Similar presentations:
Clostridium perfringens
1.
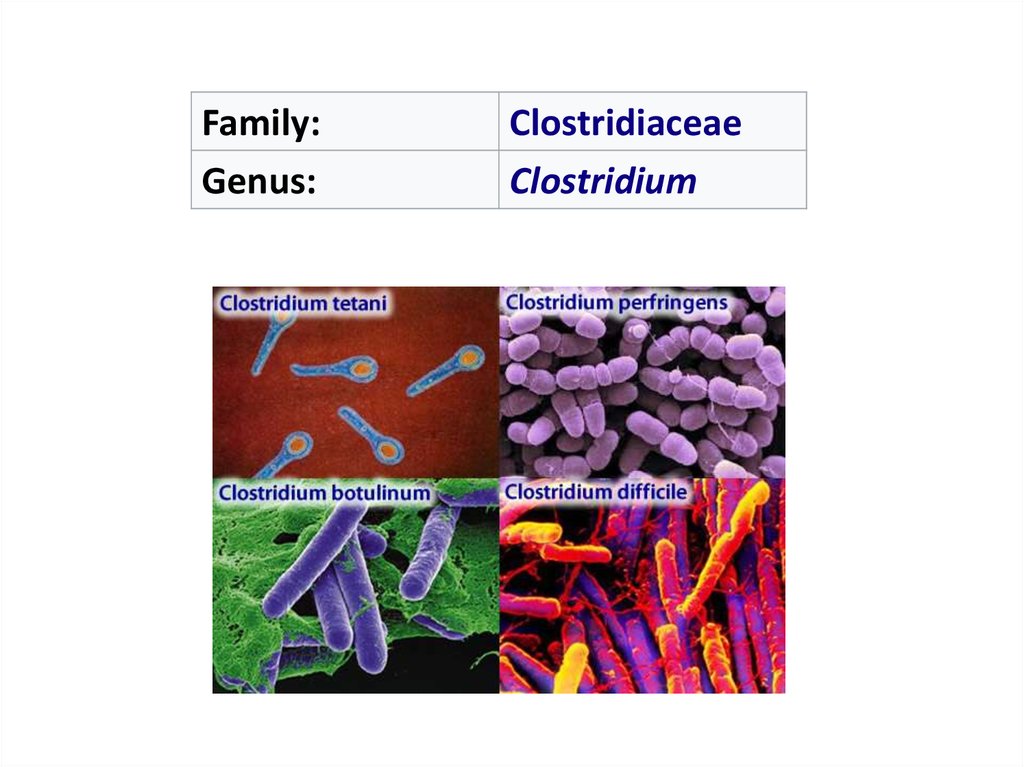
Family:Genus:
Clostridiaceae
Clostridium
2. Clostridium perfringens
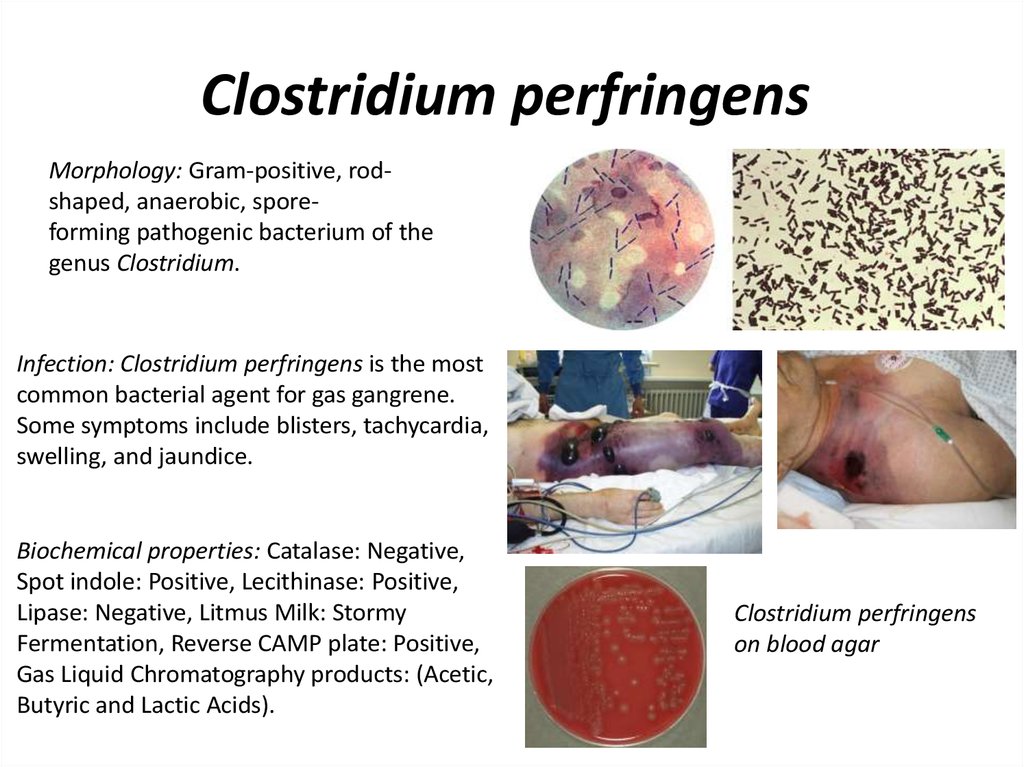
Clostridium perfringensMorphology: Gram-positive, rodshaped, anaerobic, sporeforming pathogenic bacterium of the
genus Clostridium.
Infection: Clostridium perfringens is the most
common bacterial agent for gas gangrene.
Some symptoms include blisters, tachycardia,
