Similar presentations:
Cartilages. Case 8
1. Case 8
omar2. Cartilages
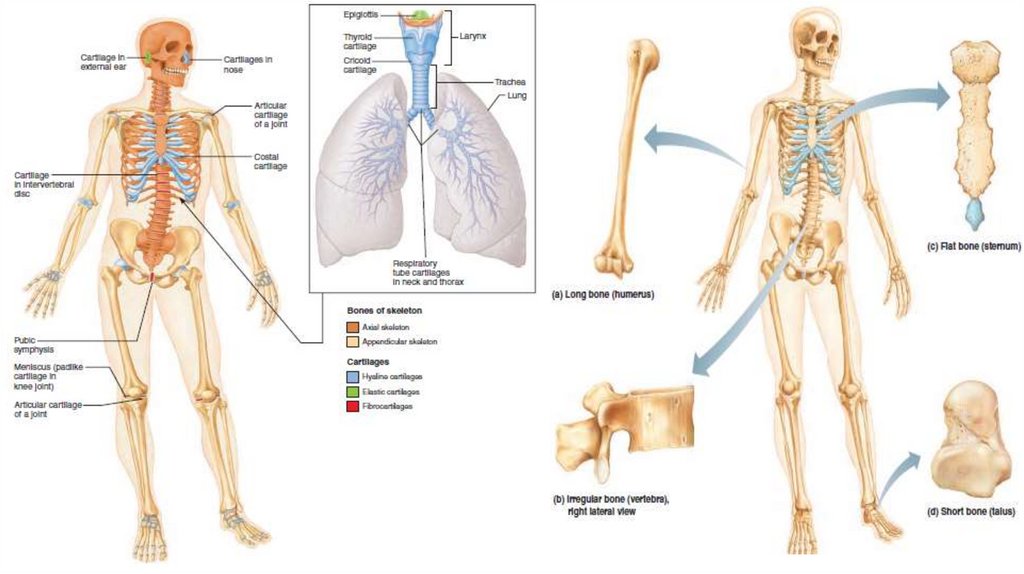
• The human skeleton is initially made up of cartilages and fibrous membranes , then they are replaced by bone andfew cartilages remain
• Skeletal cartilage is made of cartilage tissue molded to fit its body location and function
• Cartilages consists mainly of water that give them resilience ( spring back to original shape )
• Cartilage doesn’t have nerves or blood vessels , but it is surrounded by a layer of dense irregular connective tissue
( perichondrium ) that prevent outward expansion
• The perichondrium contains blood vessels from which nutrients diffuse through the matrix to reach the cartilage
cells internally , and this limit the cartilage thickness
• There are three types of cartilages in the body : hyaline, elastic, and fibrocartilage. They have all the basic
components cells called chondrocytes, encased in small cavities (lacunae) within an extracellular matrix containing
a jellylike ground substance and fibers.
• Hyaline cartilages, are the most abundant , which look like frosted glass , provide support with flexibility and
resilience. They have spherical chondrocyte and fine collagen fibers ( not detected by microscope ) , they include :
1.
2.
3.
4.
Articular cartilages : cover bones at movable joints
Costal cartilages : connect ribs to sternum
Respiratory cartilages : in larynx (voicebox) and reinforce other respiratory passageways
Nasal cartilages : support external nose
• Elastic cartilages resemble hyaline cartilages , they contain more stretchy elastic fibers ,they can found the
external ear and the epiglottis (the flap that bends to cover the opening of the larynx each time we swallow).
• Fibrocartilages Highly compressible with great tensile strength consist of roughly parallel rows of chondrocytes
alternating with thick collagen fibers , are found in site that are subjected to both pressure and stretch (menisci)
of the knee and the discs between vertebrae,
3. Growth of cartilage
• cartilage has a flexible matrix which can accommodate mitosis. So it’s ideal to the embryonic Skeletonand to provide new skeletal growth
• Growth can be appositional growth , cartilages form cells in the perichondrium that secrete matrix on
the external face of the existing cartilages
• Interstitial growth ,the lacunae divide and produce new matrix so expanding the cartilage within
• Cartilage growth ends during adolescence when the skeleton stops growing.
• calcified cartilage is not bone; cartilage and bone are always distinct tissues
• There are 206 bones in our bodies classified into
1.
2.
axial skeleton ( form the long axis of the body ex, bone of skull , vertebral column , rib cage ,and serve to protect and support
or carry other body parts )
Appendicular skeleton : ( upper and lower limbs and girdles- shoulder and hip bones that attach limbs to axial skeleton – bones
of the limbs help in movement and manipulate our environment )
• There are other classification based on shape and size , these differences help in serve and function in
different areas , as femur long bone with hollow-cylinder that provide the strength with minimum
weight , classes of bones :
1.
2.
3.
4.
5.
Long bones : are considerably longer than they are wide , and has a shaft and two expanded ends all limbs bones except wrist
patella and ankle ( fingers are long bones even they are small as classification based on elongation not overall size )
Short bones : are cube shaped bones like in ankle and wrist
Sesamoid bones : have a shape like sesame , are special type of short bones that form in tendon ( patella) , they act to alter the
direction of pull of a tendon
Flat bones : are flattened ( sternum or breast bone , scapulae , ribs , skull bones )
Irregular bones : have a complicated shape include the vertebrae and hip bones
4.
