Similar presentations:
Anthelmintic, antiprotozoal and antisyphilitic drugs
1.
Lecture 9Anthelmintic, Antiprotozoal and Antisyphilitic Drugs
1
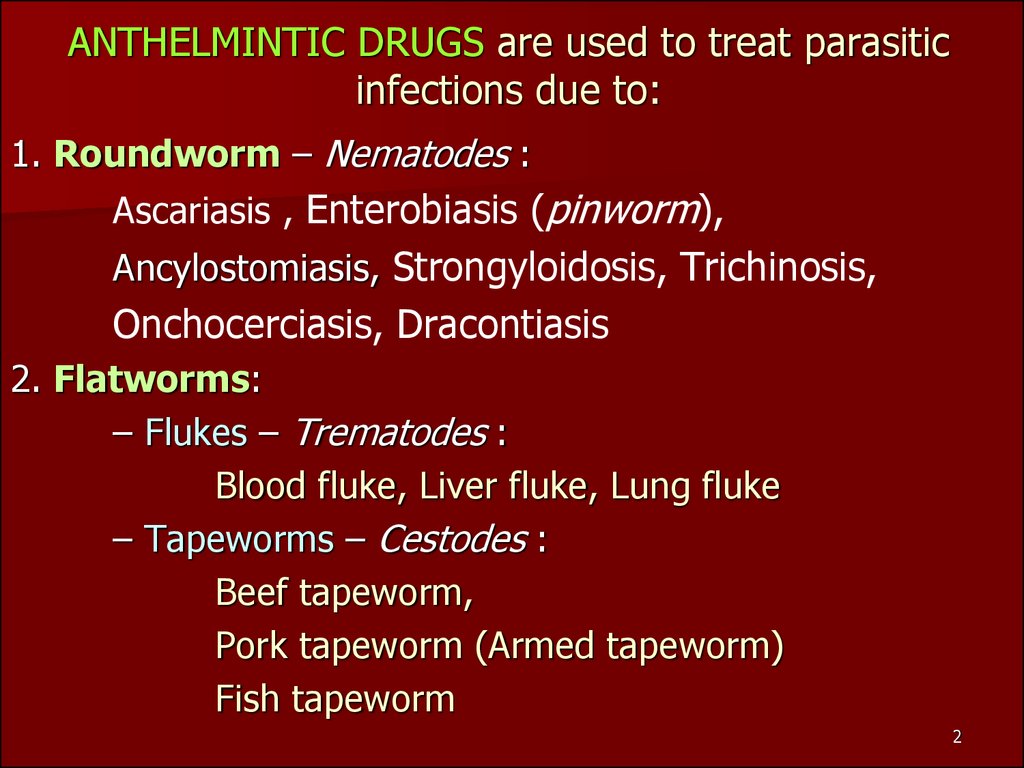
2. ANTHELMINTIC DRUGS are used to treat parasitic infections due to:
1. Roundworm – Nematodes :Ascariasis , Enterobiasis (pinworm),
Ancylostomiasis, Strongyloidosis, Trichinosis,
Onchocerciasis, Dracontiasis
2. Flatworms:
– Flukes – Trematodes :
Blood fluke, Liver fluke, Lung fluke
– Tapeworms – Cestodes :
Beef tapeworm,
Pork tapeworm (Armed tapeworm)
Fish tapeworm
2
3.
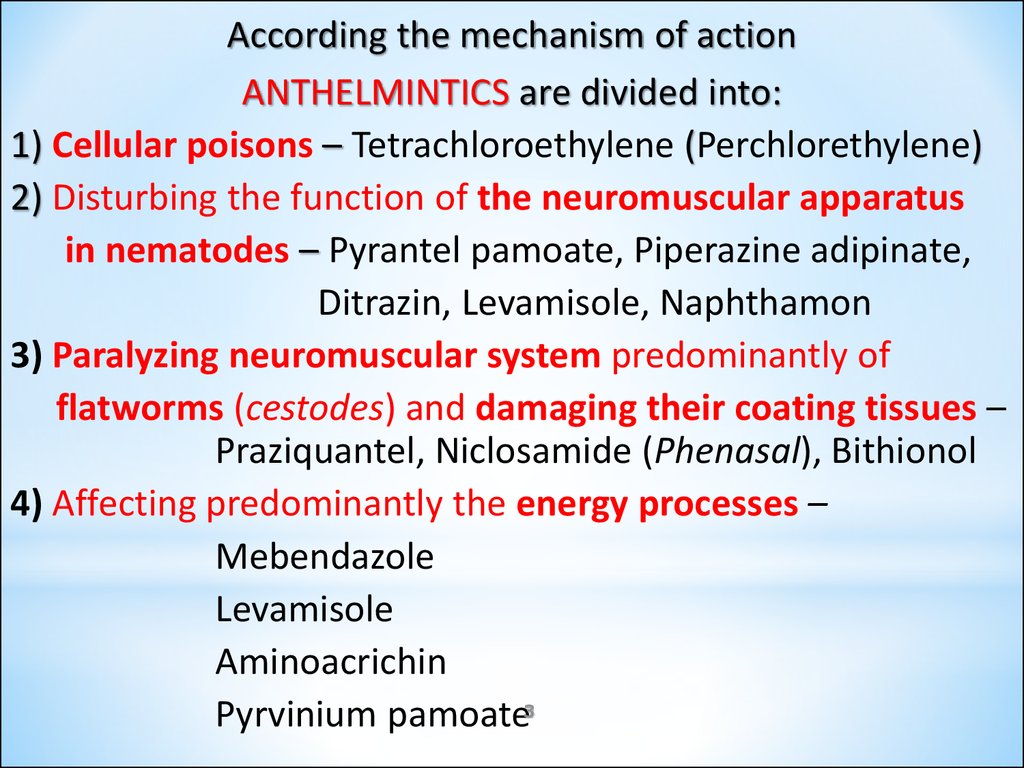
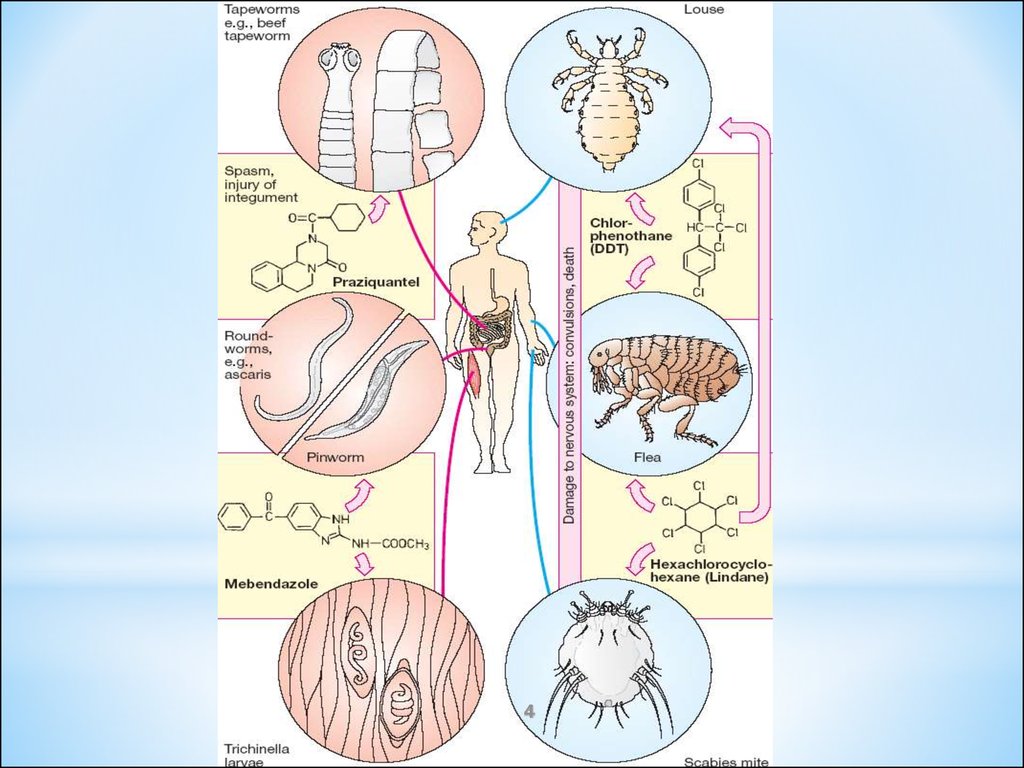
According the mechanism of actionANTHELMINTICS are divided into:
1) Cellular poisons – Tetrachloroethylene (Perchlorethylene)
2) Disturbing the function of the neuromuscular apparatus
in nematodes – Pyrantel pamoate, Piperazine adipinate,
Ditrazin, Levamisole, Naphthamon
3) Paralyzing neuromuscular system predominantly of
flatworms (cestodes) and damaging their coating tissues –
Praziquantel, Niclosamide (Phenasal), Bithionol
4) Affecting predominantly the energy processes –
Mebendazole
Levamisole
Aminoacrichin
Pyrvinium pamoate3
4.
45.
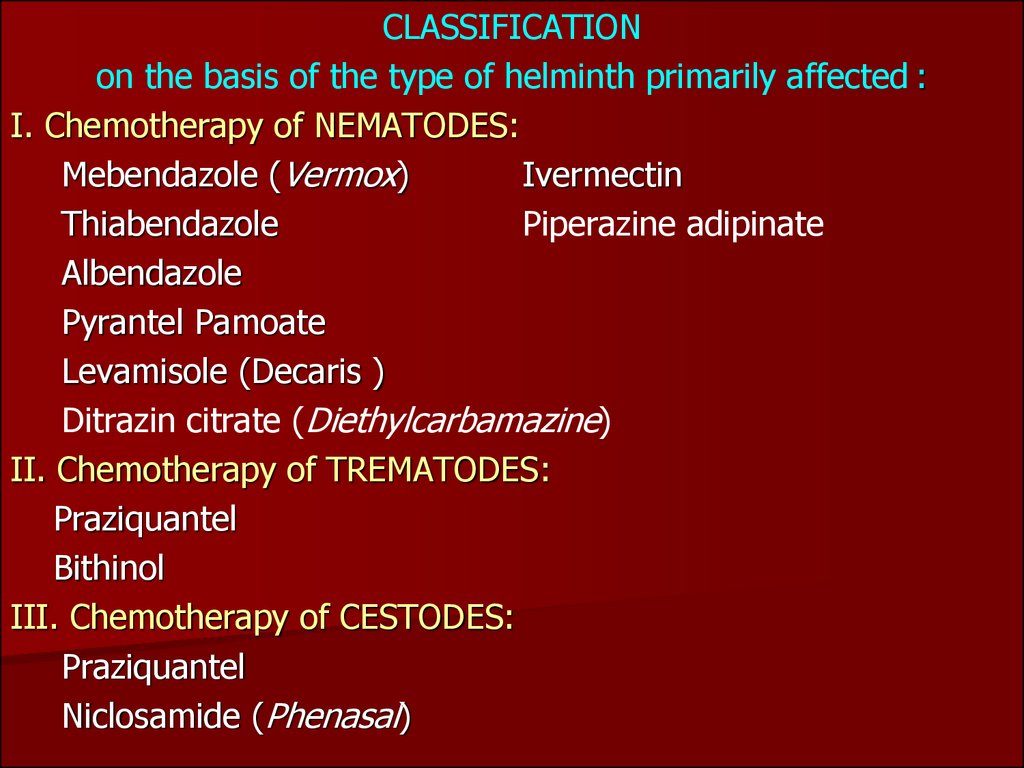
CLASSIFICATIONon the basis of the type of helminth primarily affected :
I. Chemotherapy of NEMATODES:
Mebendazole (Vermox)
Ivermectin
Thiabendazole
Piperazine adipinate
Albendazole