swelling, and jaundice.
Biochemical properties: Catalase: Negative,
Spot indole: Positive, Lecithinase: Positive,
Lipase: Negative, Litmus Milk: Stormy
Fermentation, Reverse CAMP plate: Positive,
Gas Liquid Chromatography products: (Acetic,
Butyric and Lactic Acids).
Clostridium perfringens
on blood agar
3. Toxins and enzymes
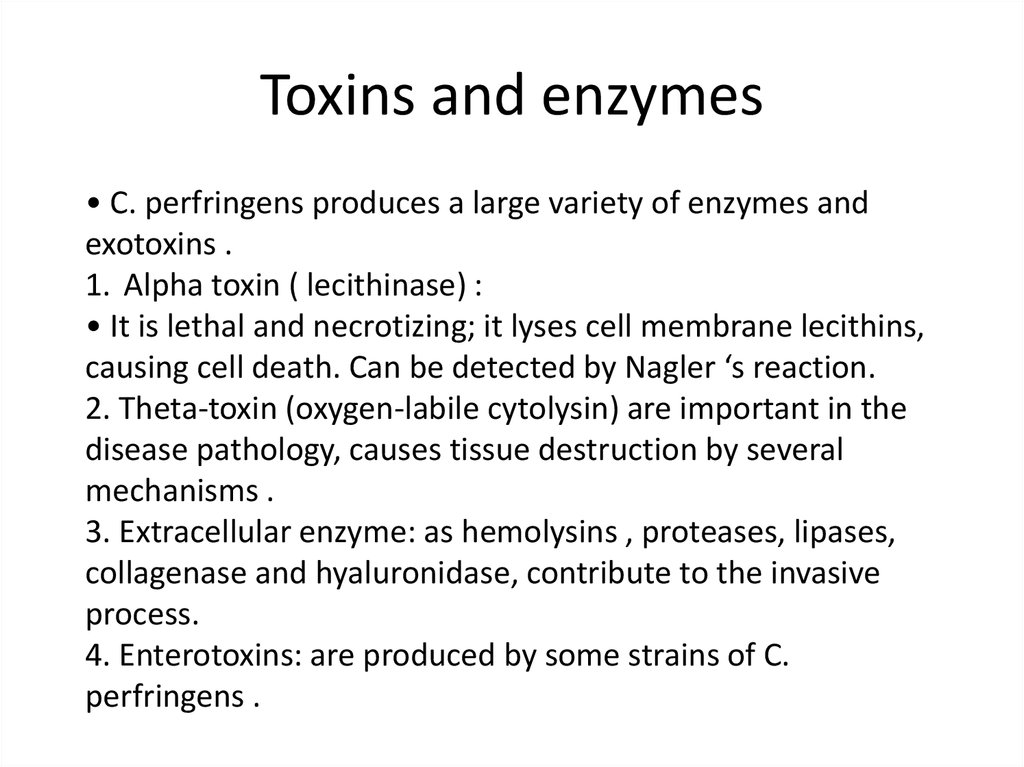
• C. perfringens produces a large variety of enzymes andexotoxins .