5. Function of bones
• Support : bones supports the body and cradles its soft organs ,ex, low limbs actas pillars of trunk , and rib cage supports the thoracic wall
• Protection : as they protect the brain , and vertebrae that protect spinal cord ,
and rib cage protects organs of the thoracic cavity
• Movement : the muscles use bones as leavers to move the body parts
• Mineral and growth factor storage. Bone is a reservoir for minerals, most
importantly calcium and phosphate, these minerals are released into the
bloodstream in the ionic form when needed , and bone matrix stores important
growth factors.
• Blood cell formation : most blood cell formation ( hematopoiesis ) occur in red
marrow cavities of certain bones
• Triglyceride ( fat ) : can be stored in the bone cavity
• Hormone production : Bones produce osteocalcin, a hormone which not only
helps regulate bone formation, but also protects against obesity, glucose
intolerance, and diabetes mellitus.
6. Bone structure
• Bones are organs because they contains differenttypes of tissues , so bone structure can be considered
at 3 levels :
• Gross anatomy :
1. Bone texture : compact and spongy bone : the outer layer
of the bone which is smooth and solid is the compact
bone , the inner layer is the spongy or trabecular bone
which is a honeycomb of small needle-like or flat pieces
(light beam ) trabeculae , and the spaces between
trabeculae are filled by red or yellow bone marrow
2. Structure of short ,irregular , flat bones : these types
share the same design , contains thin plates of spongy
bone covered by compact bone , these plates are covered
by connective tissue membranes periosteum and
endosteum , they are not cylindrical and contains bone
marrow but no well-defined marrow cavity , hyaline
cartilage covers bone in the joints region .Spongy bone in
flat bones is called diploe , and formed as sandwich
7.
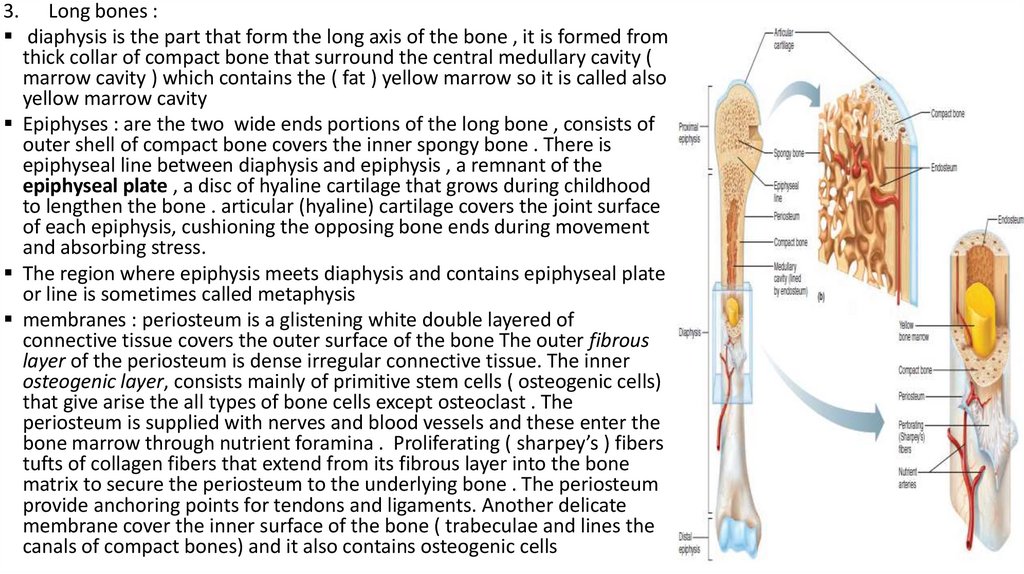
3. Long bones :diaphysis is the part that form the long axis of the bone , it is formed from
thick collar of compact bone that surround the central medullary cavity (
marrow cavity ) which contains the ( fat ) yellow marrow so it is called also
yellow marrow cavity
Epiphyses : are the two wide ends portions of the long bone , consists of
outer shell of compact bone covers the inner spongy bone . There is
epiphyseal line between diaphysis and epiphysis , a remnant of the
epiphyseal plate , a disc of hyaline cartilage that grows during childhood
to lengthen the bone . articular (hyaline) cartilage covers the joint surface
of each epiphysis, cushioning the opposing bone ends during movement
and absorbing stress.
The region where epiphysis meets diaphysis and contains epiphyseal plate
or line is sometimes called metaphysis
membranes : periosteum is a glistening white double layered of
connective tissue covers the outer surface of the bone The outer fibrous
layer of the periosteum is dense irregular connective tissue. The inner
osteogenic layer, consists mainly of primitive stem cells ( osteogenic cells)
that give arise the all types of bone cells except osteoclast . The
periosteum is supplied with nerves and blood vessels and these enter the
bone marrow through nutrient foramina . Proliferating ( sharpey’s ) fibers
tufts of collagen fibers that extend from its fibrous layer into the bone
matrix to secure the periosteum to the underlying bone . The periosteum
provide anchoring points for tendons and ligaments. Another delicate
membrane cover the inner surface of the bone ( trabeculae and lines the
canals of compact bones) and it also contains osteogenic cells
8.
