Similar presentations:
Learning objectives
1.
G. I.T. BleedingDR K . M. S. SULIMAN
CONSULTANT SURGEON
2.
G. I.T. BleedingLearning objectives
To realize the importance of GI bleeding in clinical practice
To define the different manifestations of GIB
To identify the causes of GIB
To be able to risk stratify cases of GIB
To be able to manage cases of GIB
3.
G. I.T. BleedingGI bleeding is the most common gastrointestinal
emergency
Sites:
50% of admissions for GI bleeding are for upper GIB
(UGIB; from esophagus, stomach, duodenum).
40% are for lower GI (LGIB; from the colon and
anorectum).
10% are for obscure bleeding.
4.
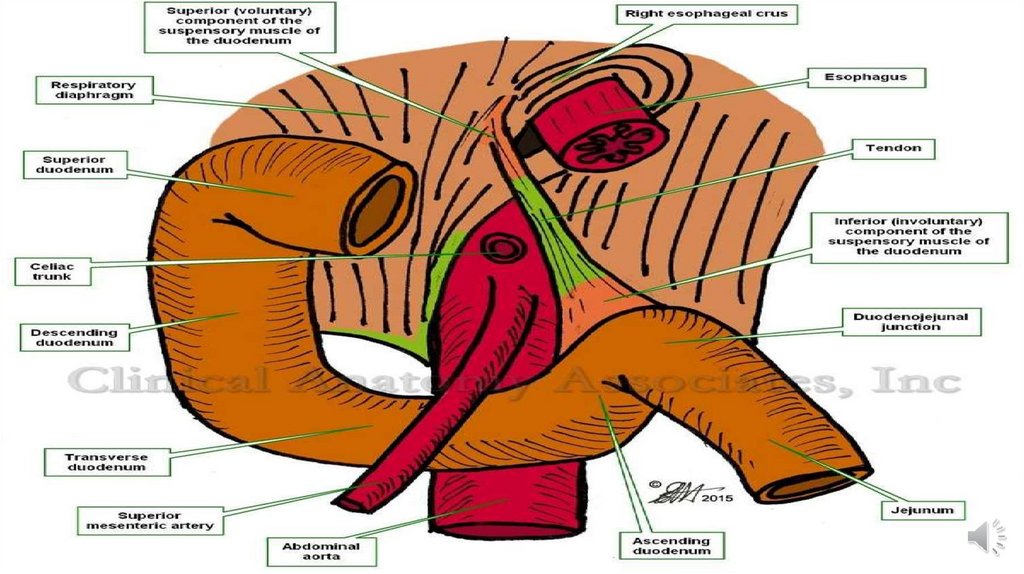
G.I.T. bleeding is Classified into:Upper GI bleeding (proximal to
ligament of Treitz).
Lower GI bleeding (distal to ligament of
Treitz).
Upper GI bleeding 4x more common
than lower GI bleeding and is a major
cause of morbidity and mortality.
5.
G. I.T. Bleeding6.
Upper G.I.T. BleedingUpper gastrointestinal bleeding is defined as bleeding
derived from a source proximal to the ligament of Treitz.
Upper GI bleed remains a major medical problem.
About 75% of patient presenting to the emergency room
with GI bleeding have an upper source.
Bleeding is self-limited in 80% of patients
with UGI hemorrhage, even without specific
therapy.
In-hospital mortality of 5-10% can be expected.
7.
Upper G.I.T. BleedingTHE COMMON CAUSES OF G.I.T. BLEEDING :
1.
Oesophageal Varices ***
2.
Chronic gastritis & gastric erosion **
3.
Peptic ulcer disease**
4.
Mallory Weiss syndrome
5.
Reflux Oesophagitis
6.
Gastric : Adenoma , Polyps , Leiomyoma ,Carcinoma , Lymphoma
7.
Vascular malformation : Angiodysplasia , Telangectasia
8.
Dieulafoy Syndrome.
9.
Miscellaneous : Coagulopathy , Aorto- Enteric fistula , Haemobilia ,
Pancreatitis , Duodenal diverticulum.
8.
Upper G.I.T. BleedingClinical presentation :
1)
Hematemesis.
2)
Melena .
3)
Hematochezia.
4)
Chronic blood loss ( faecal occult blood test =Guiac test ) .
5)
Shock state .
9.
Upper G.I.T. BleedingManagement :
Approach to massive hematemesis management :
90 % stop bleeding on conservative treatment .
Assess A , B , C : Resuscitation + monitoring .
Resuscitation :
1) High flow oxygen .