Pyrantel Pamoate
Levamisole (Decaris )
Ditrazin citrate (Diethylcarbamazine)
II. Chemotherapy of TREMATODES:
Praziquantel
Bithinol
III. Chemotherapy of CESTODES:
Praziquantel
Niclosamide (Phenasal)
6.
Mebendazole (Vermox)- Tab. 0.5 g –
a synthetic benzimidazole compound is a drug of choice in the treatment of infections by:
Pinworm (Enterobius vermicularis),
Roundworm (Ascariasis lumbricoides),
Whipworm (Trichuris trichiura)
Hookworm (Necator americanus and
Ancylostoma duodenale).
Mechanism of action:
Binding and Interfiaring with the synthesis of
β-tubulin and thus parasite’s microtubules =>
=> GLUCOSE UPTAKE by the worm.
The helminths become immobilized and die slowly,
so they may be expelled from the GIT up to 3 days
after drug therapy is completed.
7.
Pyrantel pamoate - Tab 0.25; Susp.5%-15 mlPinworm (Enterobius vermicularis)
Roundworm (Ascariasis lumbricoides)
Hookworm (Necator americanus and
Ancylostoma duodenale)
Mechanism of action:
Depolarizes Neuromuscular Junction of
the helminth => its Spasm and Paralysis
Anticholinesterase activity
Adverse effects:
Nausea, vomiting, and diarrhea.
8.
Levamisole (Decaris)- Tab. 50 and 150 mgis a synthetic imidazothiazole derivative
Highly effective against:
Roundworms (Ascaris and Trichostrongylus)
Moderately effective:
Hookworm
Mechanism of action:
Nicotine-like action, stimulation and
subsequently block of the neuromuscular junctions.