1. Alpha toxin ( lecithinase) :
• It is lethal and necrotizing; it lyses cell membrane lecithins,
causing cell death. Can be detected by Nagler ‘s reaction.
2. Theta-toxin (oxygen-labile cytolysin) are important in the
disease pathology, causes tissue destruction by several
mechanisms .
3. Extracellular enzyme: as hemolysins , proteases, lipases,
collagenase and hyaluronidase, contribute to the invasive
process.
4. Enterotoxins: are produced by some strains of C.
perfringens .
4. Gas gangrene
Myonecrosis is a conditionof necrotic damage, specific
to muscle tissue. It is often seen
in
infections
with
C.
perfringens or any of myriad
soil-borne anaerobic bacteria.
Bacteria cause myonecrosis by
specific
exotoxins.
These microorganisms are
opportunistic and, in general,
enter the body through
significant
skin
breakage.
Gangrenous infection by soilborne bacteria was common in
the combat injuries of soldiers
well into the 20th century,
because of nonsterile field
surgery and the basic nature of
care for severe projectile
wounds
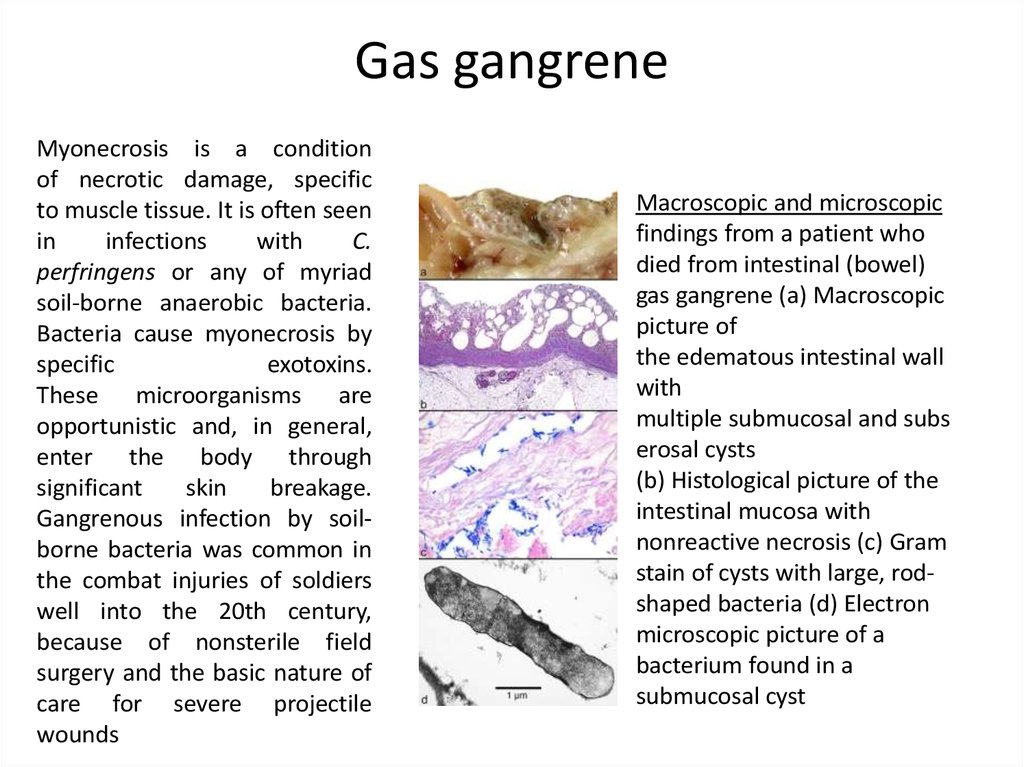
Macroscopic and microscopic
findings from a patient who
died from intestinal (bowel)
gas gangrene (a) Macroscopic
