Similar presentations:
HCV Case Study. Treat Now or Wait for New Therapies
1.
HCV Case StudyTreat Now or Wait for New Therapies
2.
Program Disclosure• This activity has been planned and implemented in
accordance with the Essential Areas and Policies of the
Accreditation Council for Continuing Medical Education
(ACCME) through the sponsorship of Annenberg Center for
Health Sciences at Eisenhower and the Chronic Liver Disease
Foundation. Annenberg Center for Health Sciences at
Eisenhower is accredited by the ACCME to provide continuing
medical education for physicians.
• This program is supported by educational grants from
Kadmon and Merck Pharmaceuticals.
3.
Learning Objectives• Describe current data on approved and experimental
DAA’s used in combination with Pegylated Interferon and
Ribavirin
• Define the benefits and risks of treating now versus
delaying therapy for different patient populations
4.
Glenn: Patient Characteristics• 55 year old male
• Shift worker
• History/risk factors
– BMI=34
– Hypertension and dyslipidemia
– Moderate drinker/cigarette smoker
• Concomitant medications
– Simvastatin 20 mg/day
– Lisinopril 10 mg/day
5.
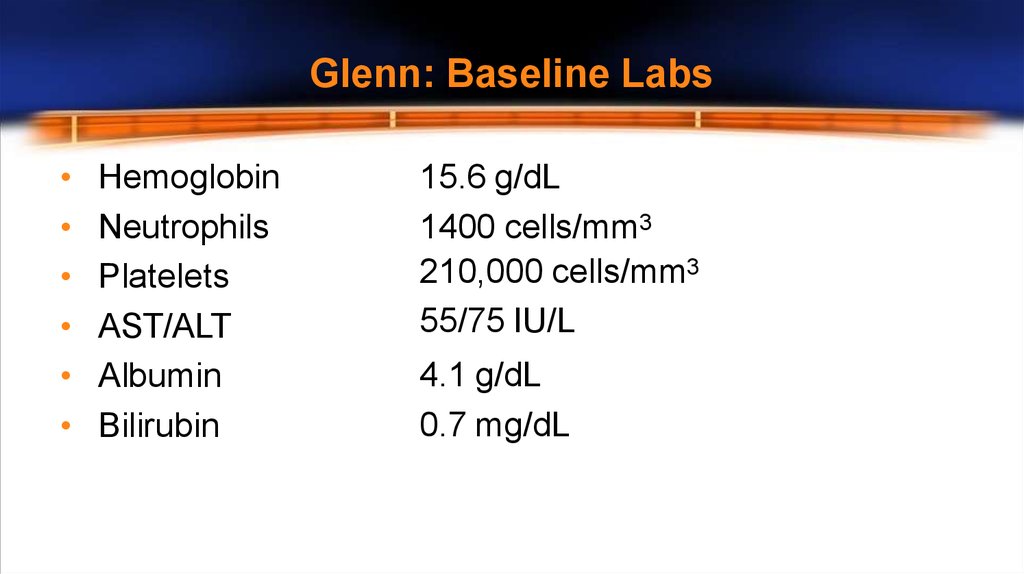
Glenn: Baseline LabsHemoglobin
Neutrophils
Platelets
AST/ALT
Albumin
Bilirubin
15.6 g/dL
1400 cells/mm3
210,000 cells/mm3
55/75 IU/L
4.1 g/dL
0.7 mg/dL
6.
Glenn: Disease CharacteristicsTreatment naïve
Genotype
IL28B
METAVIR
BL viral load
1a
CC
F3
1,300,000 IU/mL
7.
Clinical Decision 1• How would you manage this patient?
1. Continue to monitor patient but do not start treatment
2. Start patient on first generation protease inhibitor/PEG-IFN/RBV
8.
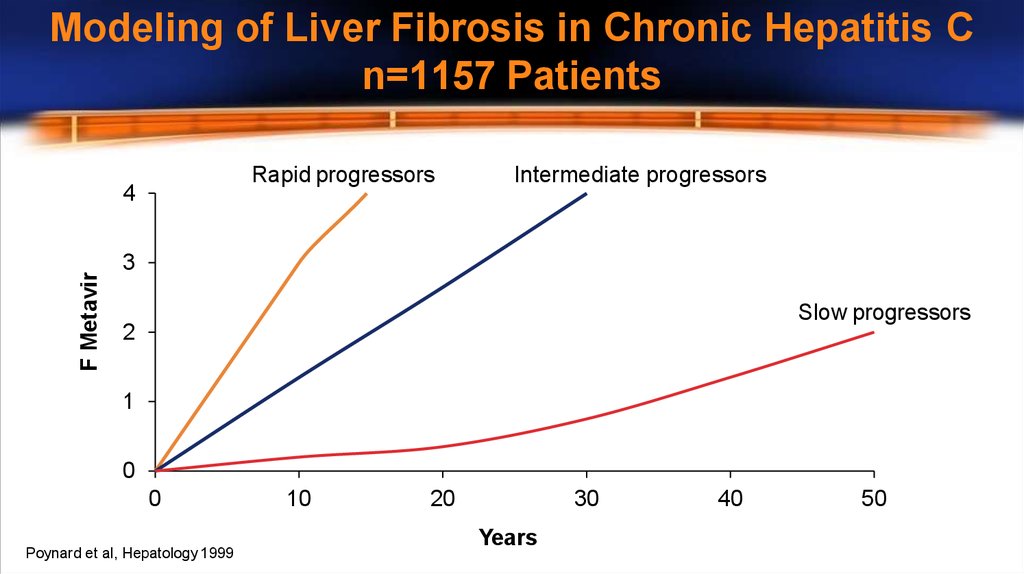
Modeling of Liver Fibrosis in Chronic Hepatitis Cn=1157 Patients
Rapid progressors
F Metavir
4
Intermediate progressors
3
Slow progressors
2
1
0
0
Poynard et al, Hepatology 1999
10
20
30
Years
40
50
9.