2 ) 2 large cannula --- start I.V. fluid replacement ( 2 litres of normal saline or Ringer lactate)+ ( 30 – 40
ml per kilogram body weight per day= maintenance fluid ).
3 ) N G tube : monitor bleeding & prevent aspiration.
4 ) Foley's catheter : monitor urine output = > 30 ml per hour.
5 ) Blood tests : CBC , RFT . LFT , Clotting profile , Blood grouping & cross matching.
6 ) Monitoring : conscious state , peripheral perfusion , vital signs , UOP , pulse oxymetry , ABG analysis ,
? CVP ( 5 cm water ).
N.B. Once , the patient is stable , take detailed history + clinical examination & arrange OGD IN THE
NEXT 24 HOURS.
10.
Upper G.I.T. BleedingManagement of stable patient :
Detailed history & Clinical examination .
History of : PU disease , GERD .
History of dyspepsia , anorexia & weight loss ( ? Malignancy )
History of painless hematemesis following violent vomiting or
retching ( Mallory Weiss syndrome )
PMH ( PU disease , GERD , liver disease , schistomiasis ,
coagulopathy , previous UGIT bleeding or operation ).
Drug history ( Aspirin , steroid , NSAIDs , Anticoagulant.
Alcohol abuse : Gastritis & liver cirrhosis
11.
Upper G.I.T. BleedingThe physical signs :
Stigmata of liver disease & Cirrhosis : spider naevi , palmar
erythema , flapping tremors , gynaecomasyia & testicular atrophy.
Stigmata of portal hypertension : oesophageal varices ,
splenomegaly , ascites & caput medusa .
12.
Upper G.I.T. BleedingDiagnosis :
1 ) Oesophago- Gastro - Dudenoscopy ( OGD ) :
A) DIAGNOSTIC :
Site of bleeding ( 80-90 % ).
Biopsy .
Stigmata of risk of bleeding .
B) Therapeutic : to stop or prevent further bleeding
e.g. PU disease , Oesophageal Varices & vascular
malformation.
13.
Upper G.I.T. BleedingENDOSCOPIC TREATMENT of PU DISEASE :
1)
Injection of adrenaline .
2)
Heater or Laser coagulation.
3)
Thermal.
4)
Sutures , clips & stapler.
ENDOSCOPIC TREATMENT of Oesophageal Varices :
1)
Rubber band ligation ( RBL ).
2)
Injection Sclerotherapy.
Factors associated with further bleeding :
a.
Old age.
b.
Shock on admission.
c.
Endoscopic stigmata.
d.
G.U. rather than D.U.
14.
Upper G.I.T. BleedingEndoscopic Stigmata of recent hemorrhage ( increase risk of
Rebleeding ) :
1)
Active bleeding from the ulcer base .
2)
The presence of visible vessel.
3)
Adherent clot overlying the ulcer.
2 ) ANGIOGRAPHY : ( Diagnostic & Therapeutic )
Active bleeding > I ml per minute.
Selective ( catheter in SMA
infusion .
Embolization or Vasopressin
15.
Upper G.I.T. BleedingDiagnostic Endoscopy :
Diagnostic appearance :
Peptic Oesophagitis : Grade:
I.
Linear streaks .
II.
Linear erosions.
III.
Confluent erosions.
IV. Stricture.
Oesophageal Varices :
This is bluish longitudinal columns ( > 4 ) with weavy configuration
& classified ( according to the extent of the bulge into the lumen ) into 4
grades .
1)
16.
Upper G.I. BleedingPeptic ulcer :
Gastric ulcer : round defect in the mucosa ( antrum or along the
lesser curvature ).
Duodenal ulcer :. the first part of the duodenum .
Stigmata of recent bleeding :
1)
Active pulsatile bleeding .
2)
Active non-pulsatile bleeding .
3)
Visible blood vessel.
4)
Flat red or black spot.
17.
Upper G.I.T. BleedingGastritis : multiple shallow ulcers seen in the antrum .
Mallory – Weiss tear : Follow violent vomiting & retching , painless
hematemesis , longitudinal tear usually involve the gastric mucosa >
Oesophageal mucosa at L.O.S.
Dieulafoy lesion: consist of tiny ulcer exposing a large blood vessel
which stick out of the mucosa any where in the stomach.
Gastric tumors : leiomyoma ( central apical ulcer ) , adenoma ,
carcinoma , lymphoma .
Vascular malformation e.g. haemangioma .
Aorto-duodenal fistula in patients with aortic graft , seen in the third
part of the duodenum .
18.
