Similar presentations:
Hyaline membrane disease
1.
2.
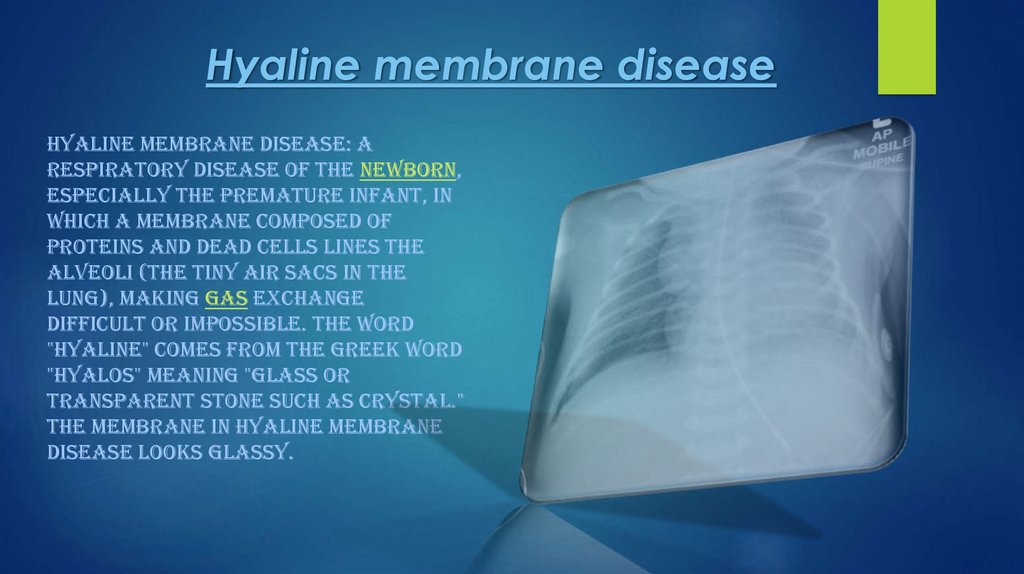
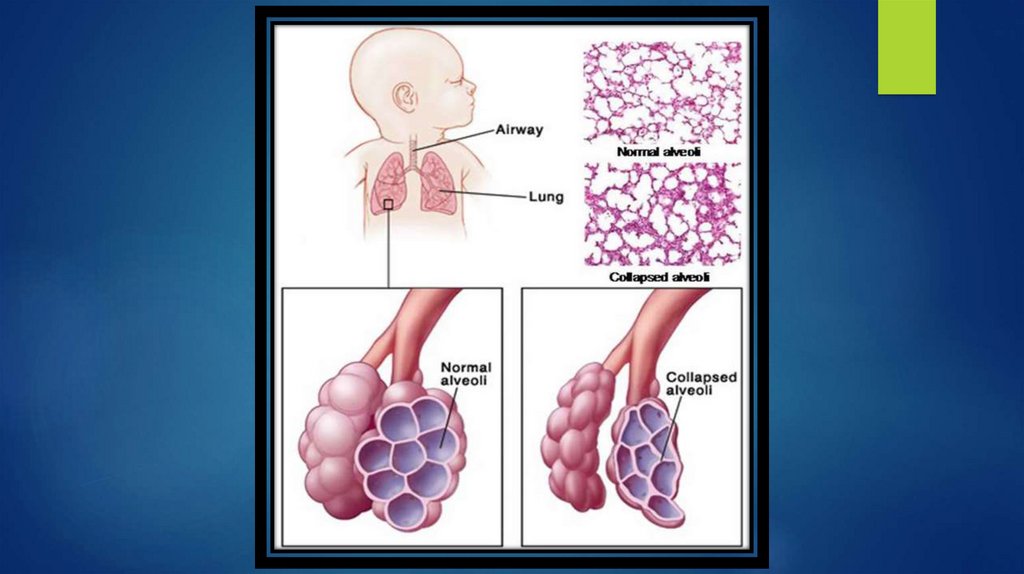
Hyaline membrane diseaseHYALINE MEMBRANE DISEASE: A
RESPIRATORY DISEASE OF THE NEWBORN,
ESPECIALLY THE PREMATURE INFANT, IN
WHICH A MEMBRANE COMPOSED OF
PROTEINS AND DEAD CELLS LINES THE
ALVEOLI (THE TINY AIR SACS IN THE
LUNG), MAKING GAS EXCHANGE
DIFFICULT OR IMPOSSIBLE. THE WORD
"HYALINE" COMES FROM THE GREEK WORD
"HYALOS" MEANING "GLASS OR
TRANSPARENT STONE SUCH AS CRYSTAL."
THE MEMBRANE IN HYALINE MEMBRANE
DISEASE LOOKS GLASSY.
3.
Hyaline membrane disease is now commonly calledrespiratory distress syndrome (RDS). It is caused by a
deficiency of a molecule called surfactant.
RDS almost always occurs in newborns born before 37
weeks of gestation. The more premature the baby is, the
greater is the chance of developing RDS. RDS is more
likely to occur in newborns of diabetic mothers.