Location of hematopoietic tissue in bones : hematopoietic tissue , red marrow ,is found in trabecular cavity in spongy bone in long bones or diploe in flat
bones, so both cavities are called red marrow cavities , in infants all spongy
bone cavities contain red marrow , but in adults the red marrow is in the
epiphysis in the head of long bones ( femur and humerus ) . The red marrow
found in the diploe of flat bones ( sternum ) in some irregular bones (such
as the hip bone) is much more active in hematopoiesis , clinicians obtain red
marrow from there . Yellow marrow in medullary cavity can revert to red
marrow as happen in anemia
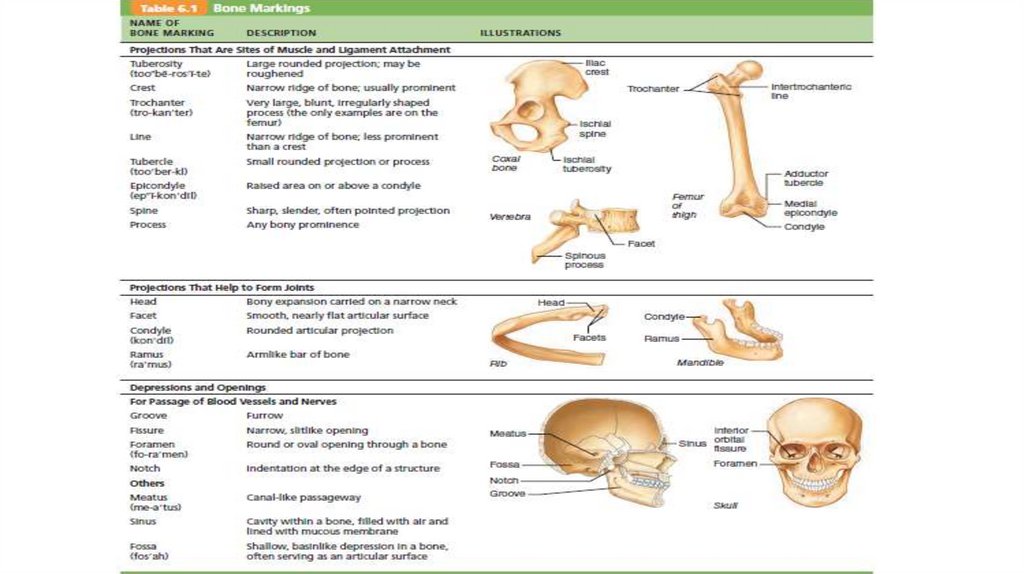
bone markings serve as sites of muscle, ligament, and tendon attachment, as
joint surfaces, or as conduits for blood vessels and nerves. They can be
projections ( heads , trochanters , spines ) projections indicate the stresses
created by muscles attached to and pulling on them, or depression or opening
(fossae , sinuses, foramina, grooves )
9.
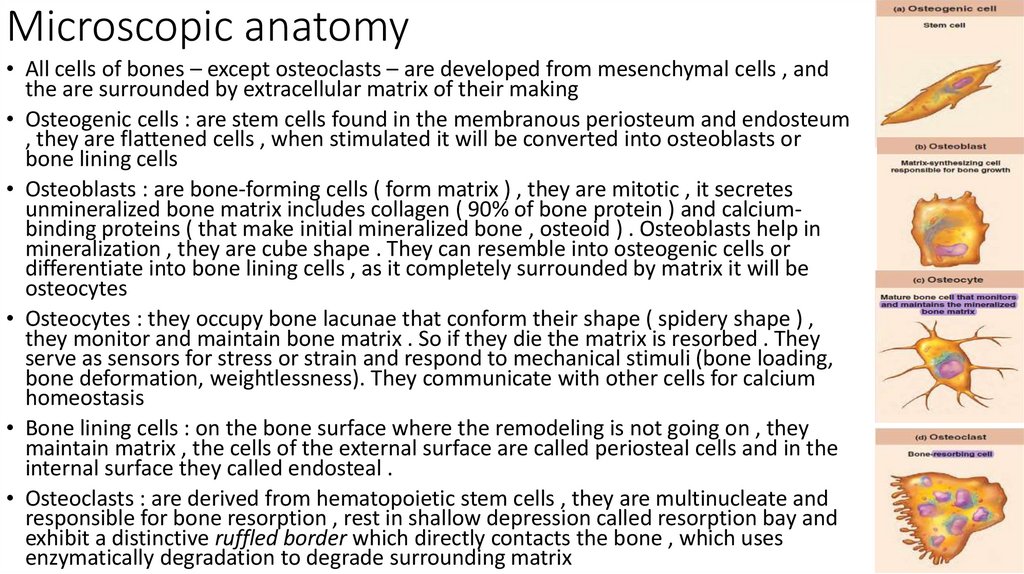
10. Microscopic anatomy
• All cells of bones – except osteoclasts – are developed from mesenchymal cells , andthe are surrounded by extracellular matrix of their making
• Osteogenic cells : are stem cells found in the membranous periosteum and endosteum
, they are flattened cells , when stimulated it will be converted into osteoblasts or
bone lining cells
• Osteoblasts : are bone-forming cells ( form matrix ) , they are mitotic , it secretes
unmineralized bone matrix includes collagen ( 90% of bone protein ) and calciumbinding proteins ( that make initial mineralized bone , osteoid ) . Osteoblasts help in
mineralization , they are cube shape . They can resemble into osteogenic cells or
differentiate into bone lining cells , as it completely surrounded by matrix it will be
osteocytes
• Osteocytes : they occupy bone lacunae that conform their shape ( spidery shape ) ,
they monitor and maintain bone matrix . So if they die the matrix is resorbed . They
serve as sensors for stress or strain and respond to mechanical stimuli (bone loading,
bone deformation, weightlessness). They communicate with other cells for calcium
homeostasis
• Bone lining cells : on the bone surface where the remodeling is not going on , they
maintain matrix , the cells of the external surface are called periosteal cells and in the
internal surface they called endosteal .