Upper G.I.T. BleedingManagement of Oesophageal Variceal Bleeding :
A.
Medical Treatment :
o
Resuscitation as above with some considerations :
The bleeding is often torrential & clotting abnormalities are common
( send blood for clotting profile , arrange fresh frozen plasma &
platelet concentrations and avoid large volume crystalloid infusion ,
as this will exacerbate ascites and peripheral oedema associated
with portal hypertension & hepatic failure ).
The patient at risk of hepatic coma , the appropriate preventive
measures as follow :
Avoid the use of Opiates.
19.
Upper G.I.T. BleedingThe patient at risk of hepatic coma , the appropriate preventive
measures as follow :
Avoid the use of Opiates.
Reduce the amount of proteins in the gut :
Lactulose 10 ml Q.D.S. & Neomycin 1 g. Q.D.S. , should be given to
reduce the production of toxic metabolites produced by bacterial
flora .
The main pharmacological agents used to control acute Variceal
bleeding are :
A)
Vasopressin .
B)
Somatostatin & its analogues .
20.
Upper G.I.T. BleedingVasopressin ( Splanchnic vasoconstrictor ) : infusion of 0.5 – 0.6 u
/minute , will reduce portal pressure & control acute Variceal
bleeding in 50 - 70 % of cases . ( N.B. Side effects of vasopressin are :
angina & arrhythmias.
SOMATOSTATIN & ITS Analogue ( Octreotide ) :
Octreotide is long acting analogue & selectively acts on the
mesenteric smooth muscles .
Octreotide : 5 ug bolus dose , then Octreotide infusion at rate of 50
ug / hour . ( N.B. Octreotide is very effective in controlling Variceal
bleeding ).
N.B. to reduce the risk of rebreeding , long term administration of
Propranolol ( Inderal 40 mg once daily ).
21.
Upper G.I.T. BleedingB) Balloon temponade : Sengstaken Blackmore tube or one of its variants is used for
control of the acute Variceal bleeding , then , Endoscopic Sclerotherapy is used after
stoppage of the Variceal bleeding .
C ) ENDOSCOPIC THERAPY :
1) Endoscopic Sclerotherapy : Sclerosants e.g. 3% sodium tetradecyl sulphate ( STD ) &
5% Ethanol amine .
2) Rubber band ligation ( RBL ).
D) Oesophageal Surgery for Variceal bleeding :
A.
Oesophageal transection using staple gun .
B.
Porta – Systemic Shunting : Trans - jugular Intra-hepatic porta-systemic shunting (
TIPSS ) : for recurrent bleeding .
22.
Upper G.I.T. BleedingManagement of acute peptic bleeding :
1)
Medical therapy : e.g. H2 receptor antagonist , proton pump
inhibitors , Somatostatin analogues . There is no good evidence that
pharmacological intervention alter the outcome of the upper G.I.
bleeding .
2)
Endoscopic hemostasis :
Endoscopic hemostasis for non-Variceal bleeding , common
techniques :
1) Injection methods : *adrenaline , alcohol , *Sclerosants e.g. 3% STD.
2) Thermal methods : Heater probe , Laser photo-coagulation ,
Diathermy .
3) Topical applications : e.g. collagen , cyano-acrylate glue .
4) Mechanical methods : clips , staples , sutures .
23.
Upper G.I.T. Bleeding3 ) Surgical treatment of acute P.U. bleeding :
The main role of surgery is to obtain secure hemostasis .
Indications for surgery :
1)* Rebleeding after endoscopic treatment .
2) Endoscopic stigmata's for Rebleeding.
3) Hemodynamic instability in spite of adequate resuscitation .
4) Others e.g. comorbid diseases.
Duodenal Ulcer : under running sutures .
Gastric ulcer : partial gastrectomy
24.
Lower G.I. BleedingThe lower G.I. bleeding is defined as bleeding distal to the ligament
of Treitz .
N.B. Hematochezia is a brisk massive bleeding from the upper G.I.T.
The massive blood loss
haemodynamically instability &
therefore , the primary concern to resuscitate the patient , then
identify the source of bleeding .
N.B. In the majority of these patients , the bleeding will stop
spontaneously .
25.
Lower G.I. BleedingCauses :
1)
2)
3)
4)
5)
6)
Upper G.I.T. ( 10% ) : P.U. disease & angiodysplasia .
Small bowel ( 5% ) : Meckel,s diverticulum , lymphoma , jejunal
diverticulosis , Aorto-enteric fistula , trauma .
Colon ( 85% ) : The commonest cause of the bleeding is the colon .
