Similar presentations:
Anticoagulant, Antiagregant Therapy
1. Anticoagulant, Antiagregant Therapy
Dr Inna TzoranThrombosis and Hemostasis Unit
Rambam Madical Center
2. Overview
• Indications• Heparin/heparin like drugs and their
complications
• Warfarin
• New anticoagulant drugs
3. Indications of Anticoagulant Therapy
• Treatment and Prevention of Deep VenousThrombosis
• Pulmonary Emboli
• Prevention of stroke in patients with atrial
fibrillation, artificial heart valves, cardiac
thrombus.
• Ischaemic heart disease
• During procedures such as cardiac
catheterisation
4. Standard Heparin
• Heterogenous mixture of polysaccharidechains
• MW 3k to 30k
• Active in vitro and in vivo
• Administration - parenteral- Do not inject IM only IV or deep s.c.
• Half-life 1 - 2 hrs - monitor APTT
• Adverse effect - haemorrhage - antidote protamine sulphate
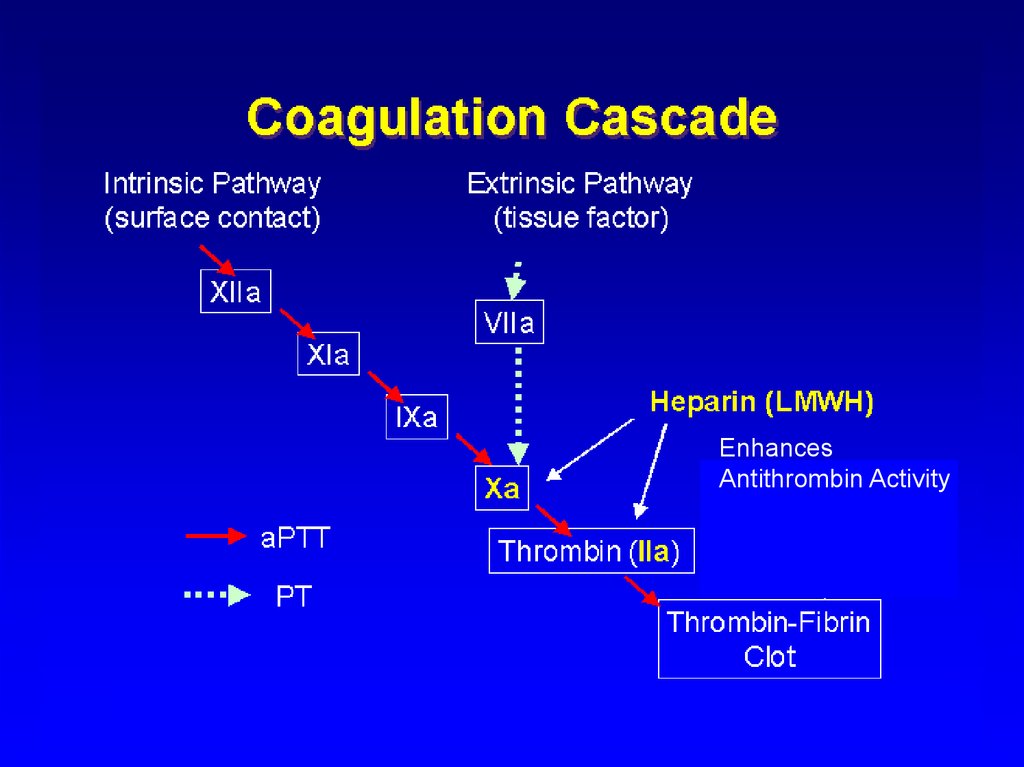
5.