Cumulative Proportion of Patients Transitioning fromCompensated to Decompensated Stage Over Time
Proportion of Patients
1.00
0.75
0.50
0.25
0.00
Pts at risk
0
24
48
72
96
120
806
513
402
302
243
217
D’Amico G et al. J Hepatol. 2006;44:217-231.
months
10.
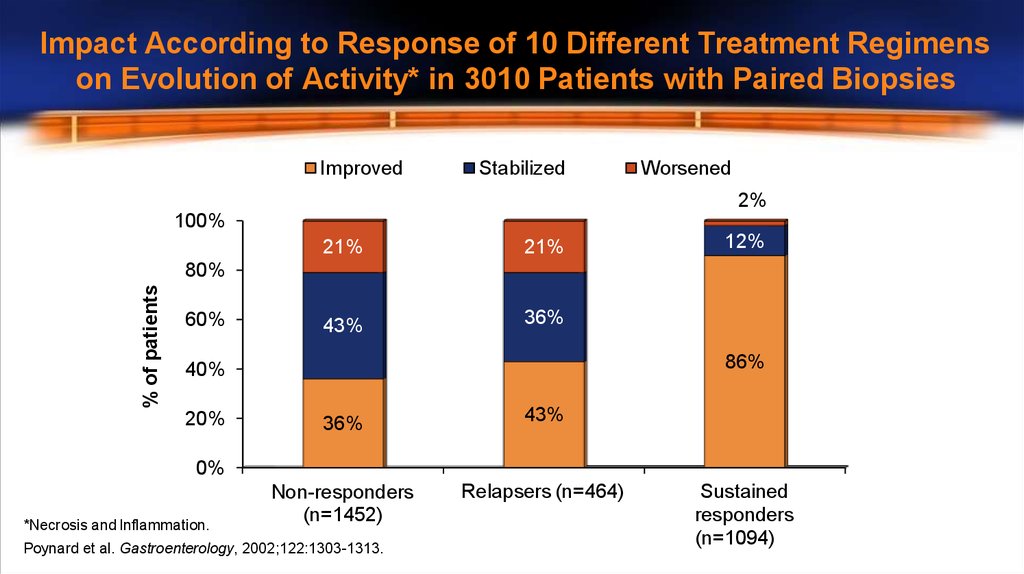
Impact According to Response of 10 Different Treatment Regimenson Evolution of Activity* in 3010 Patients with Paired Biopsies
Improved
Stabilized
Worsened
2%
100%
21%
21%
43%
36%
12%
% of patients
80%
60%
86%
40%
20%
36%
43%
Non-responders
(n=1452)
Relapsers (n=464)
0%
*Necrosis and Inflammation.
Poynard et al. Gastroenterology, 2002;122:1303-1313.
Sustained
responders
(n=1094)
11.
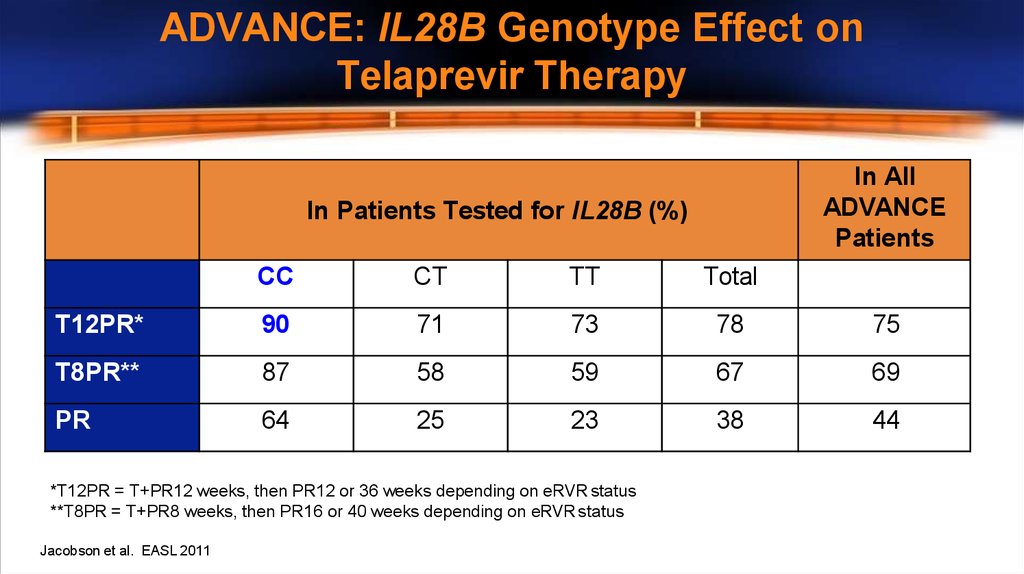
ADVANCE: IL28B Genotype Effect onTelaprevir Therapy
In All
ADVANCE
Patients
In Patients Tested for IL28B (%)
CC
CT
TT
Total
T12PR*
90
71
73
78
75
T8PR**
87
58
59
67
69
PR
64
25
23
38
44
*T12PR = T+PR12 weeks, then PR12 or 36 weeks depending on eRVR status
**T8PR = T+PR8 weeks, then PR16 or 40 weeks depending on eRVR status
Jacobson et al. EASL 2011
12.