• Osteoclasts : are derived from hematopoietic stem cells , they are multinucleate and
responsible for bone resorption , rest in shallow depression called resorption bay and
exhibit a distinctive ruffled border which directly contacts the bone , which uses
enzymatically degradation to degrade surrounding matrix
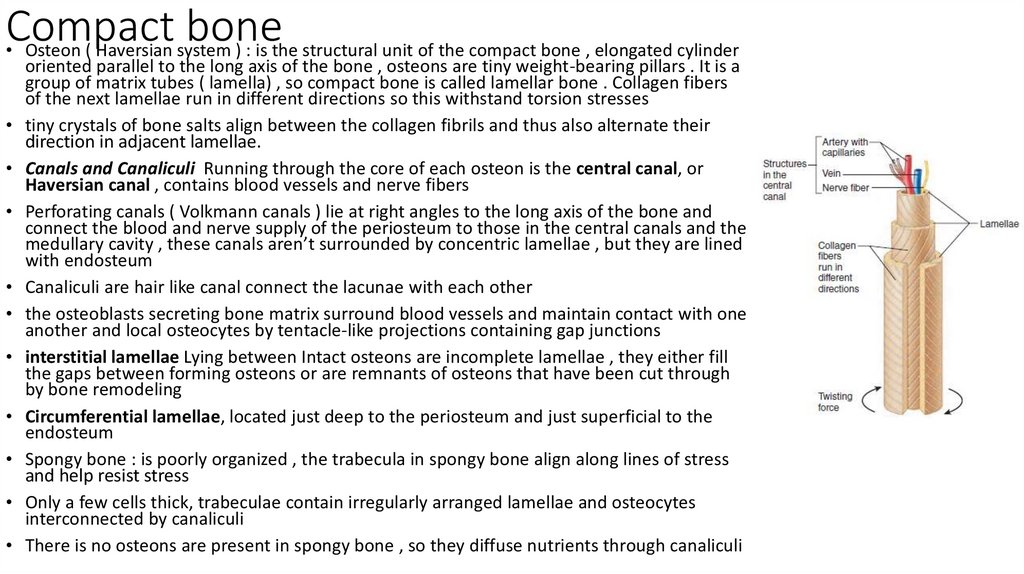
11. Compact bone
• Osteon ( Haversian system ) : is the structural unit of the compact bone , elongated cylinderoriented parallel to the long axis of the bone , osteons are tiny weight-bearing pillars . It is a
group of matrix tubes ( lamella) , so compact bone is called lamellar bone . Collagen fibers
of the next lamellae run in different directions so this withstand torsion stresses
tiny crystals of bone salts align between the collagen fibrils and thus also alternate their
direction in adjacent lamellae.
Canals and Canaliculi Running through the core of each osteon is the central canal, or
Haversian canal , contains blood vessels and nerve fibers
Perforating canals ( Volkmann canals ) lie at right angles to the long axis of the bone and
connect the blood and nerve supply of the periosteum to those in the central canals and the
medullary cavity , these canals aren’t surrounded by concentric lamellae , but they are lined
with endosteum
Canaliculi are hair like canal connect the lacunae with each other
the osteoblasts secreting bone matrix surround blood vessels and maintain contact with one
another and local osteocytes by tentacle-like projections containing gap junctions
interstitial lamellae Lying between Intact osteons are incomplete lamellae , they either fill
the gaps between forming osteons or are remnants of osteons that have been cut through
by bone remodeling
Circumferential lamellae, located just deep to the periosteum and just superficial to the
endosteum
Spongy bone : is poorly organized , the trabecula in spongy bone align along lines of stress
and help resist stress
Only a few cells thick, trabeculae contain irregularly arranged lamellae and osteocytes
interconnected by canaliculi
There is no osteons are present in spongy bone , so they diffuse nutrients through canaliculi
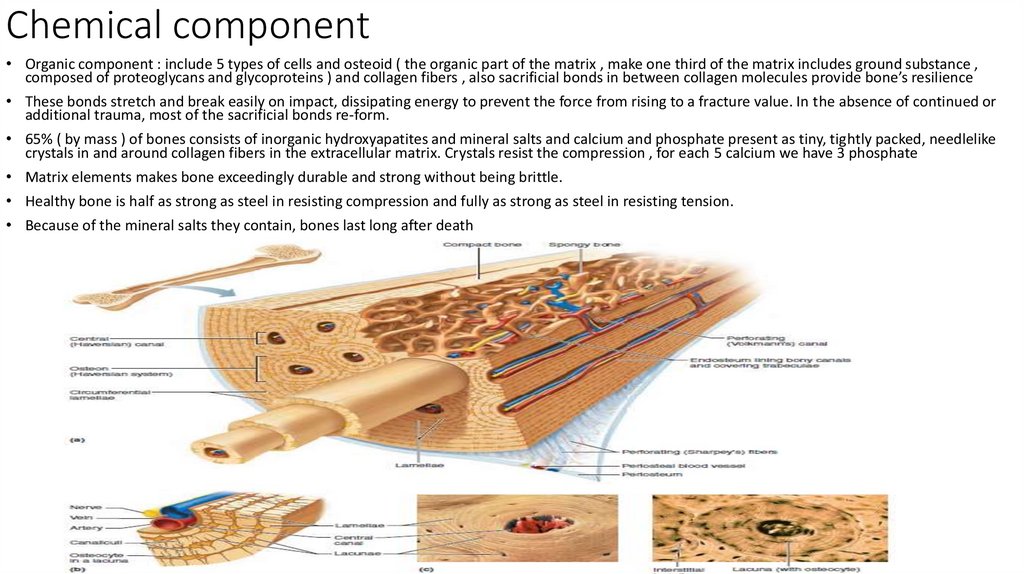
12. Chemical component
• Organic component : include 5 types of cells and osteoid ( the organic part of the matrix , make one third of the matrix includes ground substance ,composed of proteoglycans and glycoproteins ) and collagen fibers , also sacrificial bonds in between collagen molecules provide bone’s resilience
• These bonds stretch and break easily on impact, dissipating energy to prevent the force from rising to a fracture value. In the absence of continued or
additional trauma, most of the sacrificial bonds re-form.
• 65% ( by mass ) of bones consists of inorganic hydroxyapatites and mineral salts and calcium and phosphate present as tiny, tightly packed, needlelike