EnhancesAntithrombin Activity
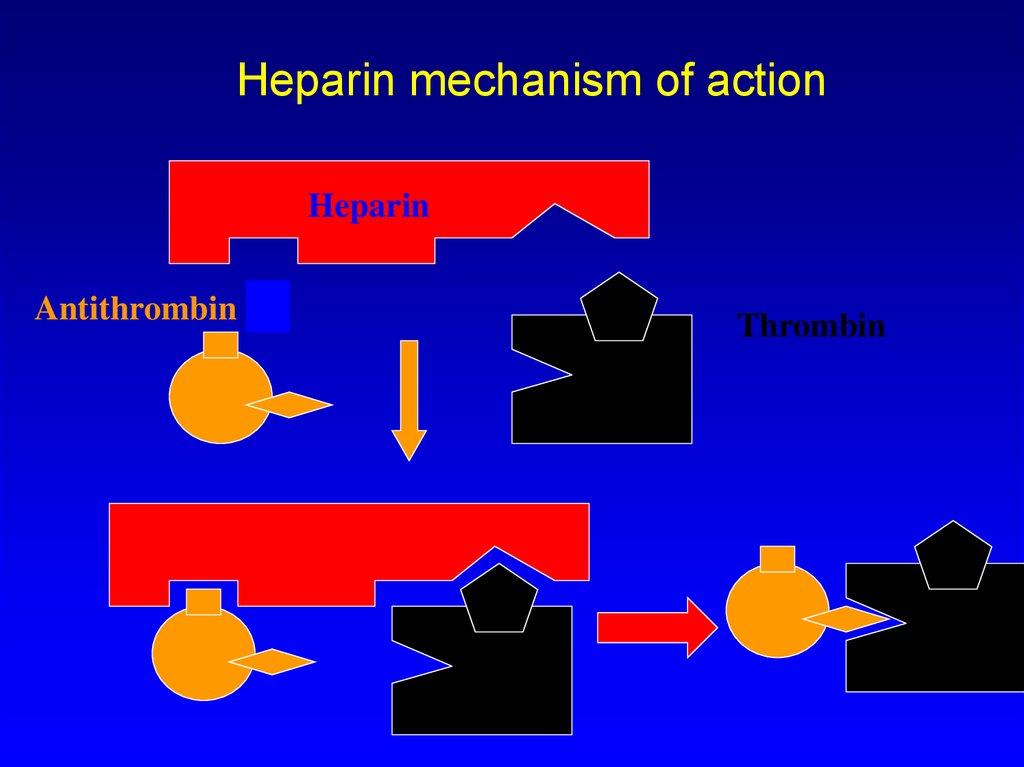
6. Heparin mechanism of action
HeparinAntithrombin III
Thrombin
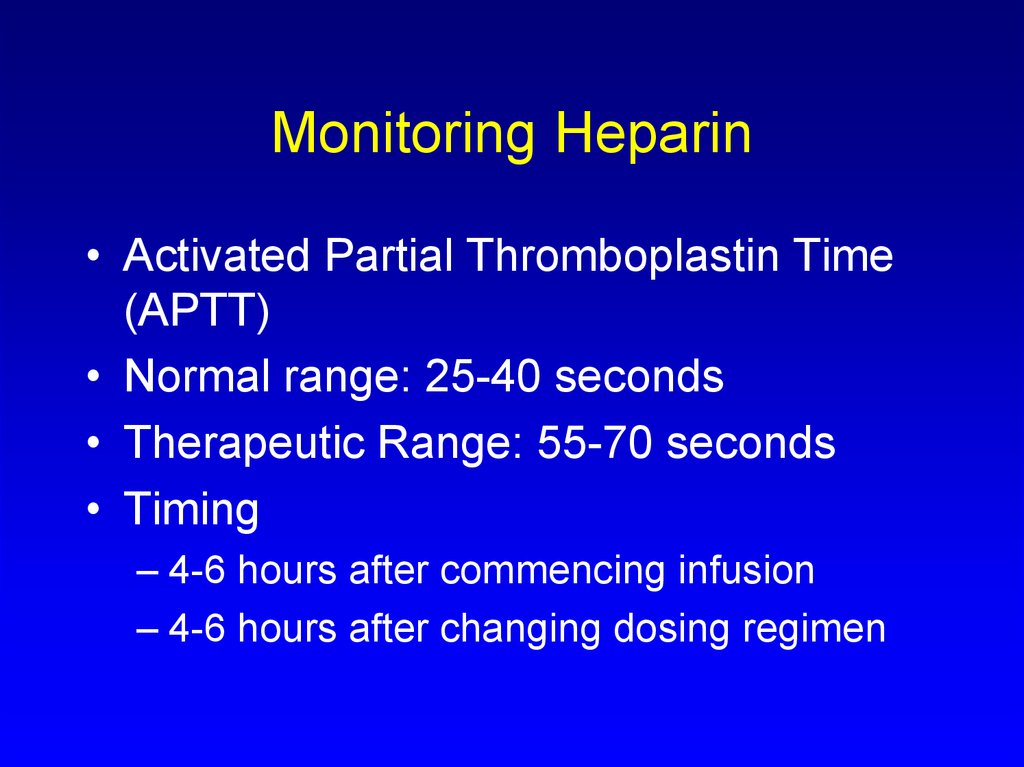
7. Monitoring Heparin
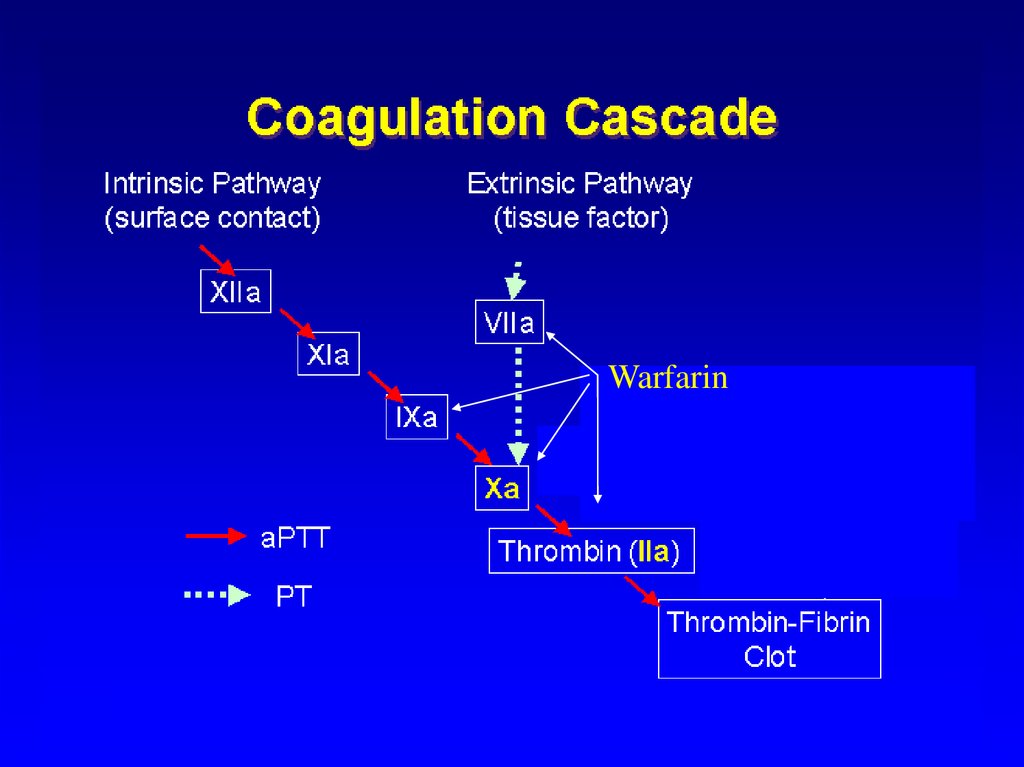
• Activated Partial Thromboplastin Time(APTT)
• Normal range: 25-40 seconds
• Therapeutic Range: 55-70 seconds
• Timing
– 4-6 hours after commencing infusion
– 4-6 hours after changing dosing regimen
8. Low Molecular Weight Heparin
• Changed management of venousthromboembolism
• Standard (Unfractionated) heparin 3k to
30k
• LMWH contains polysaccharide chains
MW 5k
• Enriched with short chains with higher
anti-Xa:IIa ratio
9.
10.
11.
12.
