemia,
requires a higher rate of re-infusion phase estimate.
- An increase of urine output - prerenal oliguria, renal
hypoperfusion due to hypovolemia.
3. When a circulatory system is compromised :
Inotropic support (increased cardiac output)
Correct using of diuretics,
Manipulating of afterload
46.
Cardiogenic shockPathophysiology
Reducing the stroke volume of the heart with the defeat:
- violation of the contractile function
- failure or obstruction of valves,
- intracardiac reset from left to right
- arrhythmia
Etiology
Myocardial infarction,
Severe myocarditis
Acute mitral or aortic regurgitation
Significant aortic stenosis
Prosthetic valve thrombosis
Rupture of the interventricular septum
Cardiac tamponade
Myocardial insufficiency after cardiac surgery.
47.
Hemodynamics and physical examinationdata
High CVP
Low cardiac output
High peripheral vascular resistance
Jugular venous distention
Cold sweat
Slow capillary refill of the nail
Possible pulmonary edema, chest pain, and heart
murmur
48.
Obstructive shockPathophysiology
Reduction in stroke volume due to the extracardiac causes.
Etiology
PE (pulmonary embolim)
Cardiac tamponade
Tension pneumothorax
49.
Hemodynamics and physical examinationdata
High or Low CVP
Low cardiac output
High peripheral vascular resistance
Often - distention of the neck veins
Cold sweat
Slow capillary refill of the nail bed
Rarely - pulmonary edema
50.
Distributive shockPathophysiology
A significant reduction in peripheral vascular resistance with
redistribution intravascular volume due to the increase
capillary permeability or arterio-venous shunting
Etiology
acute adrenal insufficiency
anaphylaxis
sepsis
neurogenic shock
toxic shock
51.
Hemodynamics and physical examinationdata
Low CVP
Increased cardiac output
Low resistance peripheral
vessels
Lack of the neck veins
distention
limbs warm
capillary of nail refill
normally
52.
Symptoms of shockDecreased blood pressure;
Increased heart rate >90 beats per minute, the pulse becomes weak,
"filamentous";
Increased frequency of respiratory movements;
Severe weakness: a man unable to move, and sometimes - even to say the
words;
Skin pallor:
The absence of urine (anuria)
Varying degrees of impairment of consciousness up to the loss; lack of
response to pain.
Shock does not always lead to a quick death, he often develops gradually –
during minutes, tens of minutes or even several hours. In this listed
symptoms and progress in the above order.
53.
The adult patients compensate state of shockprincipally by decrease systemic vascular
resistance, increase cardiac contractility and
increased heart rate.
The child's body compensates for this condition
primarily an increase in heart rate and
vasoconstriction. Vasoconstriction in children
leads to the fact that hypotension becomes late
sign of shock.
54.
Anaphylactic shock or anaphylaxis- acute
generalized allergic reaction of immediate type, the state
dramatically increased sensitivity of the organism that
develops due to repeated insertion of the allergen into the
body, accompanied by damage to its own tissues, lower blood
pressure and vital organs circulatory disturbance.
55.
One of the most dangerous complications ofdrug allergy, ends in 10-20% of cases,
lethal.
The appearance time of anaphylactic
shock - from a few seconds or minutes to 2
hours from the start of contact with the
allergen. In the development of anaphylactic
reactions in patients with a high degree of sensitization
dose or route of administration of the allergen does not
play a decisive role. However, a large dose increases
the severity and duration of shock.
56.
Pathogenesis57.
EtiologyMedication.
The introduction of blood products.
Food products (eggs, coffee, cocoa, chocolate,
strawberry, fish, milk, alcoholic drinks).
The introduction of vaccines and serums.
Insect bites (wasps, bees etc.).
Pollen allergens.
Chemical agents (cosmetics, detergents).
Animal dander.
58.
Clinical symptoms1. Initial period develops within 3-30 minutes after
allergen exposure (medication, food, insect sting or bite,
etc.).
Local reactions at the site of contact with the allergen into
the body - an unusually sharp pain, swelling and
hyperemia at the place of the sting or injection of the drug,
a strong itching of the skin, quickly spreads all over the
skin (generalized pruritus). After receiving the allergen per
os the first symptom may be a sharp pain in the abdomen,
nausea and vomiting, swelling of the mouth and larynx.
59.
Clinical symptoms2. The period of clinical manifestation
characterized by loss of consciousness,
decrease of blood pressure (less than 90/60 mm
Hg), tachycardia, paleness of the skin, lips
cyanosis,
cold
perspiration,
dyspnea,
involuntary urination and defecation, decreased
urine output.
60.
clinical symptoms3. Output period of shock usually lasts 3-4 weeks.
Patients have weakness, headache, memory
impairment. During this period may develop acute
myocardial infarction, cerebrovascular disease,
allergic myocarditis, glomerulonephritis, hepatitis,
lesion of the nervous system (meningoencephalitis,
arachnoiditis, polyneuritis), hemolytic anemia and
thrombocytopenia.
61.
Form of anaphylactic shockat Hemodynamic form the clinic with hypotonia dominated
by pain in the heart, arrhythmias. Possibly the development
of acute myocardial infarction and acute left ventricular
failure.
Asphyxial form characterized by the appearance of
dyspnea (bronchoconstriction, pulmonary edema) or
hoarseness and stridor (laryngeal edema).
at Abdominal form patients is dominated by epigastric
pain, symptoms of irritation of the peritoneum, involuntary
defecation, melena
Cerebral form characterized by agitation, stunning,
convulsions and meningeal symptoms which are caused by
cerebral edema and meningitis.
62.