picture of
the edematous intestinal wall
with
multiple submucosal and subs
erosal cysts
(b) Histological picture of the
intestinal mucosa with
nonreactive necrosis (c) Gram
stain of cysts with large, rodshaped bacteria (d) Electron
microscopic picture of a
bacterium found in a
submucosal cyst
5. Diagnosis
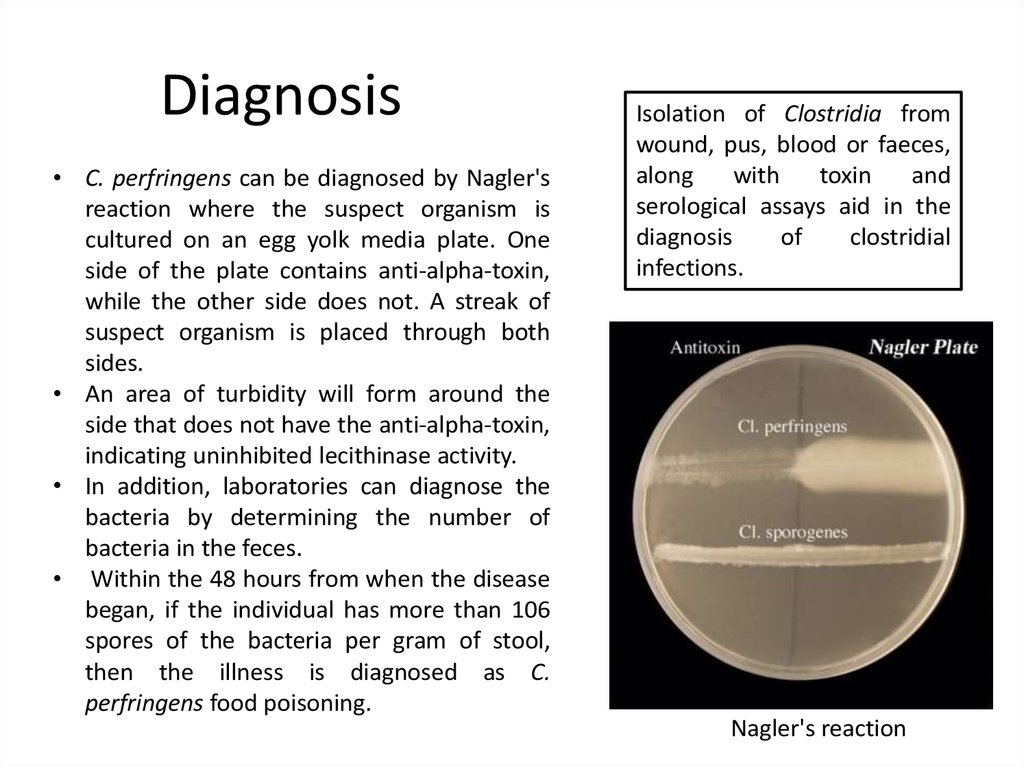
• C. perfringens can be diagnosed by Nagler'sreaction where the suspect organism is
cultured on an egg yolk media plate. One
side of the plate contains anti-alpha-toxin,
while the other side does not. A streak of
suspect organism is placed through both
sides.
• An area of turbidity will form around the
side that does not have the anti-alpha-toxin,
indicating uninhibited lecithinase activity.
• In addition, laboratories can diagnose the
bacteria by determining the number of
bacteria in the feces.
• Within the 48 hours from when the disease
began, if the individual has more than 106
spores of the bacteria per gram of stool,
then the illness is diagnosed as C.
perfringens food poisoning.
Isolation of Clostridia from
wound, pus, blood or faeces,
along
with
toxin
and
serological assays aid in the
diagnosis
of
clostridial
infections.