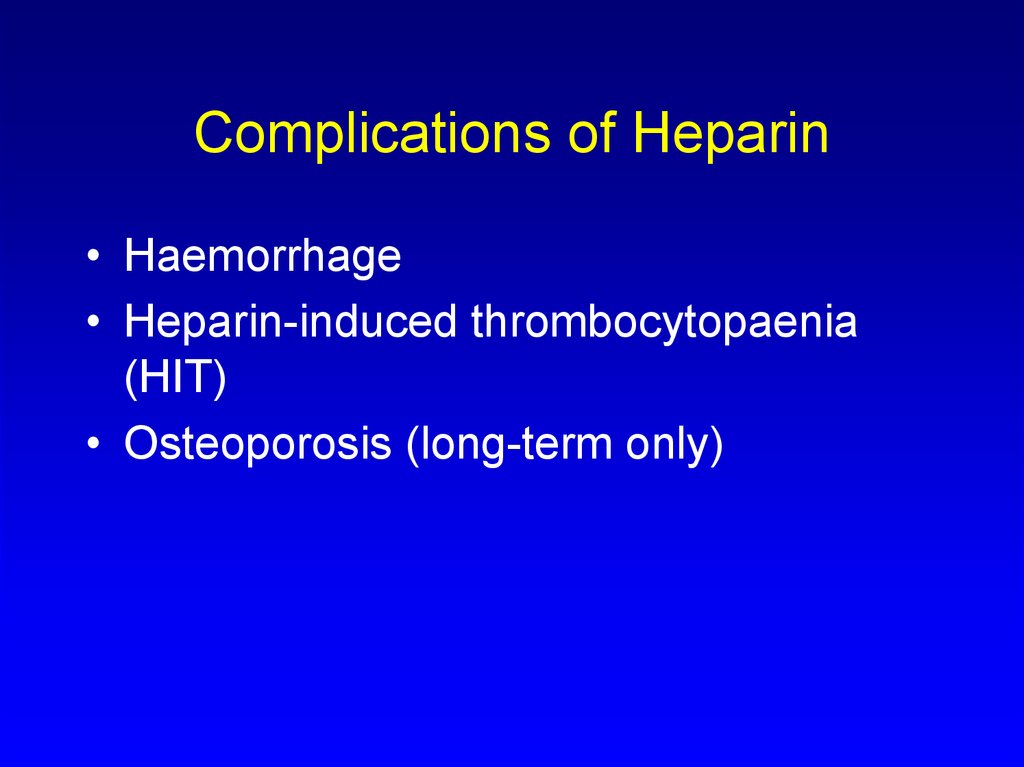
13. Complications of Heparin
• Haemorrhage• Heparin-induced thrombocytopaenia
(HIT)
• Osteoporosis (long-term only)
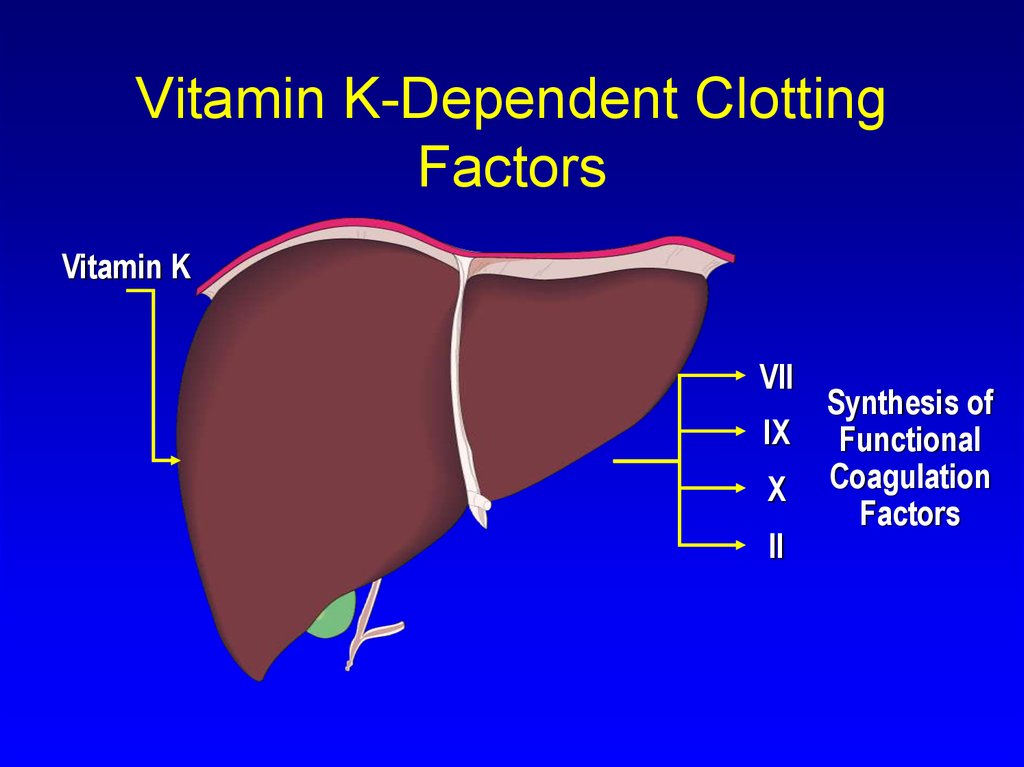
14. Vitamin K-Dependent Clotting Factors
Vitamin KVII
IX
X
II
Synthesis of
Functional
Coagulation
Factors
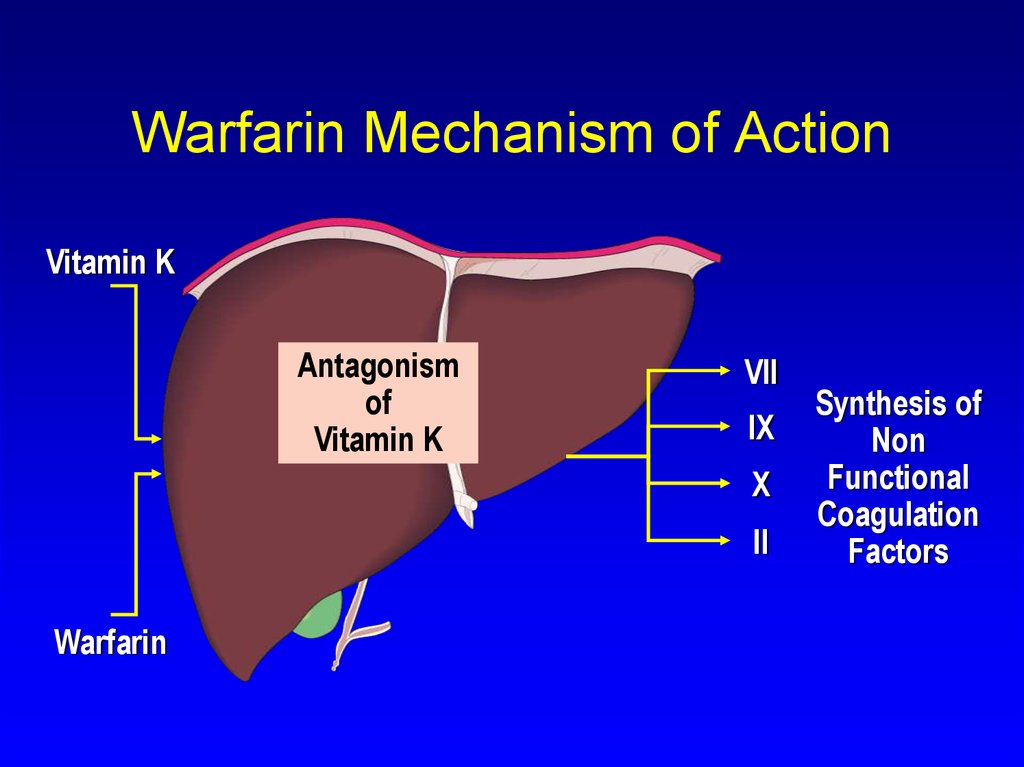
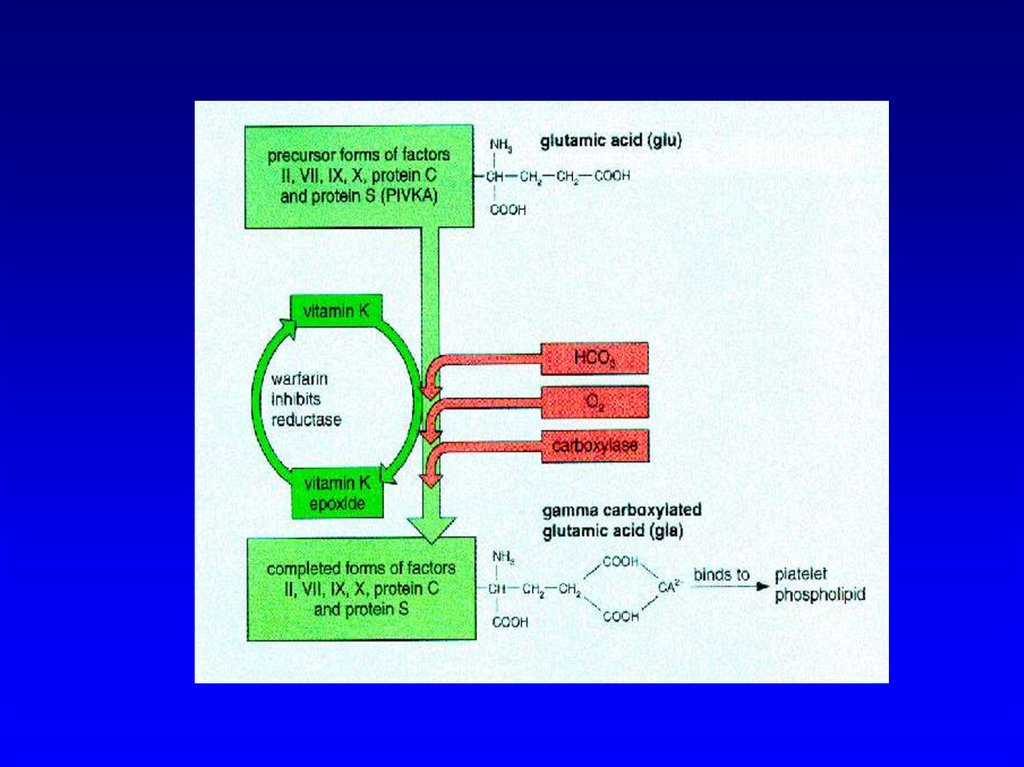
15. Warfarin Mechanism of Action
Vitamin KAntagonism
of
Vitamin K
VII
IX
X
II
Warfarin
Synthesis of
Non
Functional
Coagulation
Factors
16.
17.
WarfarinEnhances
Antithrombin Activity
18. Warfarin: Major Adverse Effect—Haemorrhage
Warfarin: Major Adverse Effect—Haemorrhage
• Factors that may influence bleeding