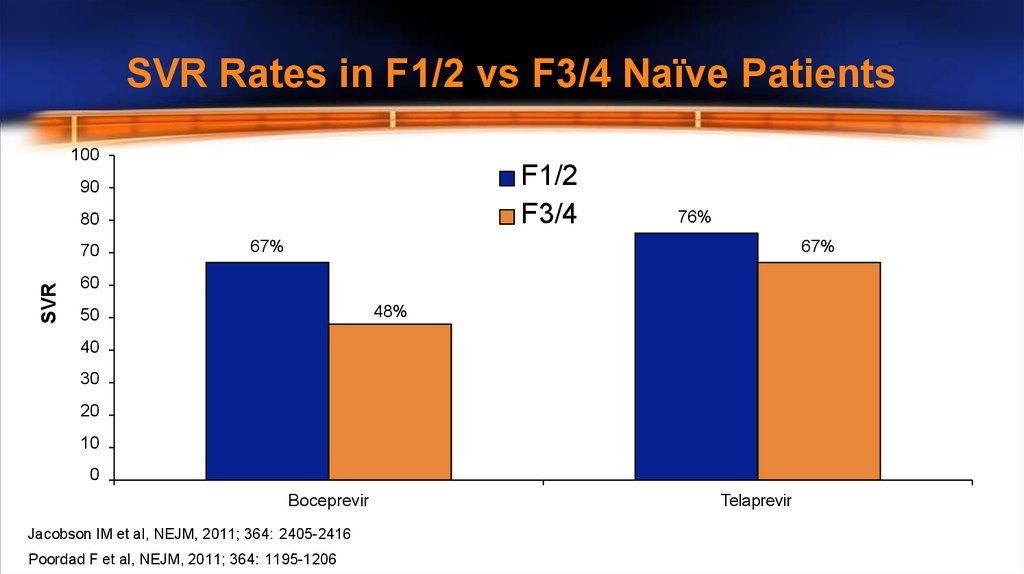
SVR Rates in F1/2 vs F3/4 Naïve Patients100
F1/2
F3/4
90
80
SVR
70
76%
67%
67%
60
48%
50
40
30
20
10
0
Boceprevir
Jacobson IM et al, NEJM, 2011; 364: 2405-2416
Poordad F et al, NEJM, 2011; 364: 1195-1206
Telaprevir
13.
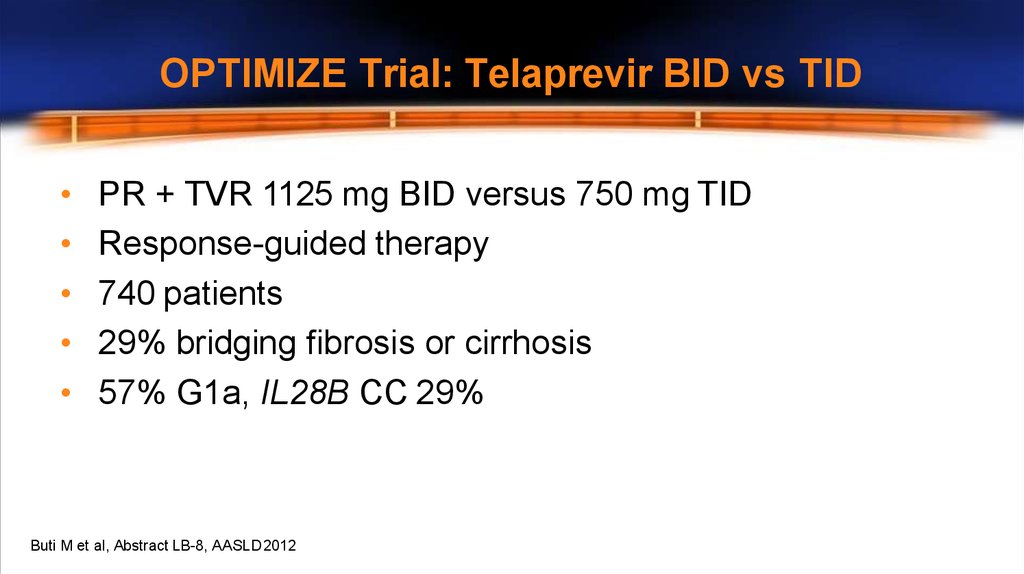
OPTIMIZE Trial: Telaprevir BID vs TIDPR + TVR 1125 mg BID versus 750 mg TID
Response-guided therapy
740 patients
29% bridging fibrosis or cirrhosis
57% G1a, IL28B CC 29%
Buti M et al, Abstract LB-8, AASLD2012
14.