crystals in and around collagen fibers in the extracellular matrix. Crystals resist the compression , for each 5 calcium we have 3 phosphate
• Matrix elements makes bone exceedingly durable and strong without being brittle.
• Healthy bone is half as strong as steel in resisting compression and fully as strong as steel in resisting tension.
• Because of the mineral salts they contain, bones last long after death
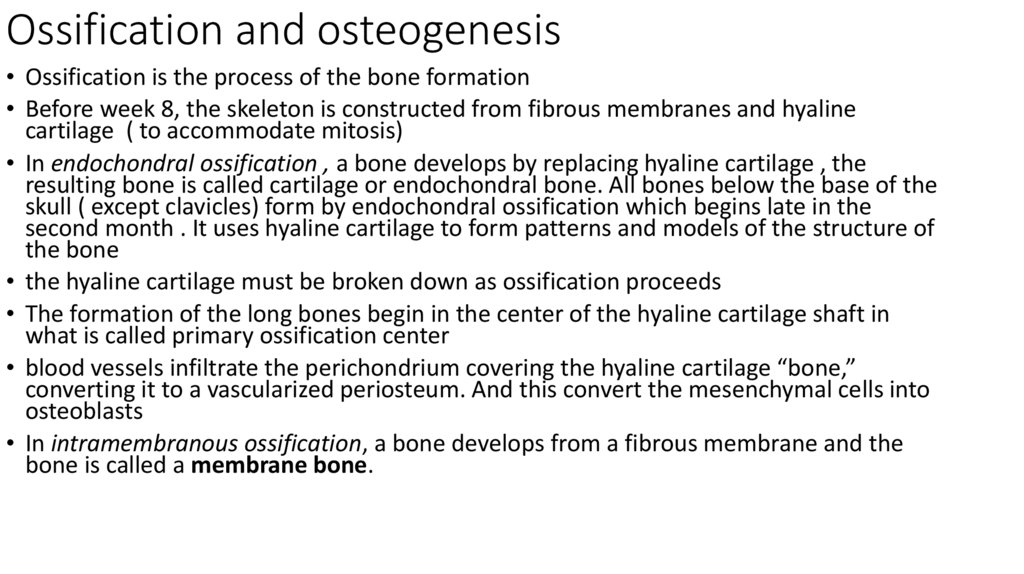
13. Ossification and osteogenesis
• Ossification is the process of the bone formation• Before week 8, the skeleton is constructed from fibrous membranes and hyaline
cartilage ( to accommodate mitosis)
• In endochondral ossification , a bone develops by replacing hyaline cartilage , the
resulting bone is called cartilage or endochondral bone. All bones below the base of the
skull ( except clavicles) form by endochondral ossification which begins late in the
second month . It uses hyaline cartilage to form patterns and models of the structure of
the bone
• the hyaline cartilage must be broken down as ossification proceeds
• The formation of the long bones begin in the center of the hyaline cartilage shaft in
what is called primary ossification center
• blood vessels infiltrate the perichondrium covering the hyaline cartilage “bone,”
converting it to a vascularized periosteum. And this convert the mesenchymal cells into
osteoblasts
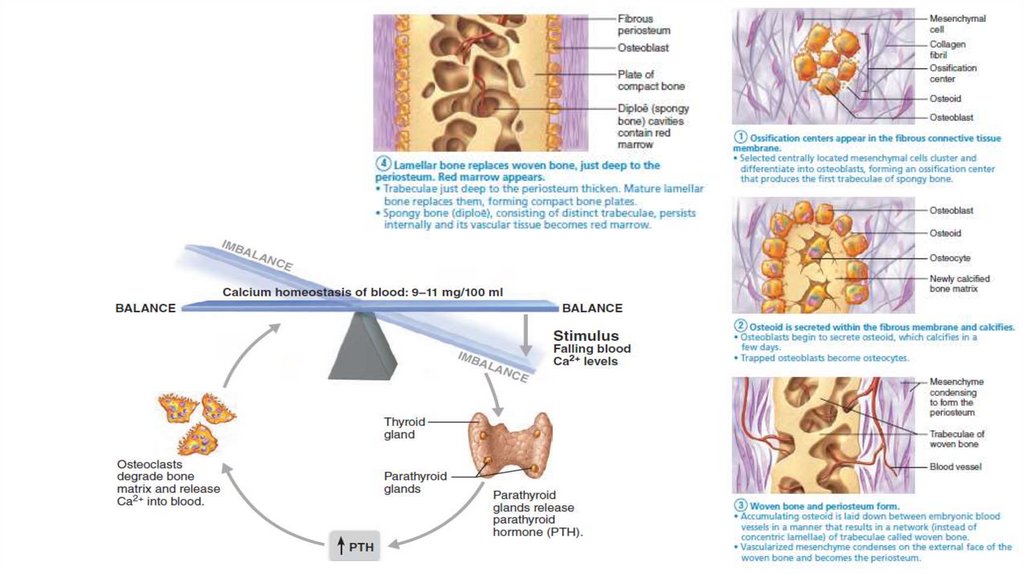
• In intramembranous ossification, a bone develops from a fibrous membrane and the
bone is called a membrane bone.
14. Enchorial ossification
1.A bone collar forms around the diaphysis of the hyaline cartilage model. As the osteoblast secrets osteoid against the hyaline cartilage diaphysis
encasing in what is called periosteal bone collar
2.
Cartilage in the center of the diaphysis calcifies and then develops cavities chondrocytes within the shaft hypertrophy (enlarge) and signal the
surrounding cartilage matrix to calcify. Calcified cartilage matrix is permeable to diffusing nutrients so the chondrocyte die and the matrix begins to
deteriorate to open cavities and collar stabilize the cartilage model
3.
The periosteal bud invades the internal cavities and spongy bone forms. In month 3, the forming cavities are invaded by a collection of elements
called the periosteal bud, which contains a nutrient artery and vein, nerve fibers, red marrow elements, osteogenic cells(become osteoblast and
secrete osteoid around the remaining calcified fragments of hyaline cartilage forming bone-covered cartilage trabeculae), and osteoclasts ( erode the
calcified cartilage matrix )
4.
The diaphysis elongates and a medullary cavity forms : as the primary ossification center enlarges , osteoclast break down spongy bone to form
medullary cavity in the center of diaphysis. The epiphysis consists of cartilage only and the hyaline cartilage continue to elongate by division ( week