DiagnosticsDiagnosis of anaphylaxis is based on specific clinic:
hypotension,
loss of consciousness,
peripheral signs of shock,
symptoms develop after administration of drugs, food
intake, insect bites, etc.
Determination of serum tryptase (the single marker of acute
allergic reactions in the international practice) three times:
immediately, after 30-120 minutes and after 24 hours.
63.
Cross-allergic reactions are observed between:1. Natural and semi-synthetic penicillins (penicillin G, oxacillin,
ampicillin, amoxicillin, and others).
2. Streptomycin and other aminoglycosides (neomycin, kanamycin,
gentamycin, amikacin, etc.).
3. Cephalosporins and penicillin.
4. Tetracycline and its derivatives (doxycycline and others).
5. Iodine and iodinated all preparations (Lugol's solution, iodinecontaining radiopaque agents and others).
6. Thiamine and cocarboksylase.
7. Barbiturates and derivatives (pentobarbital and others).
8. Non-steroidal and certain analgesic agents (e.g., drugs between
pyrazolone (metamizole sodium), acetylsalicylic acid and between
preparations from different subgroups of non-steroids.
64.
Risk factors for the development of medicinal allergiesthWith the patient's side
age
characteristic
Young adults are more at risk of adverse drug reactions than children
and the elderly
gender
Women are more likely to develop adverse drug reactions to drugs
than men
heredity
Atopy may provoke more serious and severe reactions. Genetic
polymorphism. Concomitant HIV disease, herpes infection (PVG1,
G2, G3, EBV, CMV, and others), cystic fibrosis (through the frequent
use of antibiotics)
immune status
Previous MA or previous positive allergic skin test tolerated drug
Associated with drugs
The chemical properties of drugs
Beta-lactam components, neuromuscular blockers, radiocontrast
agents, NSAIDs are the most common. Macromolecular components
/ gaptenformuyuchi more immunogenic preparations
mode of application
Adverse drug reactions to drugs often arise when applied topically
than parenteral / peroral
dosage
Frequent or prolonged use
65.
First aid90% of allergic reactions developed within 10
minutes after drug application.
66.
Tourniquet on the limb does notoverlap!
The injection site is not pricked
around!
67.
Priority treatmentEpinephrine (adrenaline) may save the patient's life, therefore, should be
immediately administered as first-line treatment of anaphylaxis.
Early introduction of epinephrine should be conducted on an individual
basis, when the allergic reaction is likely to develop into anaphylaxis.
Epinephrine be administered intramuscularly in the outer surface of the
middle third of the femur 0.01 mg / kg, dilution 1: 1,000 (1 mg / ml) of a
maximum of 0.5 mg (adult) or 0.3 mg (child).
Patients who need repeated doses of epinephrine injection should be
administered at least every 15 minutes.
In the case of an inadequate response to two or more doses of epinephrine
intramuscularly, it is administered as an infusion (infusion) in the emergency
department (emergency), intensive therapy with cardiac monitoring.
68.
The second line of treatmentIt should suspend trigger anaphylactic reactions
Providing the correct body position for aspiration prophylaxis (supine
position with their tender limbs with unstable circulation, in the sitting
position for respiratory failure in saving the situation on the side of the
loss of consciousness.
Oxygen through a mask with 6-8 L / min
Recovery airway patency and aspiration prevention
Quickly enter 1-2 liters of 0.9% sodium chloride solution through the
catheter (5-10 ml / kg in the first 5-10 minutes adult, 10 ml / kg child)
Inhaled beta-2 agonists
If necessary - the cardio-pulmonary resuscitation
69.
In severe shock is necessary to transfer the patient onmechanical ventilation with increased concentration of
oxygen in the inspired gas (50-60%).
epinephrine intravenously at a dose of 0.3-0.5 mg, if
needed, i.e. for refractory hypotension, epinephrine
infusion can be continued or dopamine (5-10 mkg /kg/
min) in order to maintain a value of BP 60 mmHg
70.
In cases of a significant tachycardia (> 120 beats / minute)tachyarrhythmia or blood pressure may be maintained by
norepinephrine or phenylephrine
In the treatment of severe anaphylactic shock observed
significant loss of fluid due to a significant endothelial
damage, so massive infusion fluid necessary to 2-4 liters.It is
usually necessary to apply a solution of sodium chloride
0.9%.
In severe cases it is necessary to apply a solution of HES
130 000 / 0.4.
71.
According to modern views the introduction ofchloride or calcium gluconate, was widely
practiced before can cause a negative impact
on the patient's condition.
72.
H1 blockers and systemic H2 receptor can alleviate the symptoms ofcutaneous anaphylaxis (infusion - H1-receptor blockers
(chlorpheniramine 10 mg (adults) 2.5-5 mg (children) or
diphenhydramine 25-50 mg (adults) and 1 mg / kg, a maximum of
50 mg (children) H2 receptor blockers - ranitidine 50 mg (adults) or
1 mg / kg, a maximum of 50 mg (children)).
Systemic corticosteroids (glucocorticoids) can be used as they can
reduce the risk of respiratory symptoms late phase and
generalization process (infusion - Hydrocortisone 200 mg (adults), a
maximum of 100 mg (children) or methylprednisolone 50-100 mg
(adults) and 1 mg / kg up to 50 mg (children).
73.
Patients who exhibit respiratory failureshould be carefully inspected for at least 68 hours; patients who exhibit instability
circulation should be inspected for 12-24
hours in reanimation department, followed
by transfer to allergological department.
Before discharge should assess the risk of
future reactions autoinjector with
epinephrine should be assigned to persons
who are at risk of relapse.


































































 industry
industry