Nagler's reaction
6. Clostridium tetani
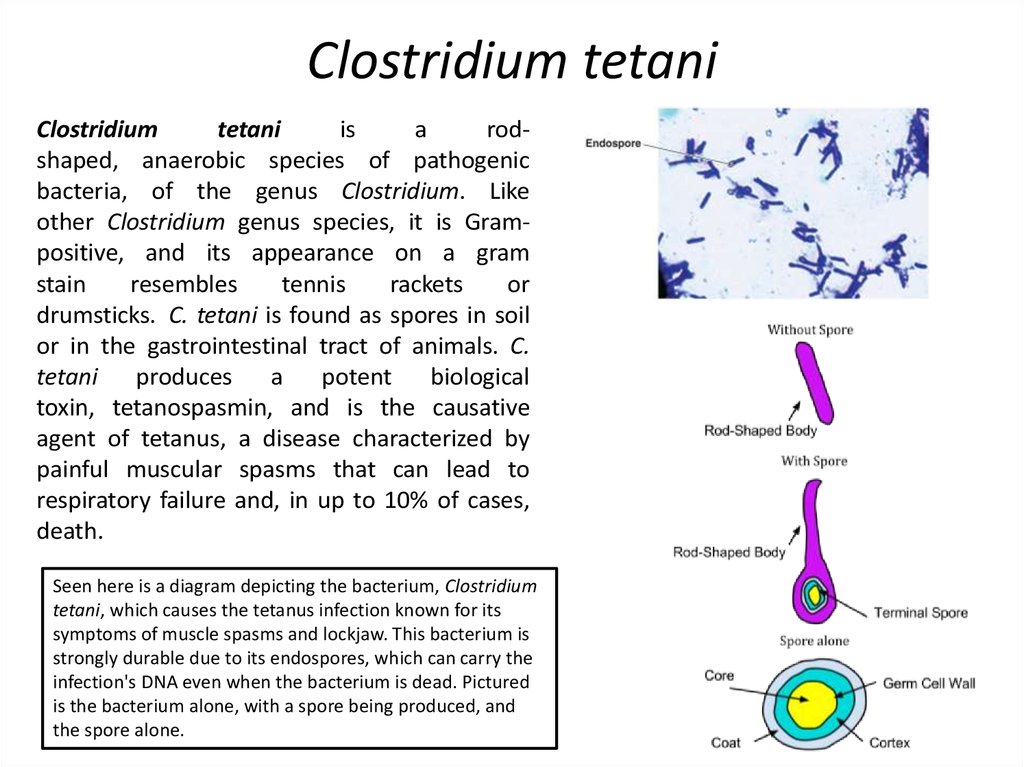
Clostridiumtetani
is
a
rodshaped, anaerobic species of pathogenic
bacteria, of the genus Clostridium. Like
other Clostridium genus species, it is Grampositive, and its appearance on a gram
stain
resembles
tennis
rackets
or
drumsticks. C. tetani is found as spores in soil
or in the gastrointestinal tract of animals. C.
tetani produces a potent biological
toxin, tetanospasmin, and is the causative
agent of tetanus, a disease characterized by
painful muscular spasms that can lead to
respiratory failure and, in up to 10% of cases,
death.
Seen here is a diagram depicting the bacterium, Clostridium
tetani, which causes the tetanus infection known for its
symptoms of muscle spasms and lockjaw. This bacterium is
strongly durable due to its endospores, which can carry the
infection's DNA even when the bacterium is dead. Pictured
is the bacterium alone, with a spore being produced, and
the spore alone.
7. C. tetani produces two toxins
a.Tetanolysin:• A hemolysin that has no role in Pathogenesis .
b.Tetanospasmin:
• A neurotoxin responsible for the symptoms of tetanus
• All C. tetani strains produce a toxin with identical
immunological and pharmacological properties .
• The toxin is heat labile, destroyed at 56 °C in 5 minutes,
and is oxygen labile .
• The toxin rapidly converts to toxoid in the presence of
formalin .
• Toxin action : It blocks the release of inhibitory
neurotransmitters, so it produces the generalized muscular
spasms characteristic of tetanus.