The commonest cause of massive lower G.I. bleeding are Diverticular
disease & angiodysplasia . Other causes : colonic carcinoma ,
colonic polyps , juvenile polyps , ulcerative colitis , ischaemic colitis ,
trauma .
Rectal : carcinoma , rectal prolapse , trauma.
Anal : piles – fissure in ano .
Miscellaneous : mucosal telangiectasia , anti-coagulant ,
coagulopathy , radiation enteritis & colitis , schistomiasis .
26.
Lower G.I. BleedingClinical Features :
o
N.B. while the patient is being resuscitated , obtain thorough history
& clinical examination .
o
Abdominal pain ( IBD & Ischaemic colitis ).
o
Painless P.R. bleeding ( diverticular disease , angiodysplasia , piles ) .
o
Constipation & change in bowel habit ( diverticular disease –
carcinoma ).
o
Anorexia & weight loss ( carcinoma ).
27.
Lower G.I. BleedingClinical examination :
General examination (signs of hypovolemia ).
Abdominal examination : *scars of previous surgery for peptic
ulcer or colonic pathology .
Digital rectal examination : piles , rectal mass .
Proctoscopy & sigmoidoscopy examinations are mandatory after
resuscitation .
Naso-gastric tube should inserted , to check the aspirate for bile ,
fresh or altered blood .
Urethral catheter ( U.O.P. ).
28.
Lower G.I. BleedingInvestigations :
1)
Proctoscopy & Sigmoidoscopy .
2)
Colonoscopy :
Diagnostic accuracy ( 70 – 90 % ).
Therapeutic : identify & arrest bleeding from tumors and
angiodysplasia .
Colonoscopy is contraindicated in shock patient & active lower G.I.
bleeding , due to decrease accuracy of the diagnosis and increase
the risk of perforation .
Since most of the lower G.I. bleeding stop spontaneously , this allow
bowel preparation before colonoscopy .
29.
Lower G.I. Bleeding3 ) Technetium Sulphur colloid scintigraphy :
Diagnosis of slow bleeding rates ( 0.5 ml / minute ).
Technetium Sulphur colloid has very short half life & rapid clearance by
R.E.S.
4 ) Technetium – labelled R.B.Cs.
5 ) Angiography ( Selective arteriography ).
Diagnosis : bleeding 1 ml / minute .
Advantages : 1) precise localization of the bleeding points. 2) not
requiring bowel preparation. 3) therapeutic options e.g. injection of
Vasopressin or embolization of gelofoam or cyano-acrylate .
Disadvantages : 1) time consuming. 2) the need for active bleeding. 3)
complications e.g. arterial thrombosis , hematoma , bleeding , embolus