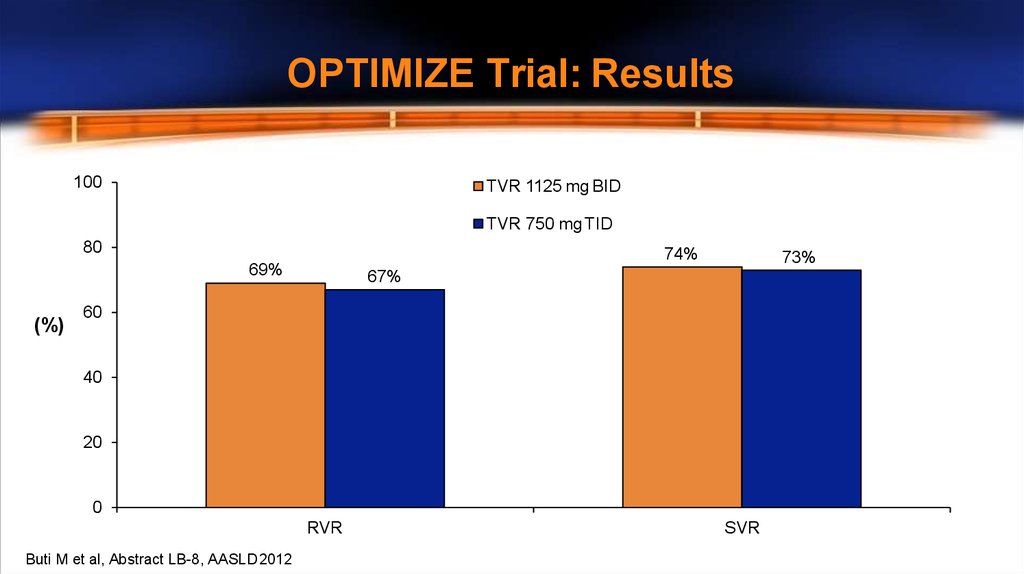
OPTIMIZE Trial: Results100
TVR 1125 mg BID
TVR 750 mg TID
80
74%
69%
(%)
73%
67%
60
40
20
0
RVR
Buti M et al, Abstract LB-8, AASLD2012
SVR
15.
Should Glenn Be Treated Now?• F3 disease – risk of progression with waiting
• IL28B CC
• Potential BID option is attractive
16.
The Case for Waiting• Multiple issues with current therapy
–
–
–
–
Compliance – pill burden
Co-morbidities
Adverse effects
New treatments on the horizon
17.
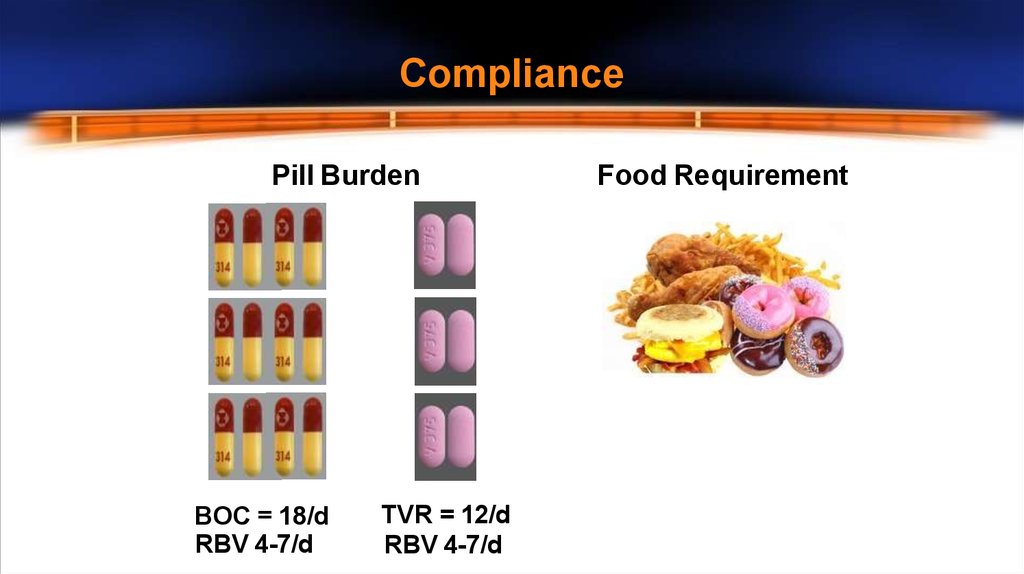
CompliancePill Burden
BOC = 18/d
RBV 4-7/d
TVR = 12/d
RBV 4-7/d
Food Requirement
18.
Co-Morbidities• Cardiac Risk Factors
– Hypertension, hyperlipidemia, smoker
• Pre Treatment
– DDI – Statin with TVR/BOC likely just stop it
• On Treatment
– Anemia management consider pre-treatment cardiac testing
19.