Surfactant, a mixture of phospholipids and lipoproteins,
is secreted by lung cells. The air-fluid interface of the
film of water lining the alveoli of the lung (where the
exchange of oxygen and CO2 occurs) exerts large
forces that cause the alveoli to close if surfactant is
deficient. Lung compliance is decreased, and the work of
inflating the stiff lungs is increased
4.
The preterm newborn is further handicappedbecause his or her ribs are more easily deformed
(compliant). Breathing efforts therefore result in
deep sternal (breastbone) retractions but poor
air entry if the ribs are compliant compared with
the lungs. This results in diffuse atelectasis
(collapse of the lungs).
Rapid, labored, grunting respirations usually
develop immediately or within a few hours after
delivery, with retractions above and below the
breastbone and flaring of the nostrils. The extent
of atelectasis (lung collapse) and the severity of
respiratory failure progressively worsen.
5.
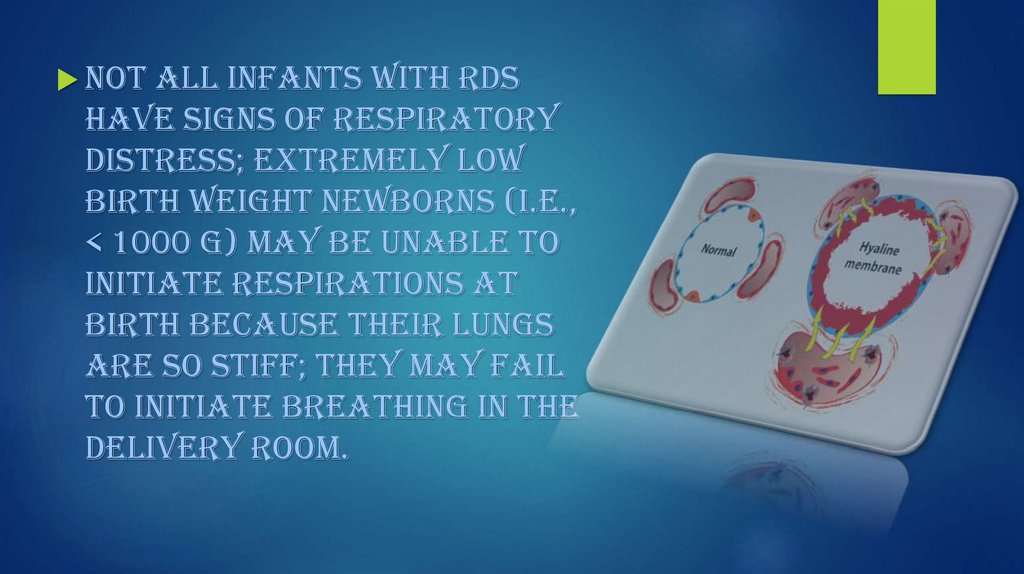
Notall infants with RDS
have signs of respiratory
distress; extremely low
birth weight newborns (i.e.,
< 1000 g) may be unable to
initiate respirations at
birth because their lungs
are so stiff; they may fail
to initiate breathing in the
delivery room.
6.
The incidence of RDS can be reducedby assessment of fetal lung
maturity to determine the optimal
time for delivery. When a fetus
must be delivered prematurely,
giving betamethasone
systemically to the mother for at
least 24 hours before delivery
induces fetal surfactant
production and usually reduces
the risk of RDS or decreases its
severity.
7.
Ifuntreated, severe RDS can result in
multiple organ failure and death.
However, if the newborn's ventilation
is adequately supported, surfactant
production will begin and RDS will
resolve by 4 or 5 days. Recovery is
hastened by treatment with
pulmonary surfactant.
8.
9.
Newborn respiratory distress syndromeNewborn respiratory distress syndrome (NRDS)
happens when a baby's lungs are not fully
developed and cannot provide enough oxygen,
causing breathing difficulties. It usually
affects premature babies.
It's also known as infant respiratory distress
syndrome, hyaline membrane disease or surfactant
deficiency lung disease.
Despite having a similar name, NRDS is not related
to acute respiratory distress syndrome (ARDS).
10.
11.
12.
Symptoms of NRDSTHE SYMPTOMS OF NRDS ARE OFTEN NOTICEABLE
IMMEDIATELY AFTER BIRTH AND GET WORSE OVER THE
FOLLOWING FEW DAYS.
THEY CAN INCLUDE:
BLUE-COLOURED LIPS, FINGERS AND TOES
RAPID, SHALLOW BREATHING
FLARING NOSTRILS
A GRUNTING SOUND WHEN BREATHING
13.
Diagnosing NRDSA number of tests can be used to diagnose NRDS and rule
out other possible causes.
These include:
a physical examination
blood tests to measure the amount of oxygen in the baby's
blood and check for an infection
a pulse oximetry test to measure how much oxygen is in the
baby's blood using a sensor attached to their fingertip, ear or
toe
a chest X-ray to look for the distinctive cloudy appearance of
the lungs in NRDS
14.
For better understandingHTTPS://WWW.YOUTUBE.COM/WATCH?V=KED0EVBKJF8
HTTPS://WWW.YOUTUBE.COM/WATCH?V=XWE7XWH7O1Y
HTTPS://WWW.YOUTUBE.COM/WATCH?V=R5-PEJFQ6WK


 medicine
medicine