bowel infarction & renal failure .
30.
Lower G.I. Bleeding6 ) Barium enema :
Air contrast barium enema ( diverticular disease)
Water soluble studies ( carcinoma ).
7 ) C.T. Scan of the abdomen & pelvis with contrast
enhancement.
8 ) M.R.I.
9 ) Enteroscopy .
31.
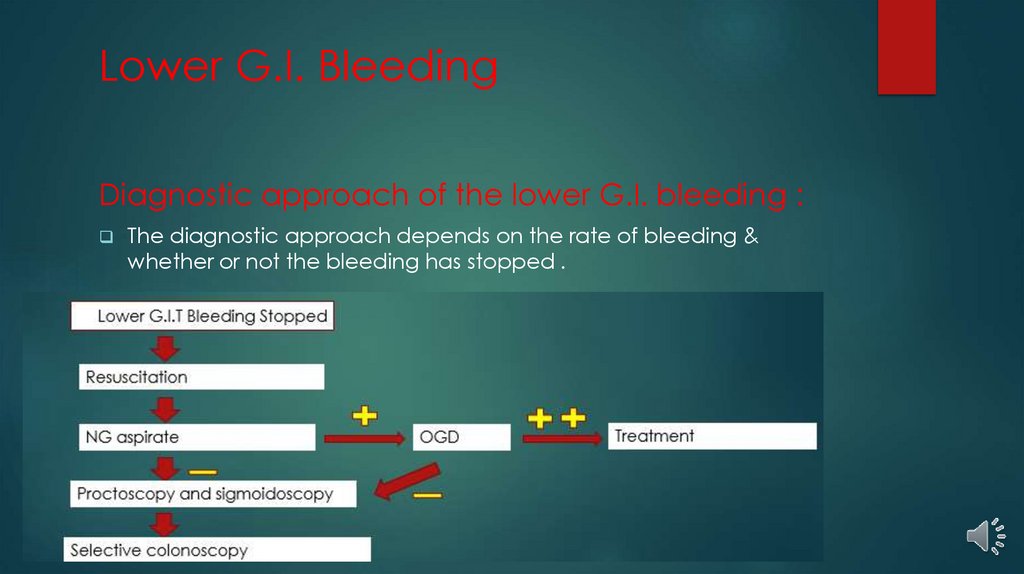
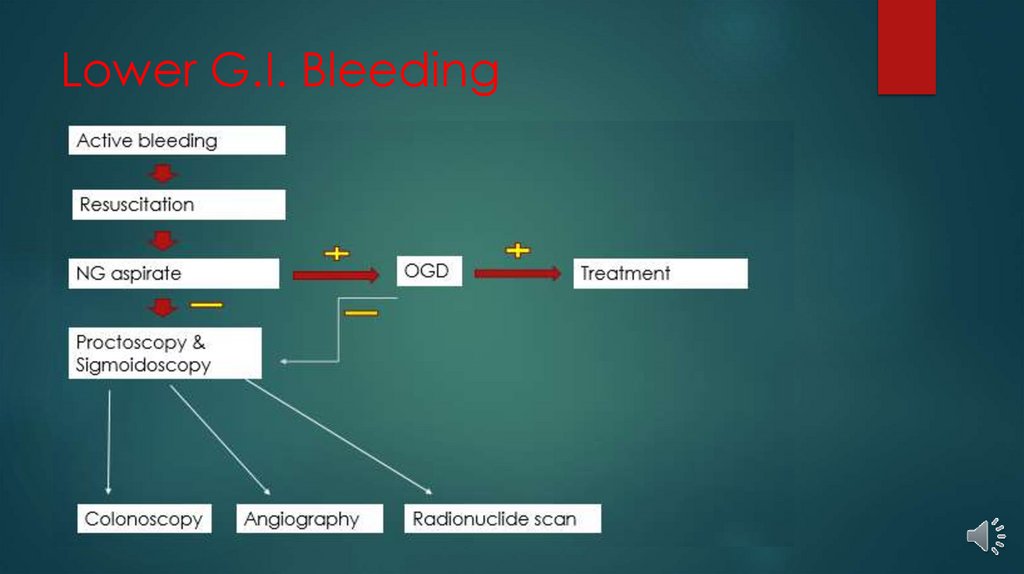
Lower G.I. BleedingDiagnostic approach of the lower G.I. bleeding :
The diagnostic approach depends on the rate of bleeding &
whether or not the bleeding has stopped .
32.
Lower G.I. Bleeding33.
Lower G.I. BleedingManagement of the common causes of the lower G.I.
bleeding :
1)
Diverticular disease :
Common in the left colon , the bleeding is arterial & severe .
The bleeding usually stop spontaneously in 80% of patients , but 25%
will rebleed .
Colonoscopy management ( Heater probe ) in small number of
patients .
Surgical treatment : surgical resection ( sub-total colectomy).
34.
Lower G.I. Bleeding2 ) Angiodysplasia :
Angiodysplasia is a specific mucosal vascular ectasia that develop as
degenerative process of aging .
Common in the caecum & ascending colon .
Management :
A) Colonoscopy with heat or laser coagulation ( effective in 80% with
higher Rebleeding rate – 20% of patients require more than one
colonoscopy treatment ).
Disadvantages of coagulation : perforation , delayed bleeding , postcoagulation syndrome ( abdominal pain , localized rebound
tenderness , leukocytosis but without evidence of colonic perforation ).
B ) Bowel resection .
35.
Lower G.I. Bleeding3) Ischaemic colitis :
Massive bleeding from infarcted colon .
Common in patients with repair of rupture A.A.A.
Clinical features : pain in the left lower abdomen , bloody diarrhea ,
signs of localized peritonitis .
Treatment : surgical resection .
4 ) I.B.D. :
Massive rectal bleeding occurs in extensive ulcerative colitis or
localized crohn,s disease .
Surgery is treatment of choice .
36.
Lower G.I. Bleeding5 ) Meckel,s diverticulum :
Meckel,s diverticulum usually occurs in children & adolescents , 2%
of the population , 60 cm from the ileo-caecal valve and often lined
with heteropic gastric epithelium .
10 – 20 %of these Meckel,s diverticulum are complicated with
bleeding .
Diagnosis : small bowel enema or pertechnetate isotope scan .
Treatment : surgical resection .








 biology
biology