8. Tetanus
Tetanus, also known as lockjaw, isan infection characterized by muscle
spasms. In the most common type, the spasms
begin in the jaw and then progress to the rest
of the body. These spasms usually last a few
minutes each time and occur frequently for
three to four weeks. Spasms may be so severe
that bone fractures may occur.
Other
symptoms
may
include fever, sweating, headache, trouble
swallowing, high blood pressure, and a fast
heart rate. Onset of symptoms is typically
three to twenty-one days following infection. It
may take months to recover. About 10% of
those infected die.
9. Vaccination
Tetanus can be prevented through the highly effective tetanus vaccine, which isa tetanus toxin inactivated with formaldehyde to be immunogenic but
not pathogenic. The vaccine can be formulated as simple or adsorbed tetanus
vaccine, combined tetanus and killed polio vaccine, or the older (diphtheria,
tetanus, pertussis) (DPT) vaccine. Side effects are rare, but if they do occur,
include fever, pain (sometimes long lasting) at the injection site, unexplained
crying in infants, and irritability in older children or adults. Severe reactions are
extremely rare and include anaphylaxis, seizures and encephalopathy. All
infants are recommended to receive the vaccine at 2, 4, 6, and 15 months of
age . A fifth booster dose should be given at 4–6 years of age. After that, it
should be given every 10 years. However, if a bite, scratch, or puncture occurs
more than five years after the last dose of vaccine, the patients should receive
another dose of vaccine.
10. Diagnostics
• Anaerobic culture of tissues from wounds: cultureon blood agar at 37°C.
• C tetani produces colonies with complete
haemolysis on blood agar and swarming • Has
terminal spherical spores
• Produces indole, but does not produce acid from
glucose.
• Isolation of C.tetani must be confirmed by
production of toxin and its neutralization by specific
antitoxin
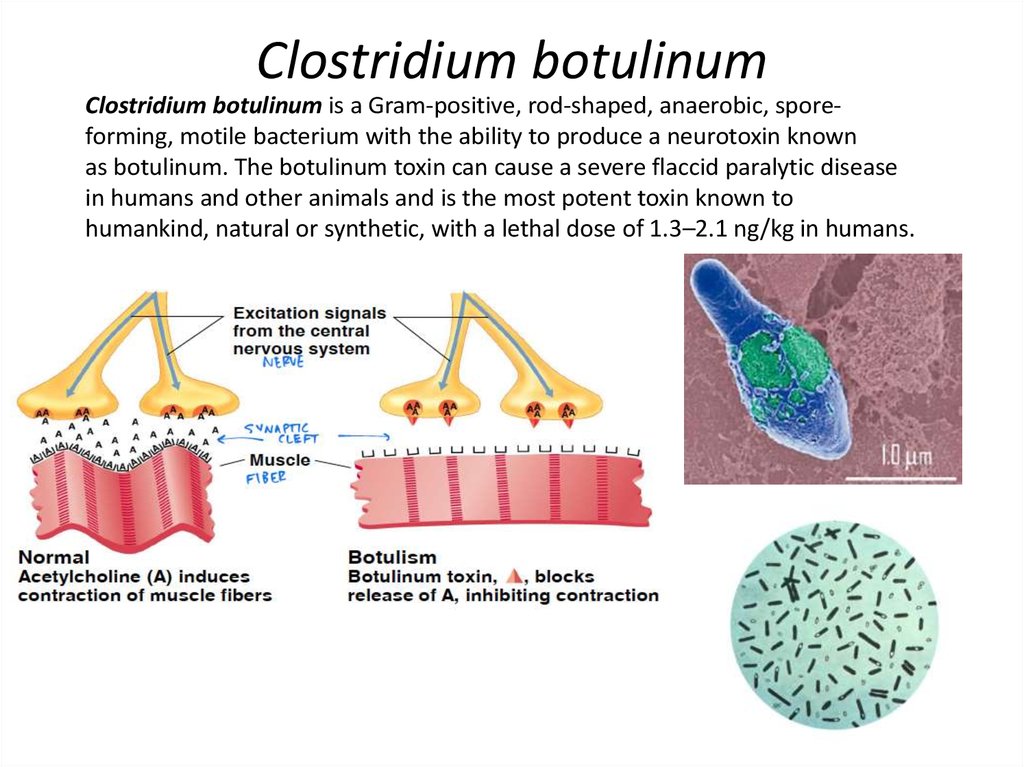
11. Clostridium botulinum
Clostridium botulinum is a Gram-positive, rod-shaped, anaerobic, sporeforming, motile bacterium with the ability to produce a neurotoxin knownas botulinum. The botulinum toxin can cause a severe flaccid paralytic disease
in humans and other animals and is the most potent toxin known to
humankind, natural or synthetic, with a lethal dose of 1.3–2.1 ng/kg in humans.