9 until birth )
5.
The epiphysis ossification : before or after birth , secondary ossification centers appear , so the cartilage in epiphysis calcifies and deteriorates
opening up cavities and allow periosteal bud to enter then the trabeculae appear ( long bones have 2 , short 1 , irregular several )
• The primary and secondary ossification are almost the same except that the spongy bone is retained and no medullary cavity
• Hyaline cartilage remain at : On the epiphyseal surfaces, as the articular cartilages . At the junction of the diaphysis and epiphysis, where it forms the
epiphyseal plates
• Intramembranous ossification forms the cranial bones of the skull and clavicles at the week 8 from fibrous connective tissue membranes formed from
mesenchymal cells
15. Growth in length
• Interstitial growth , is the growth in length of long bones like endochondralossification
• Resting or quiescent zone the part of the epiphyseal plate facing the epiphysis
• The cartilage of the epiphyseal plate form tall columns like coins in stack
• The cells at the “top” (epiphysis-facing) side of the stack abutting the resting zone
comprise the proliferation or growth zone , this push the epiphysis away from
diaphysis
• the older chondrocytes in the stack, which are closer to the diaphysis (hypertrophic
zone ) hypertrophy, and their lacunae erode and enlarge, leaving large interconnecting
spaces.
• the surrounding cartilage matrix calcifies and these chondrocytes die and deteriorate,
producing the calcification zone
• This leaves long slender spicules of calcified cartilage at the epiphysis-diaphysis
junction. These calcified spicules ultimately become part of the ossification or
osteogenic zone, and are invaded by marrow elements from the medullary cavity(
osteoclast digest the spicule tips , osteoblast that form spongy bone)
• Longitudinal growth is accompanied by almost continuous remodeling of the
epiphyseal ends to maintain the proportion between the diaphysis and epiphyses.
• the chondroblasts of the epiphyseal plates divide less often and the plates become
thinner and thinner until they are entirely replaced by bone tissue ( epiphyseal plate
closure 18 in females , 21 in males )
16. Growth in Width (Thickness)
• adult bone can still widen by appositional growth if stressed by excessivemuscle activity or body weight.
• Osteoblasts beneath the periosteum secrete bone matrix on the external
bone surface as osteoclasts on the endosteal surface of the diaphysis
remove bone ( slightly more building up than breaking down) so it
becomes stronger and thicker but not heavier
• During infancy and childhood growth hormone stimulate epiphyseal
plate ( anterior pituitary gland ) , then thyroid hormones modulate the
activity of growth hormone ensuring that the skeleton has proper
proportions as it grows.