The paralyzed worms are then passed in the feces.
Levamisole occurs IMMUNOMODULATING EFFECT and
is used as adjunct therapy with FLUOROURACIL
for the treatment of COLON CANCER
9.
Praziquantel is a broad-spectrum anthelminthicSchistosomes: Blood fluke,
Liver fluke, Lung fluke
Cestodes infections like Cysticercosis
Beef tapeworm
Pork tapeworm
Fish tapeworm
Mechanism of action:
Permeability to the Ca2+ =>
=> Musculature Contraction and
eventual Paralysis and death of the worm.
Modifies the parasite so that it becomes susceptible to
the host’s normal immune responses.
10.
Phenasal (NiclosamideCESTODES:
– Tab. 0.25 g)
Beef tapeworm
Pork tapeworm
Fish tapeworm
Mechanism of action: inhibition of the parasite's
Mitochondrial Anaerobic Phosphorylation of ADP, which
produces usable energy in the form of ATP.
Lethal for the Cestode's Scolex and Segments
but not for the Ova.
A Laxative is administered prior to
oral administration of
Phenasal
11.
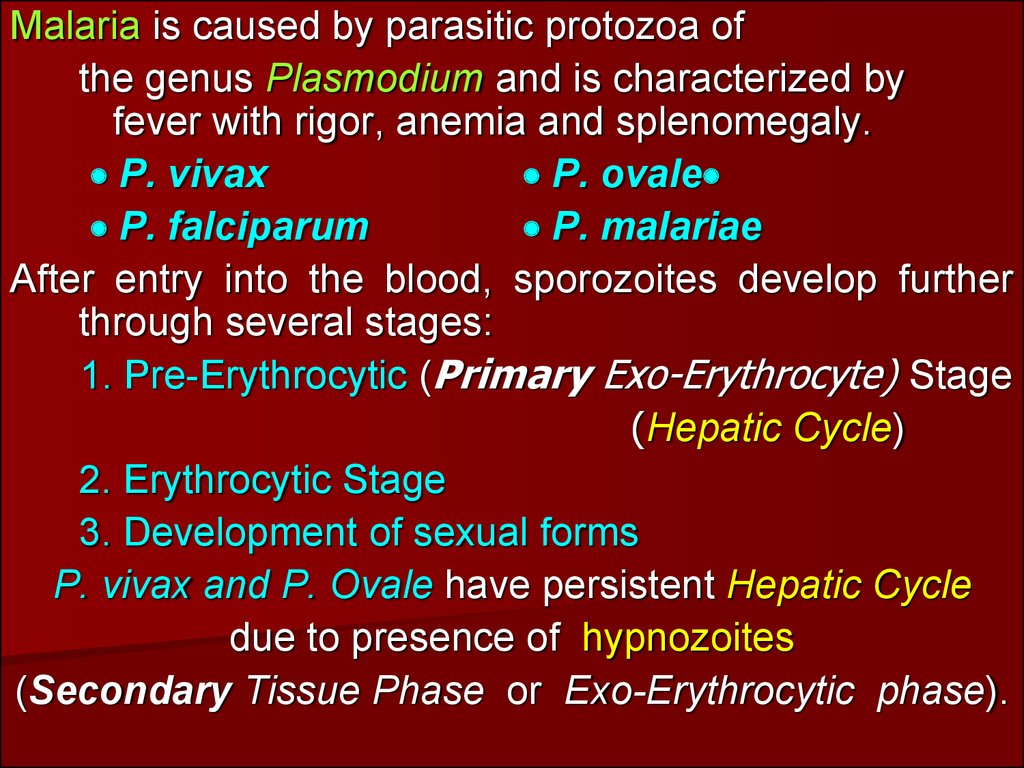
Malaria is caused by parasitic protozoa ofthe genus Plasmodium and is characterized by
fever with rigor, anemia and splenomegaly.
P. vivax
P. ovale
P. falciparum
P. malariae