risk:
– Intensity of anticoagulation
– Concomitant clinical disorders
– Concomitant use of other medications
– Quality of management
19. Warfarin-induced Skin Necrosis
20. Prothrombin Time (PT)
Prothrombin Time (PT)• Historically, a most reliable and “relied upon”
clinical test
However:
– Proliferation of thromboplastin reagents
with widely varying sensitivities to reduced
levels of vitamin K-dependent clotting
factors has occurred
– Problem addressed by use of INR
(International Normalised Ratio)
21. Changing over from Heparin to Warfarin
• May begin concomitantly with heparin therapy• Heparin should be continued until target INR
for two days
• When INR reaches desired therapeutic range,
discontinue heparin
22. Warfarin: Dosing & Monitoring
Warfarin: Dosing & Monitoring• Start low
– Initiate 5 mg daily
– Educate patient
• Stabilise
– Titrate to appropriate INR
– Monitor INR frequently (daily then weekly)
• Adjust as necessary
• Monitor INR regularly (every 1–2 weeks) and adjust
23. Relative Contraindications to Warfarin Therapy
• Situations where the risk of hemorrhageis greater than the potential clinical
benefits of therapy
– Uncontrolled alcohol/drug abuse
– Unsupervised dementia/psychosis
24. Reversing action of warfarin
• Plasma– Rapid but short-lasting
• Vitamin K
– Not rapid, but lasts 1-2 weeks. Do not use
if wishing to restart warfarin within next
week.