• At puberty , male and female sex hormones ( testosterone and estrogen )
promote the growth spurt typical of adolescence, and masculinization
and feminization of skeleton
• Hyper secretion of GH leads to gigantism and deficits leads to dwarfism
• Every week we recycle 5-7% of our bone mass , and 0.5 gram enter or
leave our skeleton every day . Spongy bone is replaced every 3 to 4
years and compact every 10 years
17. Bone remodeling
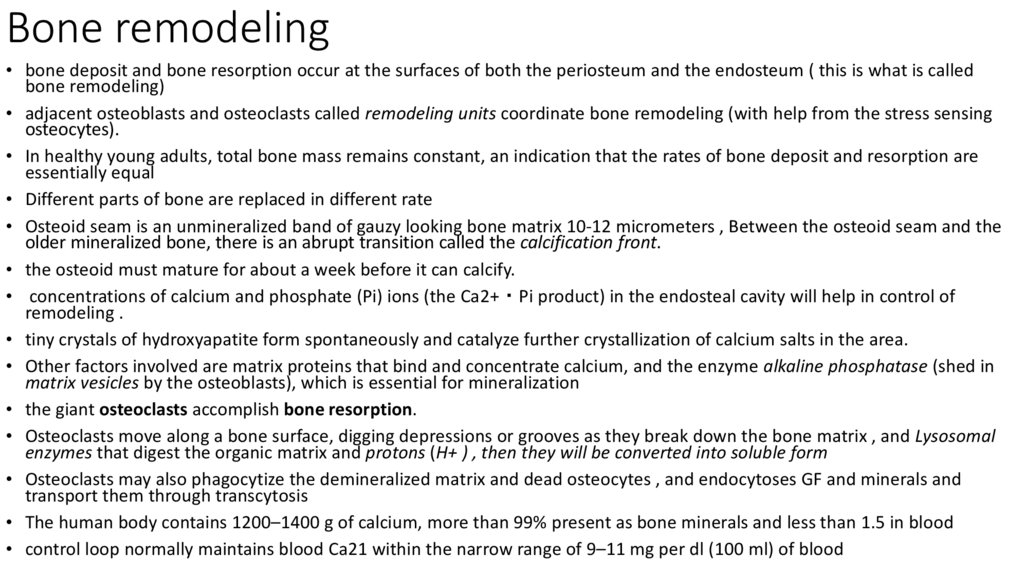
• bone deposit and bone resorption occur at the surfaces of both the periosteum and the endosteum ( this is what is calledbone remodeling)
• adjacent osteoblasts and osteoclasts called remodeling units coordinate bone remodeling (with help from the stress sensing
osteocytes).
• In healthy young adults, total bone mass remains constant, an indication that the rates of bone deposit and resorption are
essentially equal
• Different parts of bone are replaced in different rate
• Osteoid seam is an unmineralized band of gauzy looking bone matrix 10-12 micrometers , Between the osteoid seam and the
older mineralized bone, there is an abrupt transition called the calcification front.
• the osteoid must mature for about a week before it can calcify.
• concentrations of calcium and phosphate (Pi) ions (the Ca2+・Pi product) in the endosteal cavity will help in control of
remodeling .
• tiny crystals of hydroxyapatite form spontaneously and catalyze further crystallization of calcium salts in the area.
• Other factors involved are matrix proteins that bind and concentrate calcium, and the enzyme alkaline phosphatase (shed in
matrix vesicles by the osteoblasts), which is essential for mineralization
• the giant osteoclasts accomplish bone resorption.
• Osteoclasts move along a bone surface, digging depressions or grooves as they break down the bone matrix , and Lysosomal
enzymes that digest the organic matrix and protons (H+ ) , then they will be converted into soluble form
• Osteoclasts may also phagocytize the demineralized matrix and dead osteocytes , and endocytoses GF and minerals and
transport them through transcytosis
• The human body contains 1200–1400 g of calcium, more than 99% present as bone minerals and less than 1.5 in blood
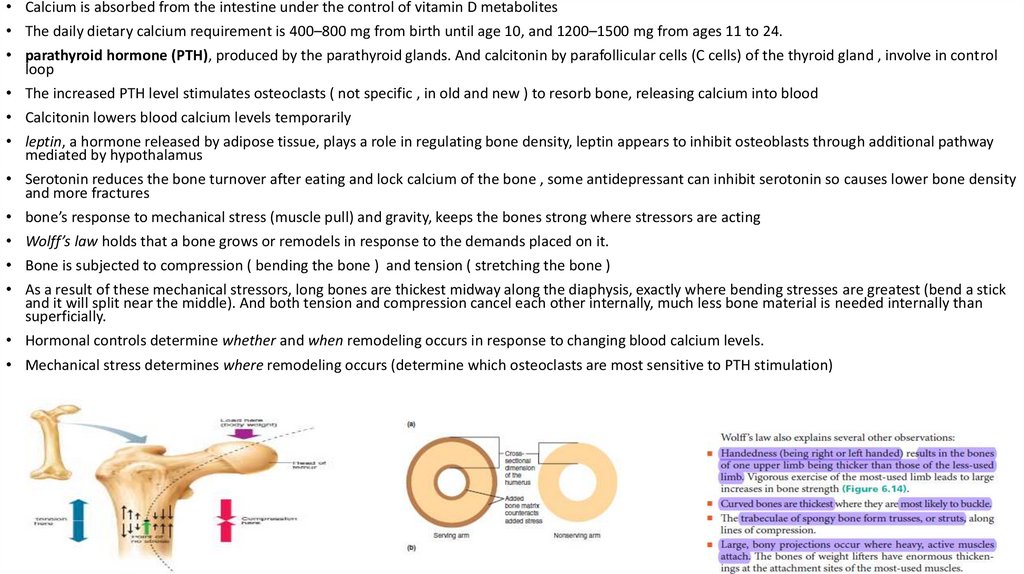
• control loop normally maintains blood Ca21 within the narrow range of 9–11 mg per dl (100 ml) of blood
18.