After entry into the blood, sporozoites develop further
through several stages:
1. Pre-Erythrocytic (Primary Exo-Erythrocyte) Stage
(Hepatic Cycle)
2. Erythrocytic Stage
3. Development of sexual forms
P. vivax and P. Ovale have persistent Hepatic Cycle
due to presence of hypnozoites
(Secondary Tissue Phase or Exo-Erythrocytic phase).
12.
1213.
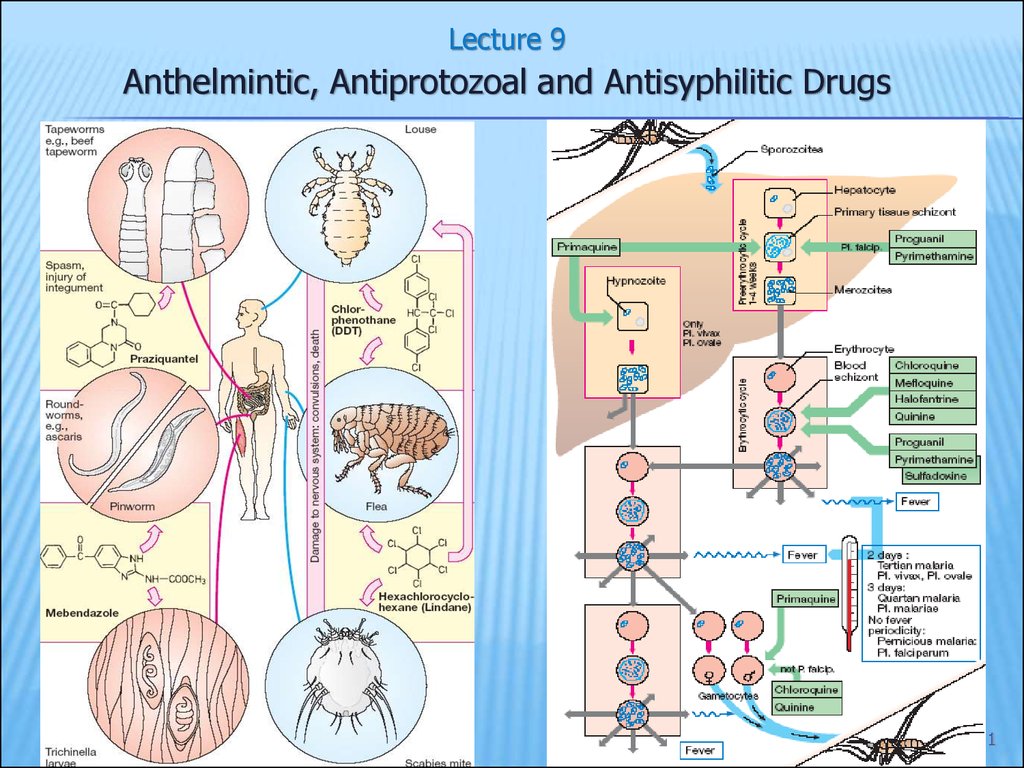
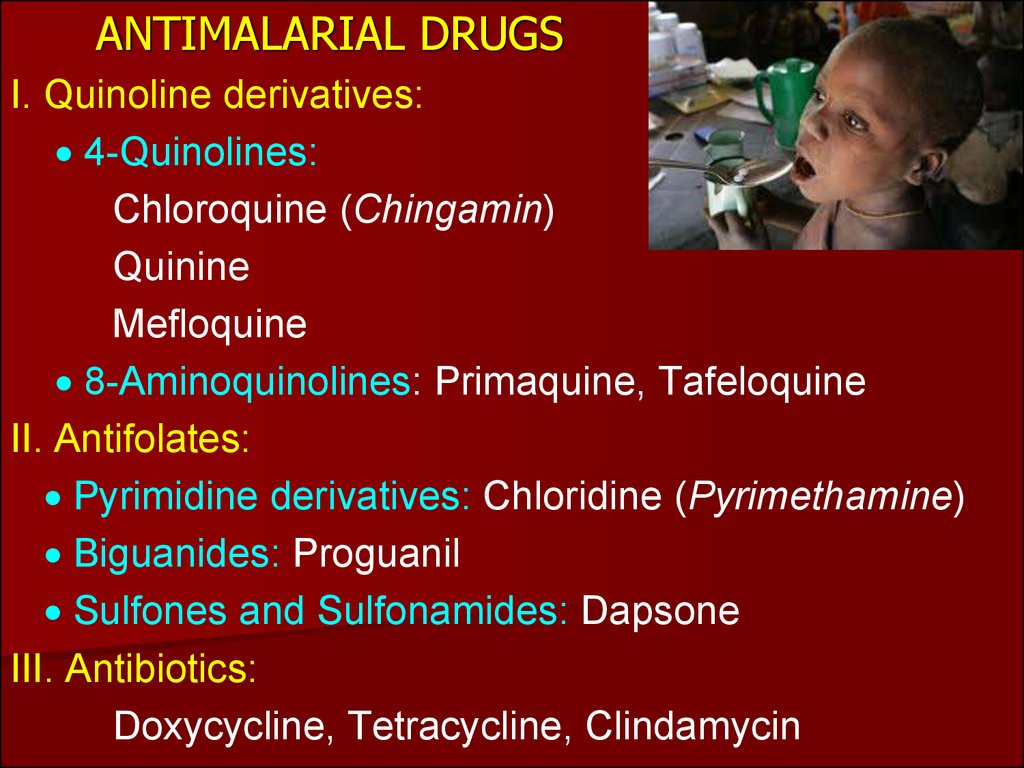
ANTIMALARIAL DRUGSI. Quinoline derivatives:
4-Quinolines:
Chloroquine (Chingamin)
Quinine
Mefloquine
8-Aminoquinolines: Primaquine, Tafeloquine
II. Antifolates:
Pyrimidine derivatives: Chloridine (Pyrimethamine)
Biguanides: Proguanil
Sulfones and Sulfonamides: Dapsone
III. Antibiotics:
Doxycycline, Tetracycline, Clindamycin
14.
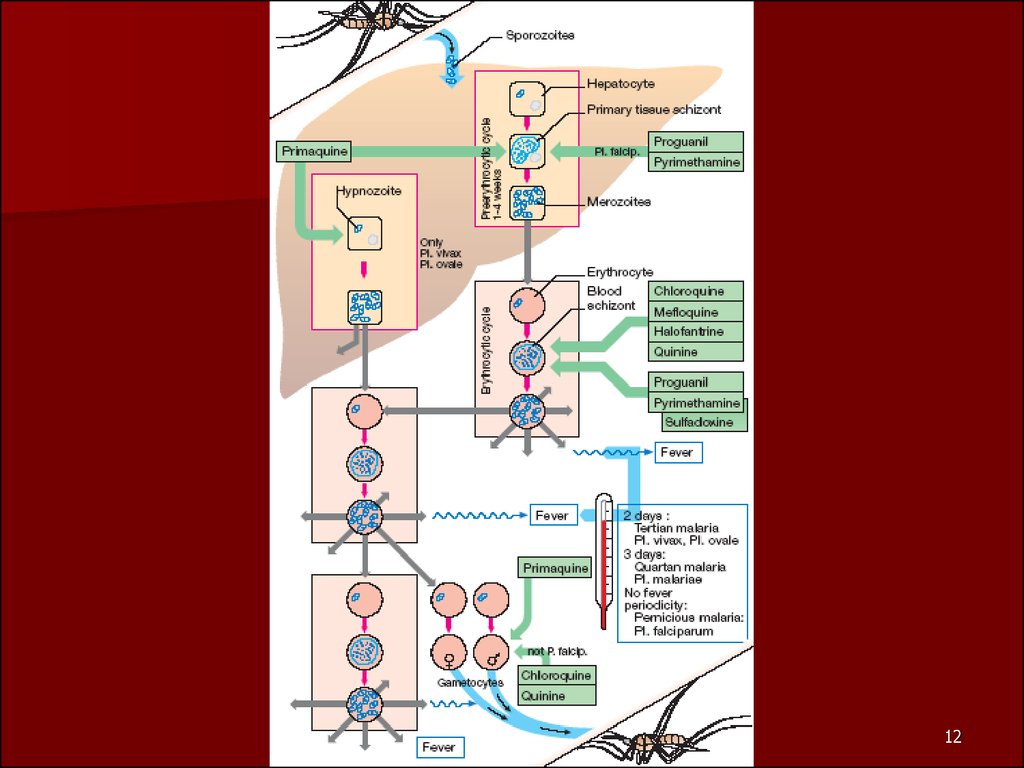
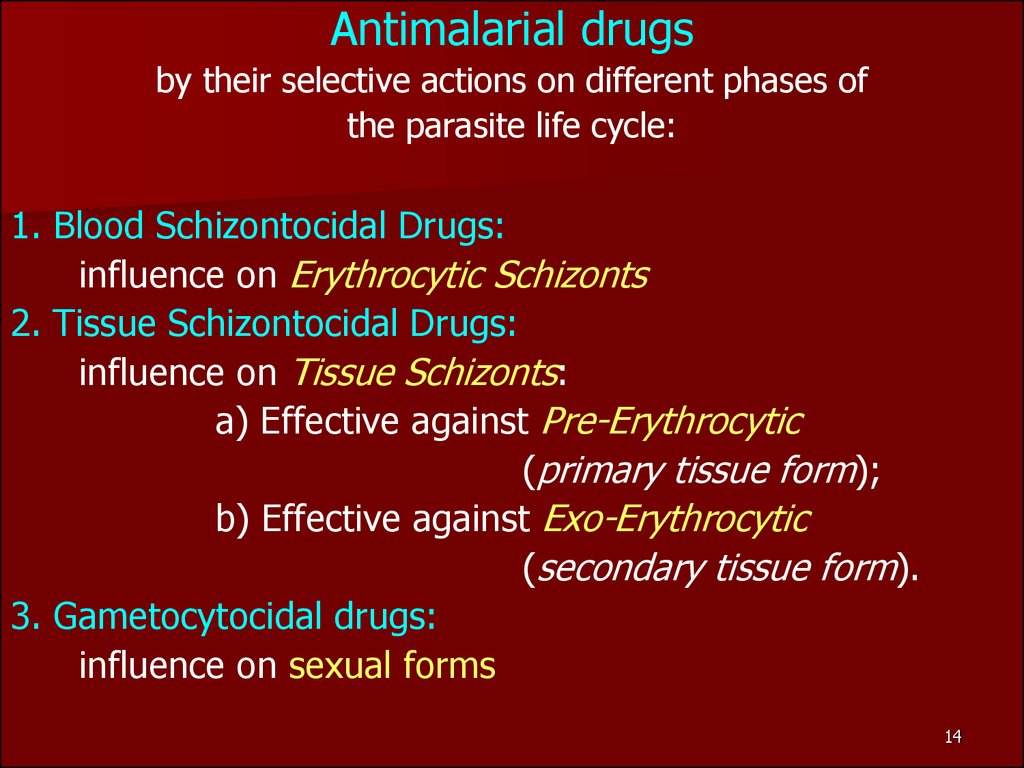
Antimalarial drugsby their selective actions on different phases of
the parasite life cycle:
1. Blood Schizontocidal Drugs:
influence on Erythrocytic Schizonts
2. Tissue Schizontocidal Drugs:
influence on Tissue Schizonts:
a) Effective against Pre-Erythrocytic
(primary tissue form);
b) Effective against Exo-Erythrocytic
(secondary tissue form).