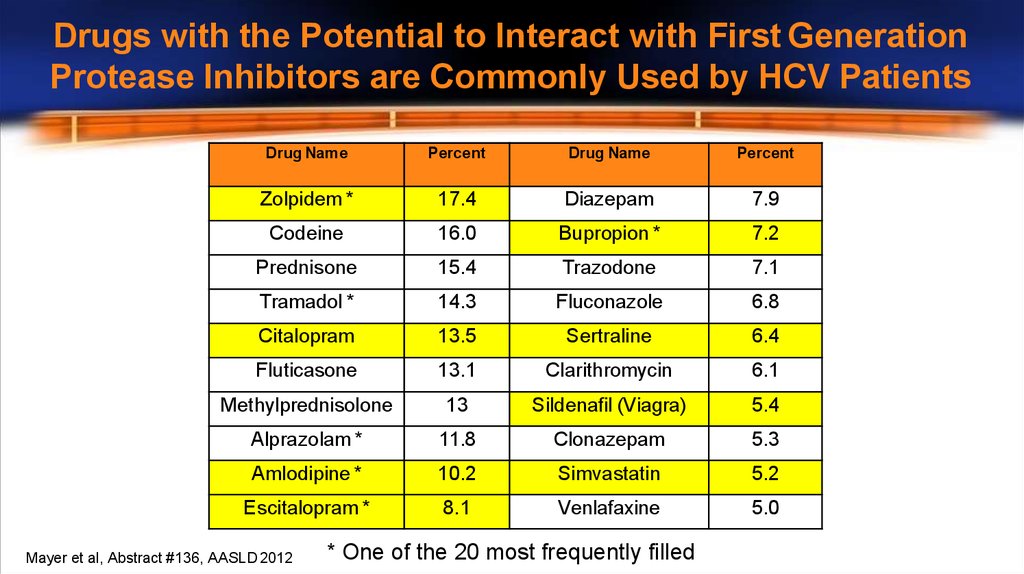
Drugs with the Potential to Interact with First GenerationProtease Inhibitors are Commonly Used by HCV Patients
Drug Name
Percent
Drug Name
Percent
Zolpidem *
17.4
Diazepam
7.9
Codeine
16.0
Bupropion *
7.2
Prednisone
15.4
Trazodone
7.1
Tramadol *
14.3
Fluconazole
6.8
Citalopram
13.5
Sertraline
6.4
Fluticasone
13.1
Clarithromycin
6.1
Methylprednisolone
13
Sildenafil (Viagra)
5.4
Alprazolam *
11.8
Clonazepam
5.3
Amlodipine *
10.2
Simvastatin
5.2
Escitalopram *
8.1
Venlafaxine
5.0
Mayer et al, Abstract #136, AASLD 2012
* One of the 20 most frequently filled
20.
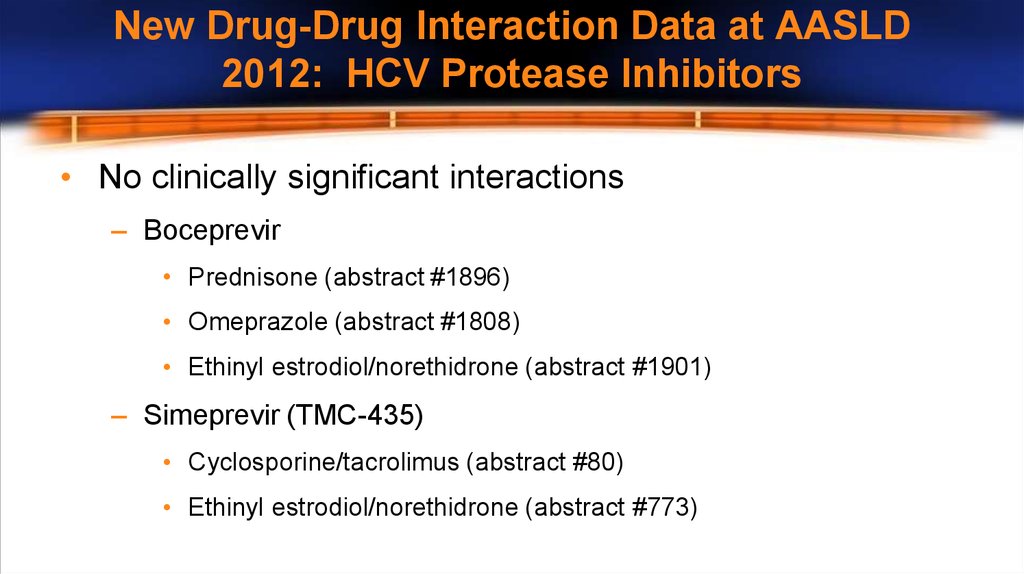
New Drug-Drug Interaction Data at AASLD2012: HCV Protease Inhibitors
• No clinically significant interactions
– Boceprevir
• Prednisone (abstract #1896)
• Omeprazole (abstract #1808)
• Ethinyl estrodiol/norethidrone (abstract #1901)
– Simeprevir (TMC-435)
• Cyclosporine/tacrolimus (abstract #80)
• Ethinyl estrodiol/norethidrone (abstract #773)
21.
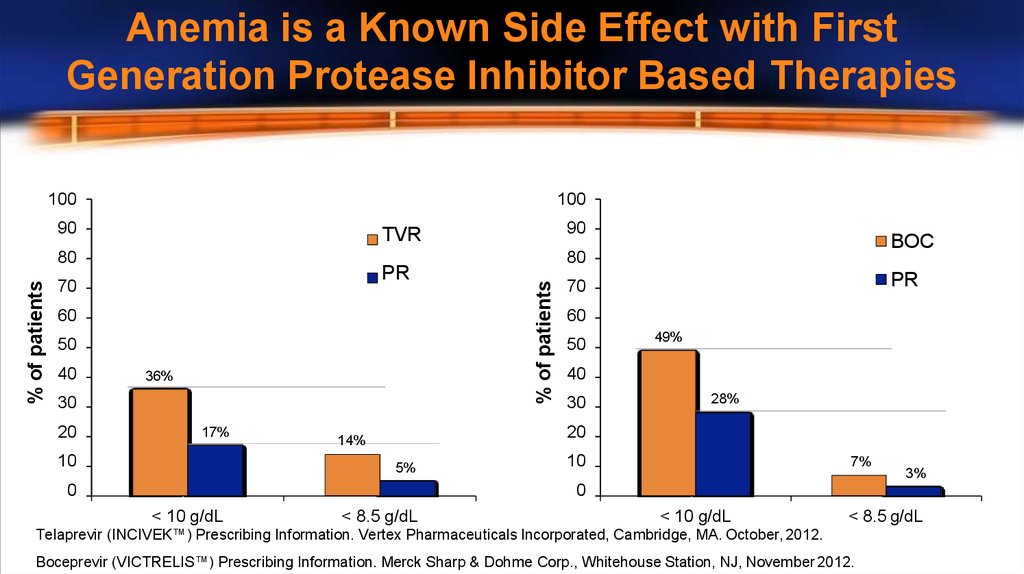
Anemia is a Known Side Effect with FirstGeneration Protease Inhibitor Based Therapies
100
100
90
PR
70
60
50
36%
30
20
17%
10
BOC
80
% of patients
% of patients
80
40
90
TVR
PR
70
60
50
49%
40
30
28%
20
14%
5%
0
10
7%
3%
0
< 10 g/dL
< 8.5 g/dL
< 10 g/dL
< 8.5 g/dL
Telaprevir (INCIVEK™) Prescribing Information. Vertex Pharmaceuticals Incorporated, Cambridge, MA. October, 2012.