12. Botultoxin
Seven antigenic types of toxins exist .• The toxins are designated A, B, C1, D, E,
F, and G) .
• Types A, B, E and F are the most toxic for
humans.
• Type A is the most potent exotoxin
known (10 ng can kill a normal adult).
• Toxin is heat-labile
• Toxin binds to neuromuscular junctions of
parasympathetic nerves and interferes with
acetylcholine release, causing flaccid muscle
paralysis.
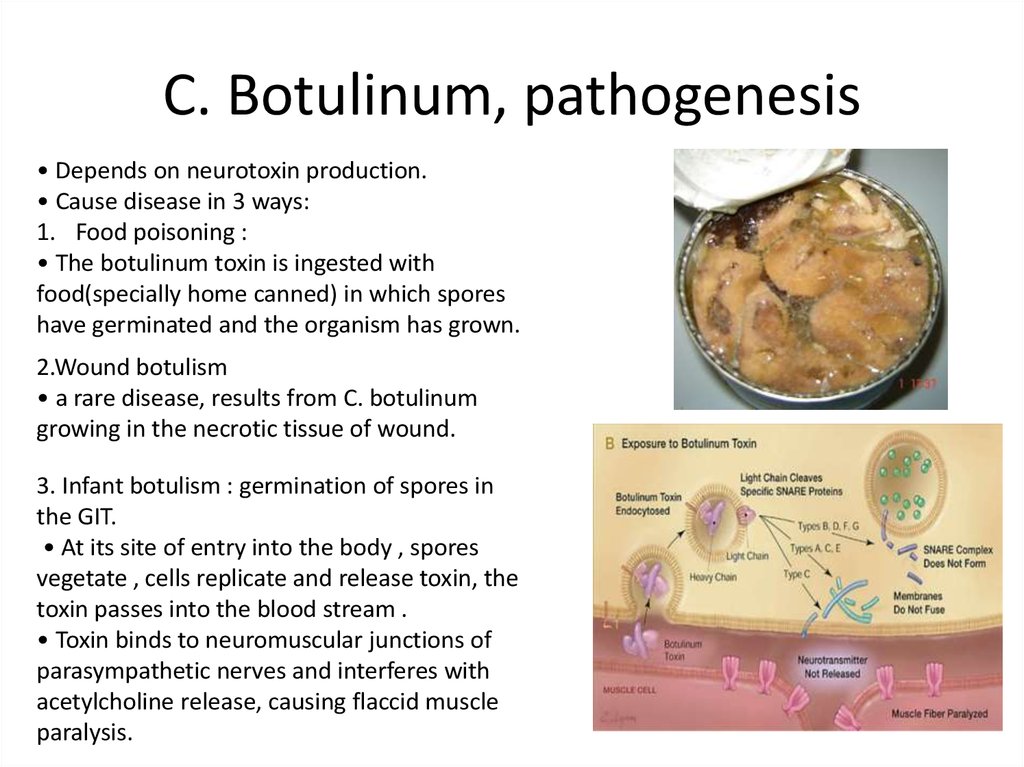
13. C. Botulinum, pathogenesis
• Depends on neurotoxin production.• Cause disease in 3 ways:
1. Food poisoning :
• The botulinum toxin is ingested with
food(specially home canned) in which spores
have germinated and the organism has grown.