3. Gametocytocidal drugs:
influence on sexual forms
14
15.
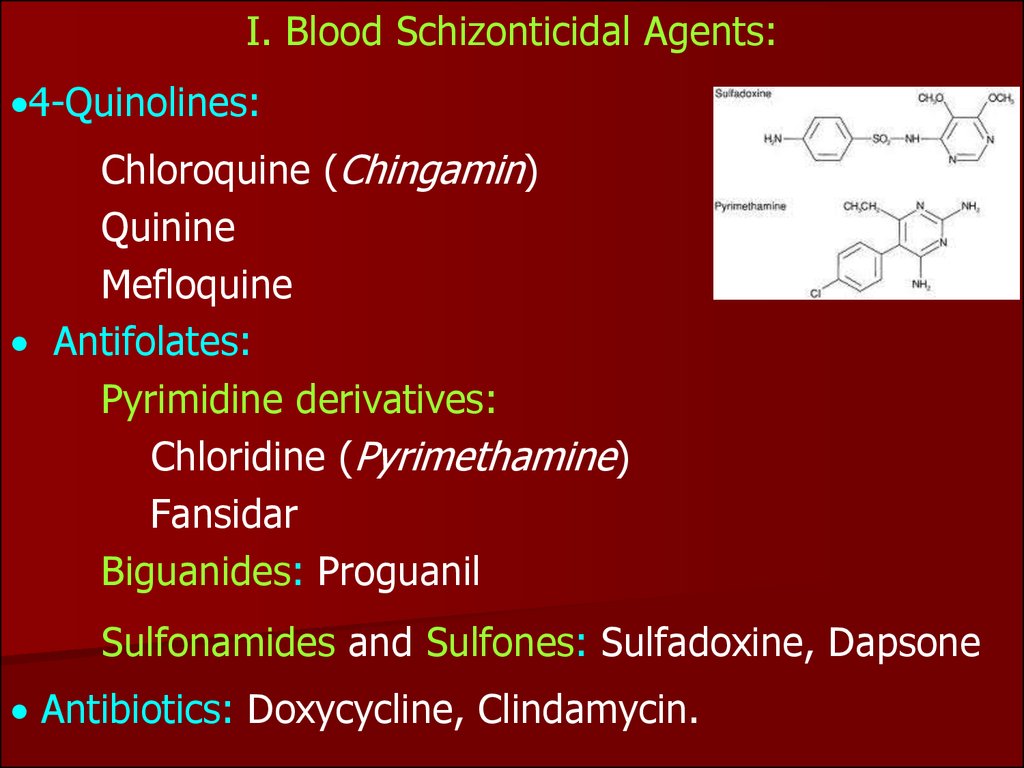
I. Blood Schizonticidal Agents:4-Quinolines:
Chloroquine (Chingamin)
Quinine
Mefloquine
Antifolates:
Pyrimidine derivatives:
Chloridine (Pyrimethamine)
Fansidar
Biguanides: Proguanil
Sulfonamides and Sulfones: Sulfadoxine, Dapsone
Antibiotics: Doxycycline, Clindamycin.
16.
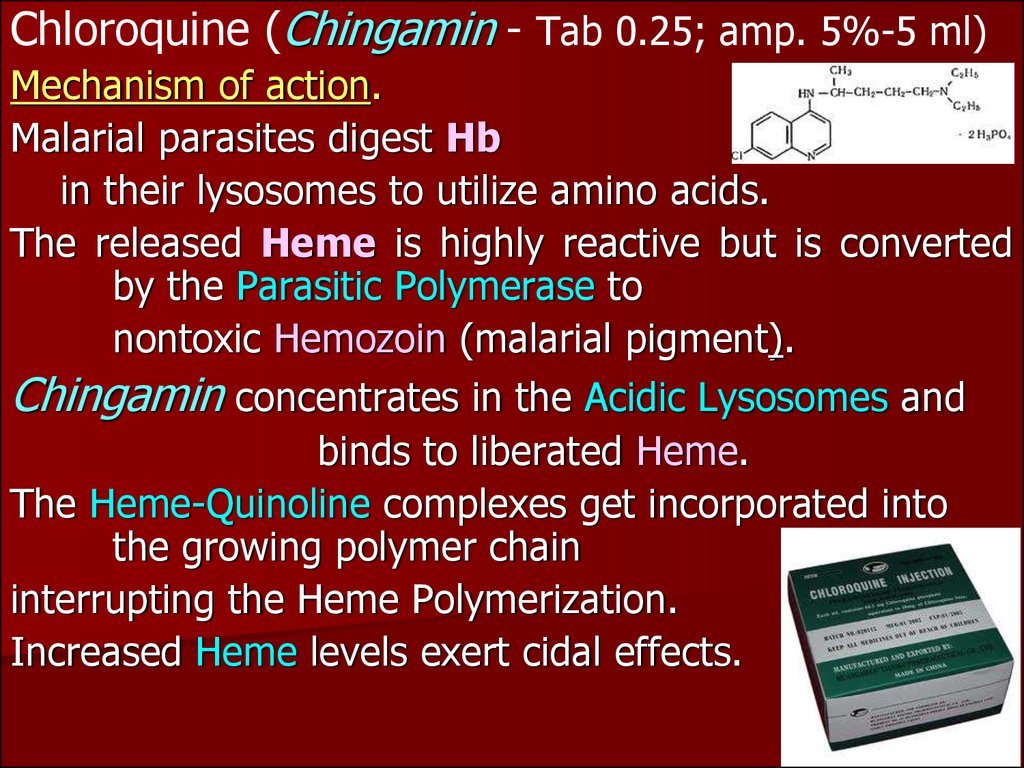
Chloroquine (Chingamin - Tab 0.25; amp. 5%-5 ml)Mechanism of action.