Boceprevir (VICTRELIS™) Prescribing Information. Merck Sharp & Dohme Corp., Whitehouse Station, NJ, November 2012.
22.
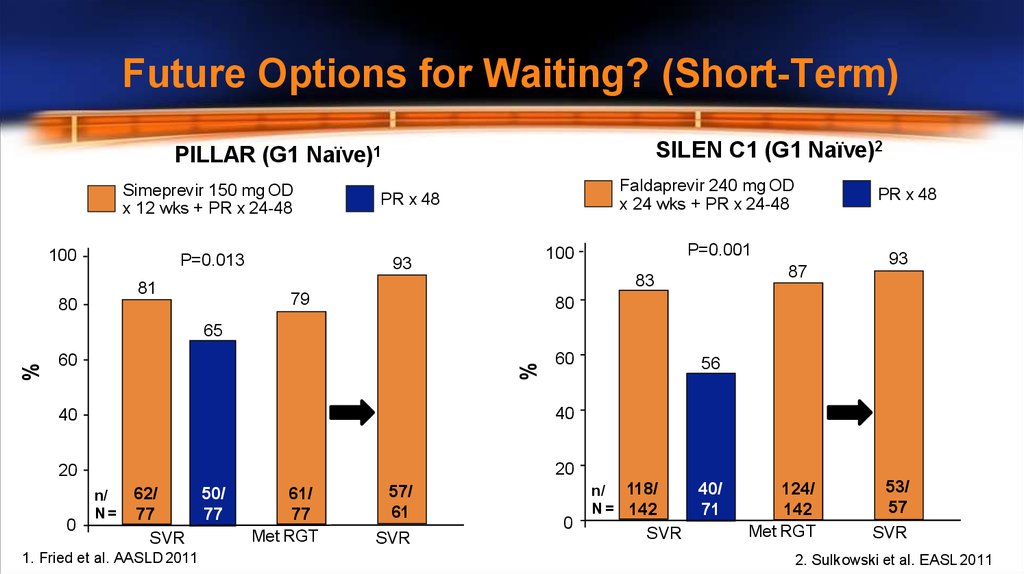
Future Options for Waiting? (Short-Term)SILEN C1 (G1 Naïve)2
PILLAR (G1 Naïve)1
Simeprevir 150 mg OD
x 12 wks + PR x 24-48
100
P=0.013
Faldaprevir 240 mg OD
x 24 wks + PR x 24-48
PR x 48
P=0.001
100
93
87
83
81
79
80
PR x 48
93
80
60
%
%
65
60
40
40
20
20
0
n/
N=
62/
50/
77
77
SVR
1. Fried et al. AASLD 2011
61/
77
Met RGT
57/
61
SVR
0
56
n/ 118/
N = 142
SVR
40/
71
124/
142
Met RGT
53/
57
SVR
2. Sulkowski et al. EASL 2011
23.
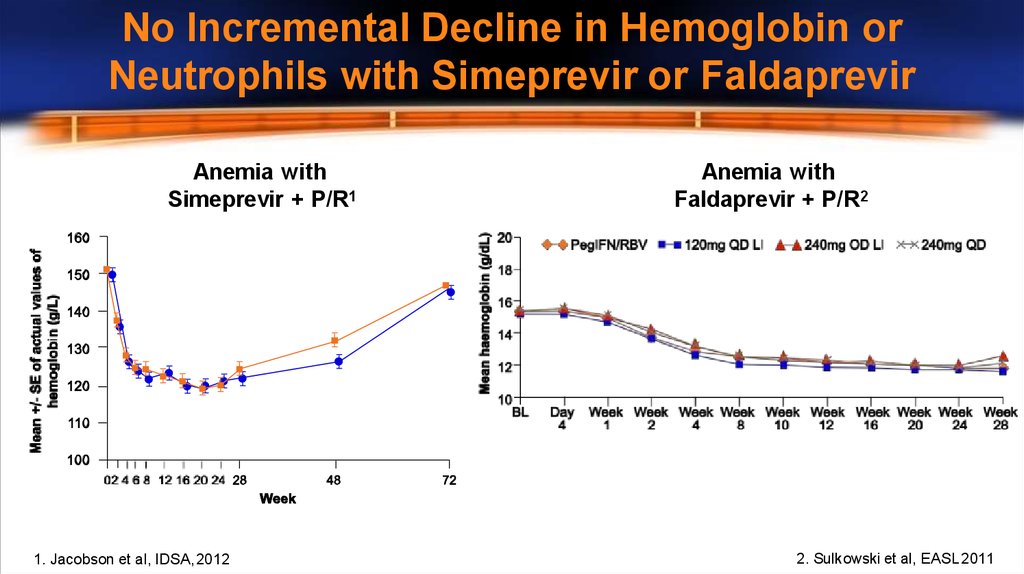
No Incremental Decline in Hemoglobin orNeutrophils with Simeprevir or Faldaprevir
Anemia with
Simeprevir + P/R1
1. Jacobson et al, IDSA, 2012
Anemia with
Faldaprevir + P/R2
2. Sulkowski et al, EASL 2011
24.