• Calcium is absorbed from the intestine under the control of vitamin D metabolites• The daily dietary calcium requirement is 400–800 mg from birth until age 10, and 1200–1500 mg from ages 11 to 24.
• parathyroid hormone (PTH), produced by the parathyroid glands. And calcitonin by parafollicular cells (C cells) of the thyroid gland , involve in control
loop
• The increased PTH level stimulates osteoclasts ( not specific , in old and new ) to resorb bone, releasing calcium into blood
• Calcitonin lowers blood calcium levels temporarily
• leptin, a hormone released by adipose tissue, plays a role in regulating bone density, leptin appears to inhibit osteoblasts through additional pathway
mediated by hypothalamus
• Serotonin reduces the bone turnover after eating and lock calcium of the bone , some antidepressant can inhibit serotonin so causes lower bone density
and more fractures
• bone’s response to mechanical stress (muscle pull) and gravity, keeps the bones strong where stressors are acting
• Wolff’s law holds that a bone grows or remodels in response to the demands placed on it.
• Bone is subjected to compression ( bending the bone ) and tension ( stretching the bone )
• As a result of these mechanical stressors, long bones are thickest midway along the diaphysis, exactly where bending stresses are greatest (bend a stick
and it will split near the middle). And both tension and compression cancel each other internally, much less bone material is needed internally than
superficially.
• Hormonal controls determine whether and when remodeling occurs in response to changing blood calcium levels.
• Mechanical stress determines where remodeling occurs (determine which osteoclasts are most sensitive to PTH stimulation)
19.
20. Bone Repair
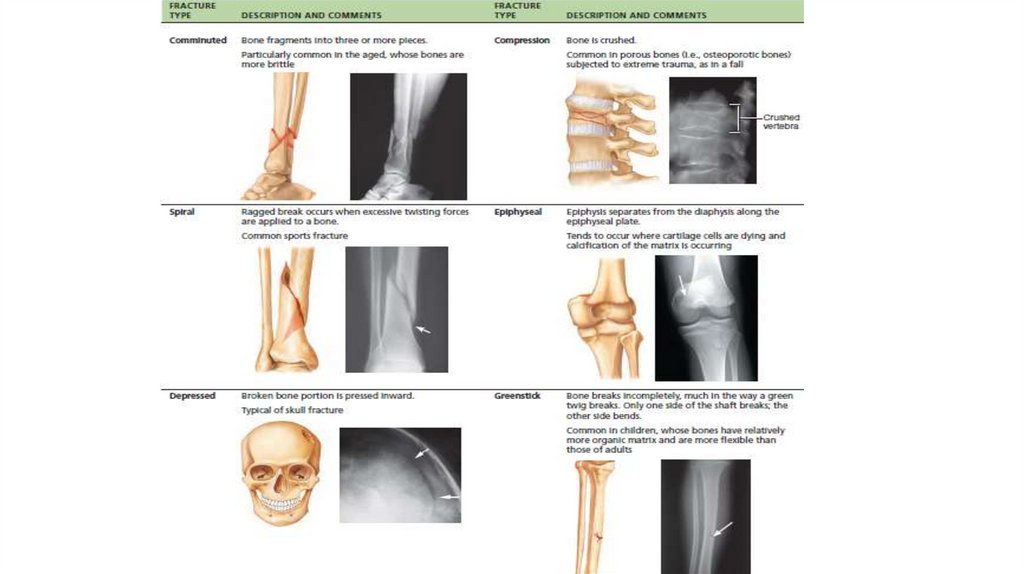
• Fractures may be classified by :1.
2.
3.
Position of the bone ends after fracture: In nondisplaced fractures, the bone
ends retain their normal position. In displaced fractures, the bone ends are
out of normal alignment.
Completeness of the break: If the bone is broken through, the fracture is a
complete fracture. If not, it is an incomplete fracture.
Whether the bone ends penetrate the skin: If so, the fracture is an open
(compound) fracture. If not, it is a closed (simple) fracture.
• There are two types of reduction (the realignment of the broken bone
ends ) treatment : external coax the bone ends into position. In open
(internal) reduction, the bone ends are secured together surgically with
pins or wires
• simple fracture of small or medium-sized bones in young adults heals in
six to eight weeks , but it takes much longer for large, weight-bearing
bones and for bones of elderly people (because of their poorer
circulation)





 biology
biology