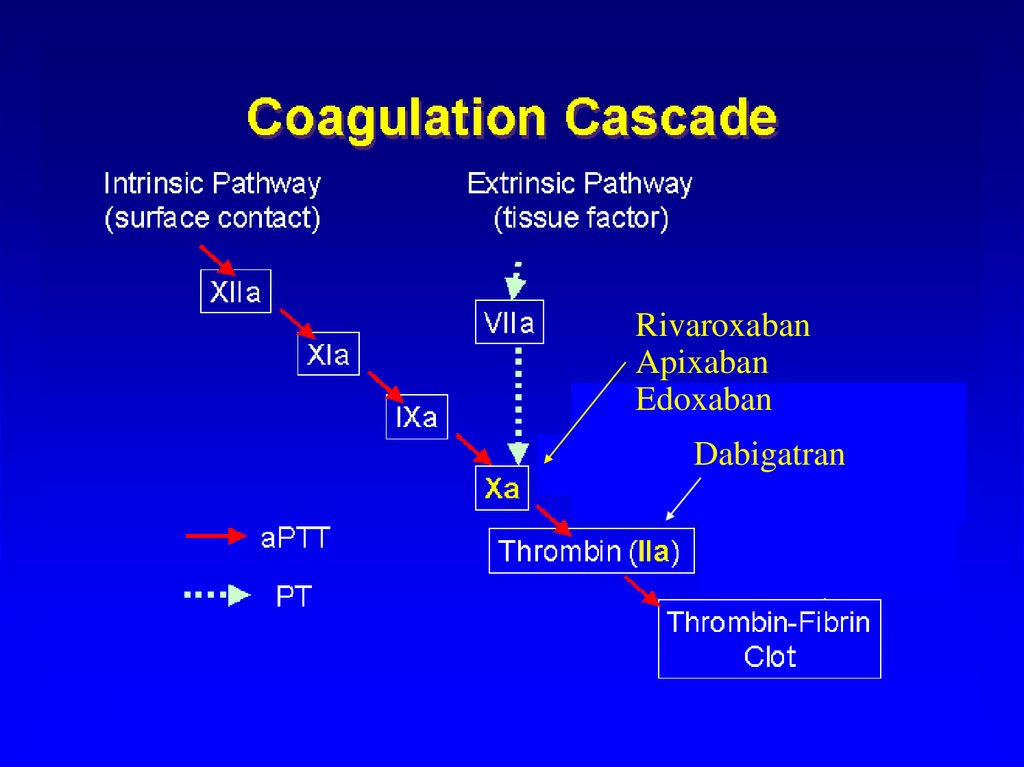
25. New Anticoagulation Drugs
• Direct Thrombin Inhibitors– PO: Dabigatran
– IV: hirudin, bivalirudin, and argatroban
Synthetic pentasaccharide
Acivated Protein C
Tissue Factor Pathway Inhibitor (TFPI)
Factor Xa inhibitor PO: rivaroxaban,
apixaban, edoxaban
26. Synthetic Pentasaccharide
E.g Fondaparinux (Arixtra®)
Synthetic, single molecular entity
Targets Factor Xa
Does not cause thrombocytopenia
Shown DVT prevention during
orthopedic procedures.
• Better than LMWH in ischaemic heart
disease
27. Dabigatran (Pradaxa®)
Two doses available.
Twice daily treatment.
No monitoring needed.
Recent studies showed it as good as or
even superior to warfarin in atrial
fibrillation and VTE treatment.
28. Rivaroxaban (Xarelto®); Apixaban (Eliquis®)
• Once/ twice daily• No dose monitoring needed.
• As good as warfarin in efficacy and
superior on safety in AF and VTE
treatment
29.
RivaroxabanApixaban
Edoxaban
Enhances
Dabigatran
Antithrombin Activity
30. Antiagregants
IndicationsIschemic
heart disease primary
secondary prevention
CVA
PVD
Atrial fibrilation to avoid CVA
and
31. Aspirin
COX-2 inhibitorside effects:
gastritis, gastric ulcer
Allergy
Thrombocytopenia
32. Clopidrogel (Plavix®)
AD receptor inhibitorSide effects:
Bleeding
Thrombocytopenia
allergy
33. New antiplatelet agents
AD receptor inhibitor:• Prasugrel
• Ticagrelor
• Elinogrel






 medicine
medicine