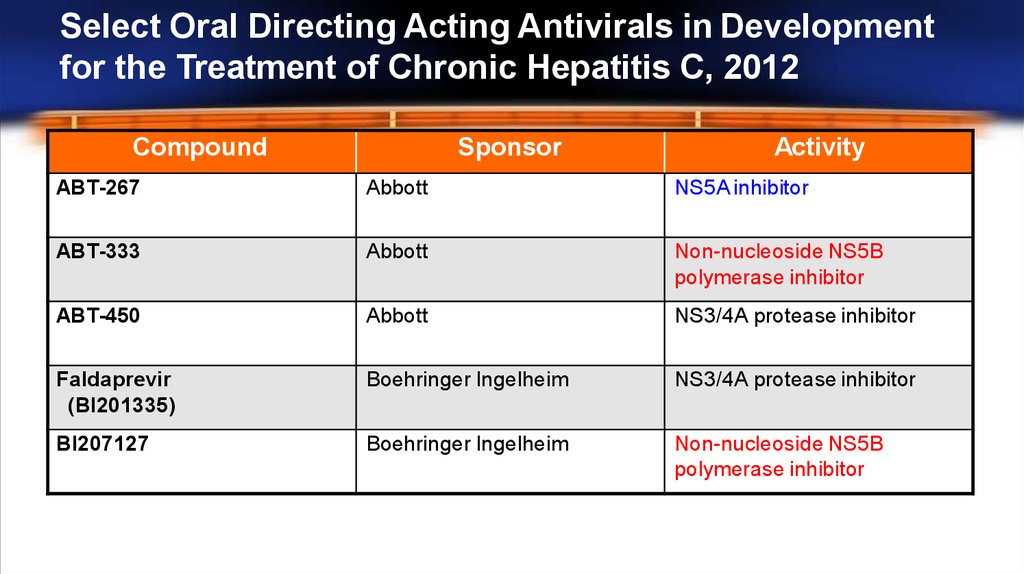
Select Oral Directing Acting Antivirals in Developmentfor the Treatment of Chronic Hepatitis C, 2012
Compound
Sponsor
Activity
ABT-267
Abbott
NS5A inhibitor
ABT-333
Abbott
Non-nucleoside NS5B
polymerase inhibitor
ABT-450
Abbott
NS3/4A protease inhibitor
Faldaprevir
(BI201335)
Boehringer Ingelheim
NS3/4A protease inhibitor
BI207127
Boehringer Ingelheim
Non-nucleoside NS5B
polymerase inhibitor
25.
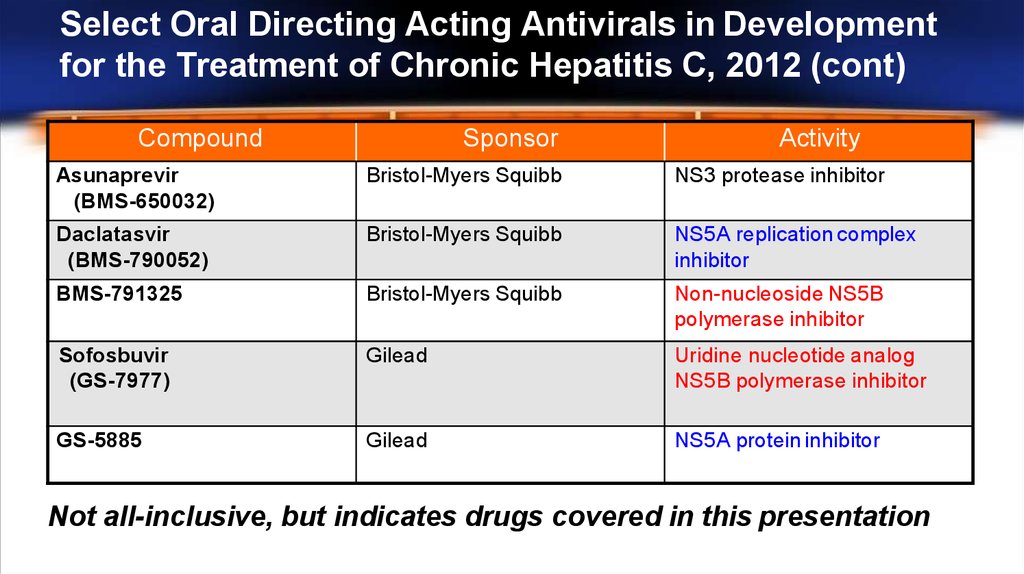
Select Oral Directing Acting Antivirals in Developmentfor the Treatment of Chronic Hepatitis C, 2012 (cont)
Compound
Sponsor
Activity
Asunaprevir
(BMS-650032)
Bristol-Myers Squibb
NS3 protease inhibitor
Daclatasvir
(BMS-790052)
Bristol-Myers Squibb
NS5A replication complex
inhibitor
BMS-791325
Bristol-Myers Squibb
Non-nucleoside NS5B
polymerase inhibitor
Sofosbuvir
(GS-7977)
Gilead
Uridine nucleotide analog
NS5B polymerase inhibitor
GS-5885
Gilead
NS5A protein inhibitor
Not all-inclusive, but indicates drugs covered in this presentation
26.