Malarial parasites digest Hb
in their lysosomes to utilize amino acids.
The released Heme is highly reactive but is converted
by the Parasitic Polymerase to
nontoxic Hemozoin (malarial pigment).
Chingamin concentrates in the Acidic Lysosomes and
binds to liberated Heme.
The Heme-Quinoline complexes get incorporated into
the growing polymer chain
interrupting the Heme Polymerization.
Increased Heme levels exert cidal effects.
17.
Pharmacological Effects of ChloroquineAntimalarial action –
DNA synthesis: disrupts the tertiary structure of
the nucleonic acid in the parasite
Amebicidal action
Anti-inflammatory action –
Antagonizes
Histamine and Serotonin;
Inhibits PG effects by inhibiting conversion of
Arachidonic Acid to PG F2.
Inhibits Chemotaxis of:
Polymorphonuclear Leukocytes, Macrophages, and
Eosinophils.
18.
CLINICAL USES of CHLOROQUINE:Treatment and Chemoprophylaxis of:
Malaria, Acute Attack of Malaria,
Extraintestinal Amebiasis
Rheumatoid Arthritis, Lupus Erythematosus
DOSAGE of CHINGAMIN
SUPPRESSIVE IN ACUTE ATTACK:
Initial dose 1 g followed by 0.5 g after 6 hours and
0.5 g daily thereafter for 2 days followed
by 0.5 g once a week for 3 months.
SUPPRESSIVE PROPHYLAXIS:
0.5 g PO on same day once weekly beginning
2 weeks prior to exposure
Adverse effects: skin reactions, dyspepsia,
depigmentation and loss of hair, retinopathy,
bone-marrow suppression.
19.
Quinine is the levo rotatory alkaloidobtained from Cinchona Bark.
It is an erythrocyte schizontocide
for all species of plasmodia and useful
only as suppressive;
less effective and more toxic than chloroquine.
CINCHONISM:
resembles SALICYLISM :
ringing in the ears, headache, GI distress, cardiovascular effects
(hypotension, collapse, conduction disturbances), tinnitus,
deafness, vertigo, blurred vision, disturbances of colour vision,
photophobia and total blindness;
skin rashes, seizures, and delirium.
Death may occur due to respiratory arrest.
TREATMENT: gastric lavage,
fluid and electrolyte replacement, artificial respiration,
stabilization of hemodynamics and renal function.
Anaphylactic reactions may require
Adrenaline, Corticosteroids, and Antihistamines.
20.
Chloridine (Pyrimethamine), a pyrimidine derivative-an Antifolate agent that is frequently employed as a
blood schizontocide to produce a radical cure.
-It also acts as a strong sporontocide in the mosquito’s
gut when the mosquito ingests it with the blood
of action: Inhibits Dihydrofolate Reductase
In contrast to Trimethoprim, it has very poor action on
bacterial dihydrofolate reductase.
Under the influence Pyrimethamine, schizogony of
malarial parasite in blood gradually stops.
At high doses it inhibits Toxoplasma gondii.
Effective against the Erythrocytic Forms but its action
-Mechanism
is slow.
Effective against the Pre-Erythrocytic forms,
INEFFECTIVE against the Exo-Erythrocytic forms.
21.
II. TISSUE SCHIZONTICIDAL AGENTSChloridine (Pyrimethamine) is referred to drugs
suppressing the PRE-ERYTHROCYTIC forms,,
but it is ineffective against the Exo-erythrocytic forms.
ONLY the 8-aminoquinolines -
Primaquine, Tafenoquine
are effective against
the EXO-ERYTHROCYTIC forms
Radical cure – by acting on the parasites in the Liver:
Destroy GAMETOCYTES and SPREAD of INFECTION.
Primaquine
differs from other antimalarials in having
a marked effect on primary as well as secondary tissue
phases of the malarial plasmodium.
It is highly active against Gametocytes and Hypnozoites.
22.
III. DRUGS for CHEMOPROPHYLAXIS –block the link between the Exo-Erythrocytic Stage
and the Erythrocytic Stage :
Chloroquine
Mefloquine
Proguanil
Pyrimethamine
Dapsone
Doxycycline
23.
IV. DRUGS to PREVENT TRANSMISSION:Primaquine
Proguanil
Chloridine (Pyrimethamine)
Destroy the GAMETOCYTES,
Preventing Transmission by the Mosquito and
Preventing the Increase of the Human
Reservoir of the Disease
24.