2.Wound botulism
• a rare disease, results from C. botulinum
growing in the necrotic tissue of wound.
3. Infant botulism : germination of spores in
the GIT.
• At its site of entry into the body , spores
vegetate , cells replicate and release toxin, the
toxin passes into the blood stream .
• Toxin binds to neuromuscular junctions of
parasympathetic nerves and interferes with
acetylcholine release, causing flaccid muscle
paralysis.
14. C. Botulinum, prevention
Proper food handling and preparation.• Boiling of contaminated food will inactivate the
toxin, as it is heat-labile .
• Food containers that bulge may contain gas
produced by C. botulinum and should not be
opened or tasted.
• A multivalent toxoid produces good protective
antibiody response
• Its use is unjustified due to the infrequency of the
disease.
15. C. Botulinum, diagnosis
Demonstrating toxin in the patient's feces, serum, orvomitus.
• Fecal samples are the best specimens for
detecting toxin in food poisoning or infant botulism .
• Toxin is usually detected by its lethal effect in mice
coupled with neutralization of this effect by specific
antisera.
16. ANTIMICROBIAL THERAPY
• Clindamycin• Penicillin-G
• Metronidazole
• Vancomycin
• Imipenem
• Meropenem
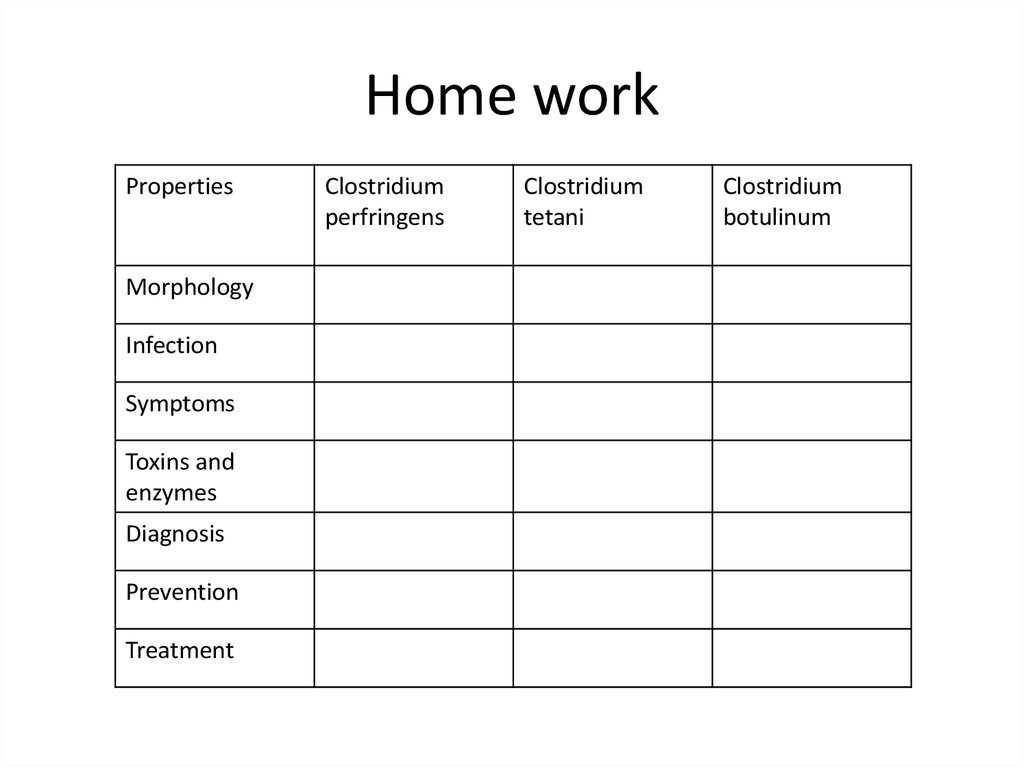
17. Home work
PropertiesMorphology
Infection
Symptoms
Toxins and
enzymes
Diagnosis
Prevention
Treatment
Clostridium
perfringens
Clostridium
tetani
Clostridium
botulinum





 medicine
medicine