Should Glenn Delay Treatment?• IL28B CC ~80% chance of shortened therapy
- 80-90% chance of SVR
• F3 disease – risk of progression with waiting
• No clear issues with IFN
• Seems anxious and willing to be treated now
• I would suggest treatment
27.
Glenn: On Treatment Response• Glenn was started on TVR/PEG/RBV
• TW4 and TW12
– HCV RNA undetectable
28.
Clinical Decision 2• Which regimen should Glenn receive?
1. 12 weeks TVR/PEG/RBV
2. 12 weeks TVR/PEG/RBV + 12 weeks PEG/RBV
3. 12 weeks TVR/PEG/RBV + 24 weeks PEG/RBV
4. 12 weeks TVR/PEG/RBV + 36 weeks PEG/RBV
5. 24 weeks TVR/PEG/RBV
29.
Recommended Treatment DurationTreatment-Naïve and Prior Relapse Patients
Triple Therapy
TVR/Peg-IFN/RBV
Dual Therapy
Peg-IFN/RBV
Total
Treatment
Duration
Undetectable at TW4 and
TW12
First 12 weeks
Additional 12 weeks
24 weeks
Detectable (<1000 IU/mL)
at TW4 and/or TW12
First 12 weeks
Additional 36 weeks
48 weeks
HCV-RNA
Telaprevir (INCIVEK™) Prescribing Information. Vertex Pharmaceuticals Incorporated, Cambridge, MA. October, 2012.
30.
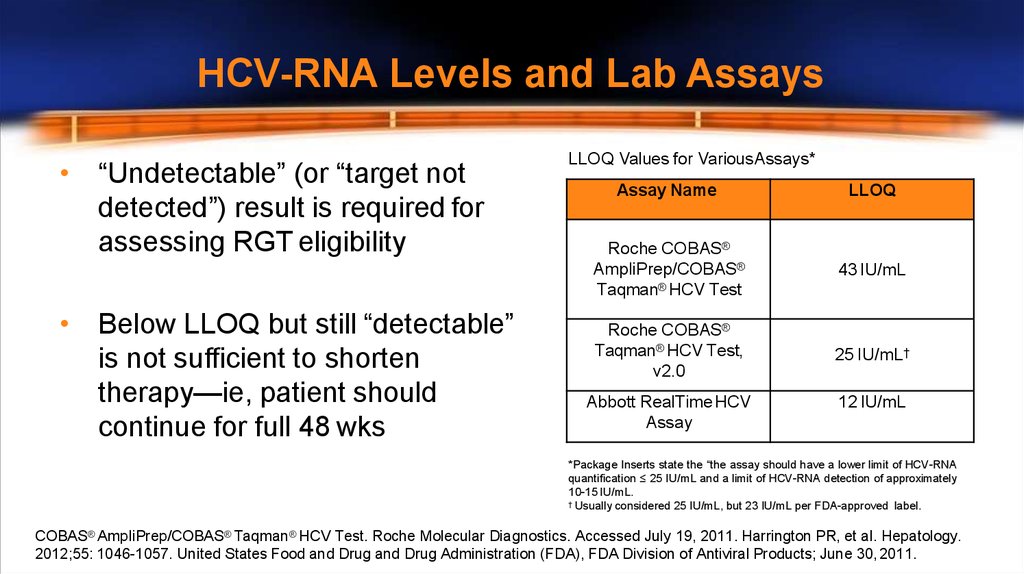
HCV-RNA Levels and Lab Assays• “Undetectable” (or “target not
detected”) result is required for
assessing RGT eligibility
• Below LLOQ but still “detectable”
is not sufficient to shorten
therapy—ie, patient should
continue for full 48 wks
LLOQ Values for VariousAssays*
Assay Name
LLOQ
Roche COBAS®
AmpliPrep/COBAS®
Taqman® HCV Test
43 IU/mL
Roche COBAS®
Taqman® HCV Test,
v2.0
25 IU/mL†
Abbott RealTime HCV
Assay
12 IU/mL
*Package Inserts state the “the assay should have a lower limit of HCV-RNA
quantification ≤ 25 IU/mL and a limit of HCV-RNA detection of approximately
10-15 IU/mL.
† Usually considered 25 IU/mL, but 23 IU/mL per FDA-approved label.
COBAS® AmpliPrep/COBAS® Taqman® HCV Test. Roche Molecular Diagnostics. Accessed July 19, 2011. Harrington PR, et al. Hepatology.
2012;55: 1046-1057. United States Food and Drug and Drug Administration (FDA), FDA Division of Antiviral Products; June 30, 2011.
31.
Conclusions• Many chronic hepatitis C patients are good candidates
for treatment today
• The HCV pipeline is promising with potential new
treatment modalities in the near future
• Physicians should carefully consider individual patient
characteristics when deciding whether to initiate or delay
treatment




 medicine
medicine