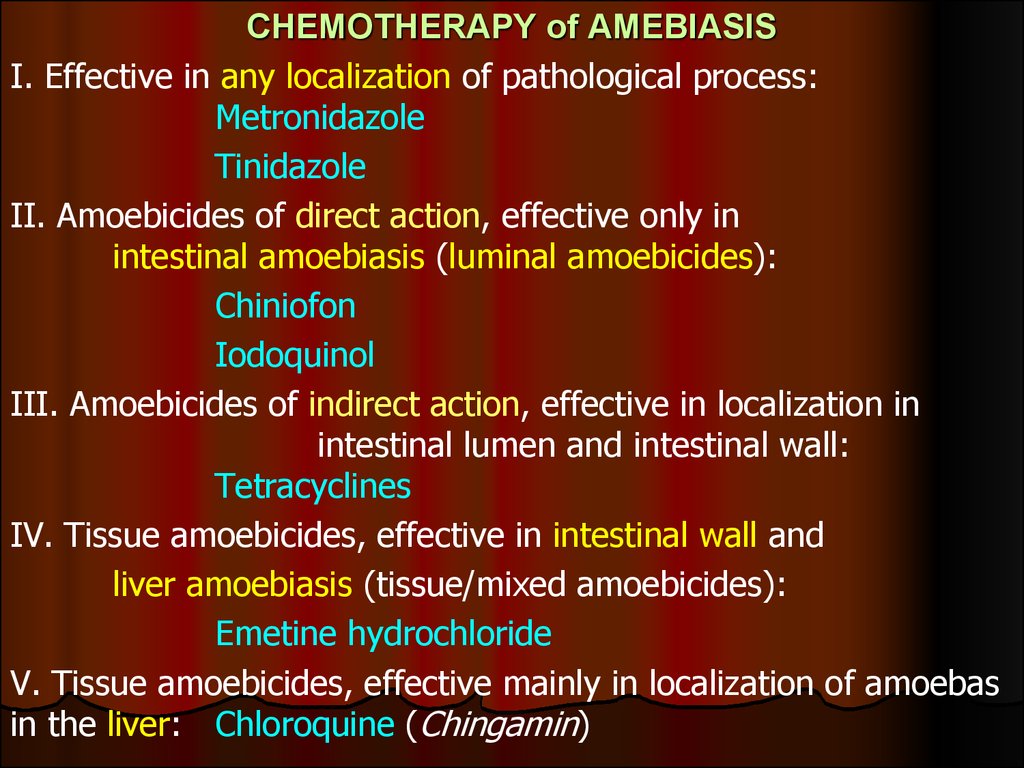
CHEMOTHERAPY of AMEBIASISI. Effective in any localization of pathological process:
Metronidazole
Tinidazole
II. Amoebicides of direct action, effective only in
intestinal amoebiasis (luminal amoebicides):
Chiniofon
Iodoquinol
III. Amoebicides of indirect action, effective in localization in
intestinal lumen and intestinal wall:
Tetracyclines
IV. Tissue amoebicides, effective in intestinal wall and
liver amoebiasis (tissue/mixed amoebicides):
Emetine hydrochloride
V. Tissue amoebicides, effective mainly in localization of amoebas
in the liver: Chloroquine (Chingamin)
25.
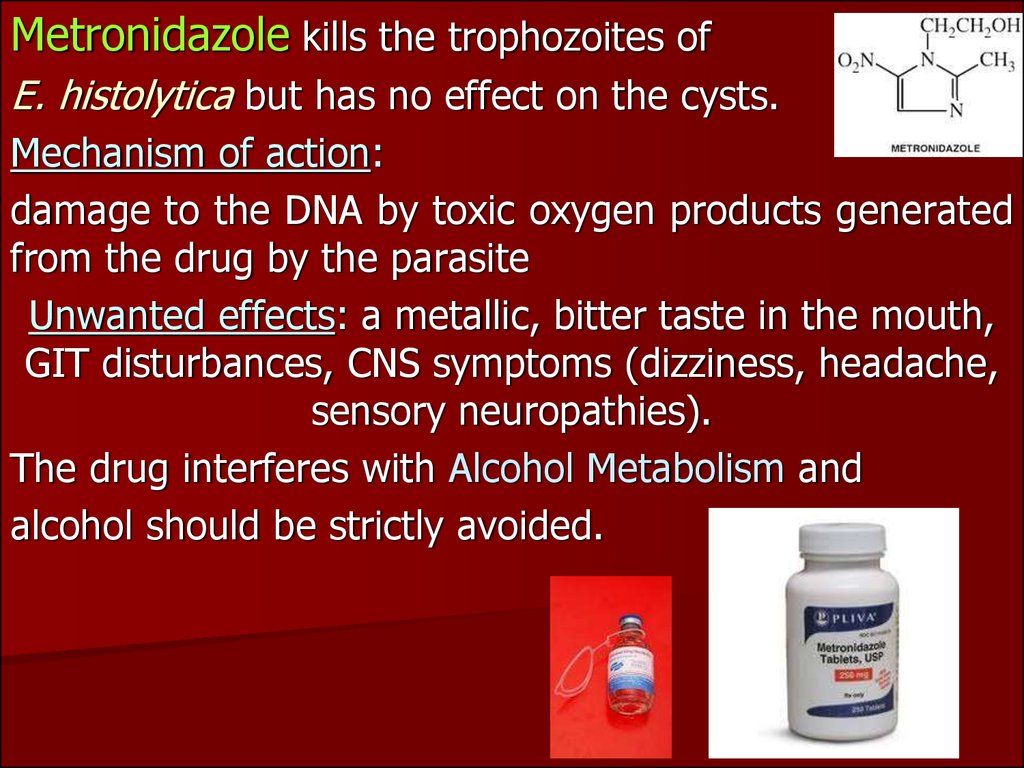
Metronidazole kills the trophozoites ofE. histolytica but has no effect on the cysts.
Mechanism of action:
damage to the DNA by toxic oxygen products generated
from the drug by the parasite
Unwanted effects: a metallic, bitter taste in the mouth,
GIT disturbances, CNS symptoms (dizziness, headache,
sensory neuropathies).
The drug interferes with Alcohol Metabolism and
alcohol should be strictly avoided.
26.
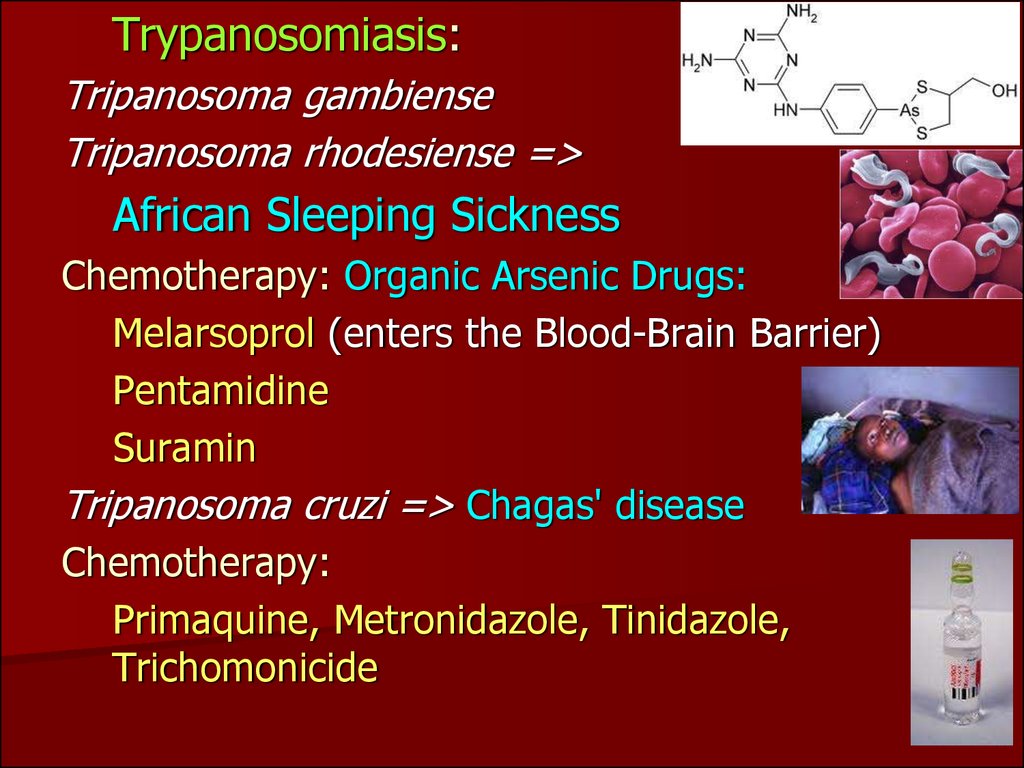
Trypanosomiasis:Tripanosoma gambiense
Tripanosoma rhodesiense =>
African Sleeping Sickness
Chemotherapy: Organic Arsenic Drugs:
Melarsoprol (enters the Blood-Brain Barrier)
Pentamidine
Suramin
Tripanosoma cruzi => Chagas' disease
Chemotherapy:
Primaquine, Metronidazole, Tinidazole,
Trichomonicide
27.
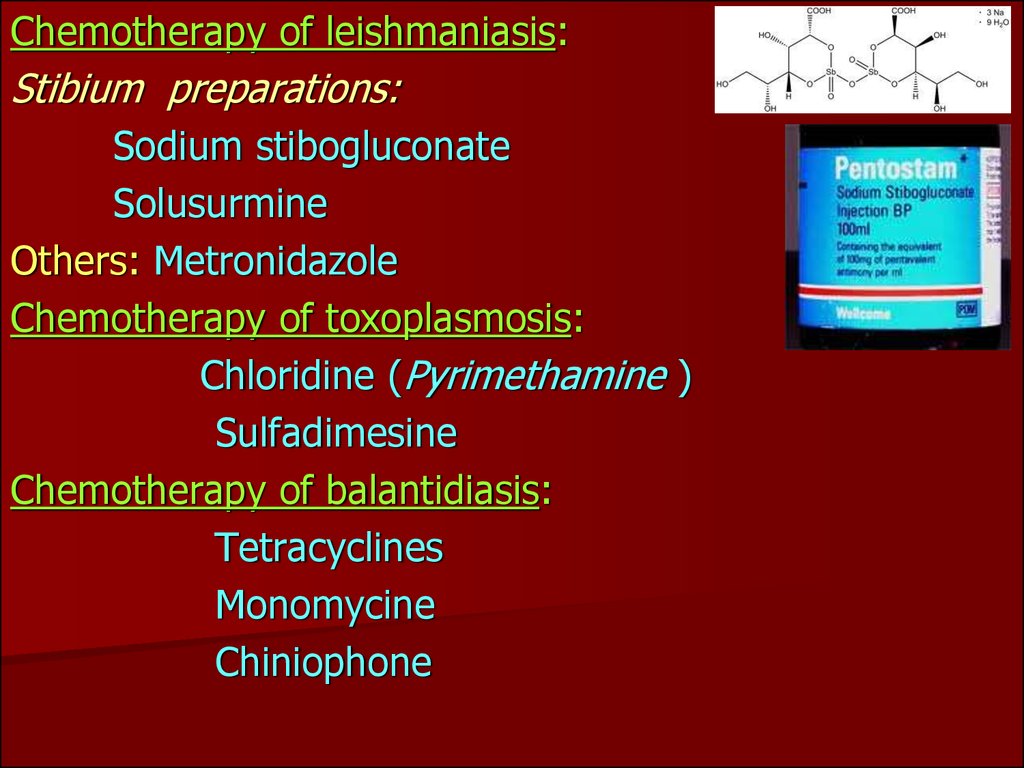
Chemotherapy of leishmaniasis:Stibium preparations:
Sodium stibogluconate
Solusurmine
Others: Metronidazole
Chemotherapy of toxoplasmosis:
Chloridine (Pyrimethamine )
Sulfadimesine
Chemotherapy of balantidiasis:
Tetracyclines
Monomycine
Chiniophone
28.
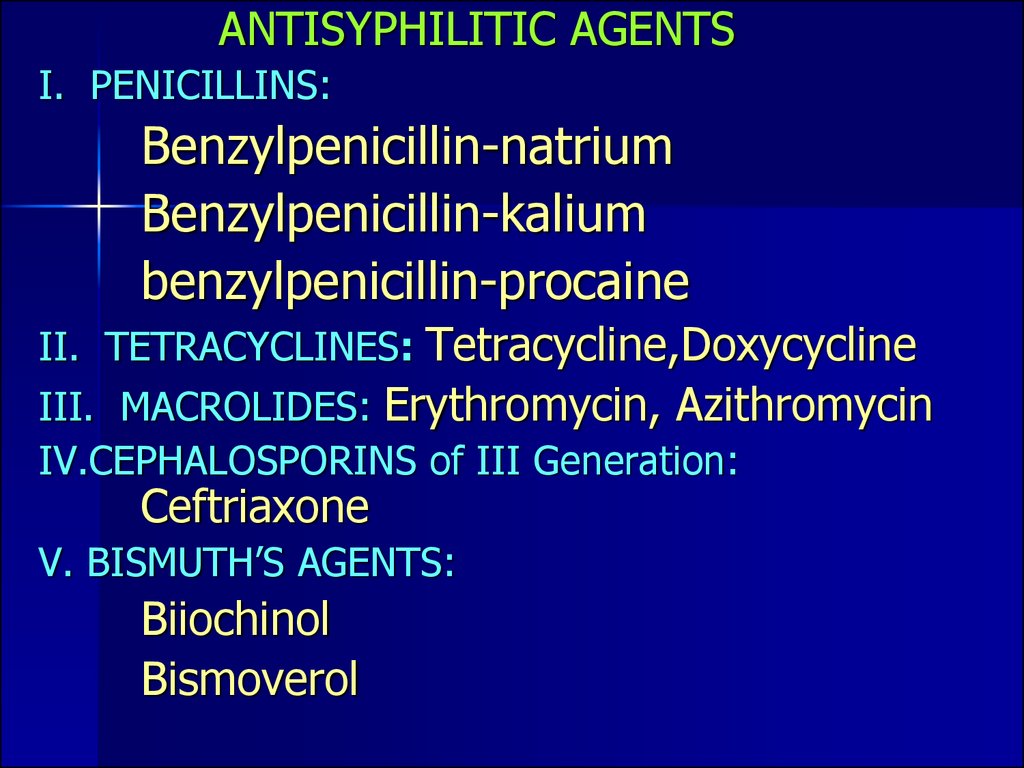
ANTISYPHILITIC AGENTSI. PENICILLINS:
Benzylpenicillin-natrium
Benzylpenicillin-kalium
benzylpenicillin-procaine
II. TETRACYCLINES: Tetracycline,Doxycycline
III. MACROLIDES: Erythromycin, Azithromycin
IV.CEPHALOSPORINS of III Generation:
Ceftriaxone
V. BISMUTH’S AGENTS:
Biiochinol
Bismoverol



 medicine
medicine