Similar presentations:
Transitional states in newborns
1. Transitional states in newborns assistant prof. of Hospital Paediatrics department with course of child infectious diseases
2.
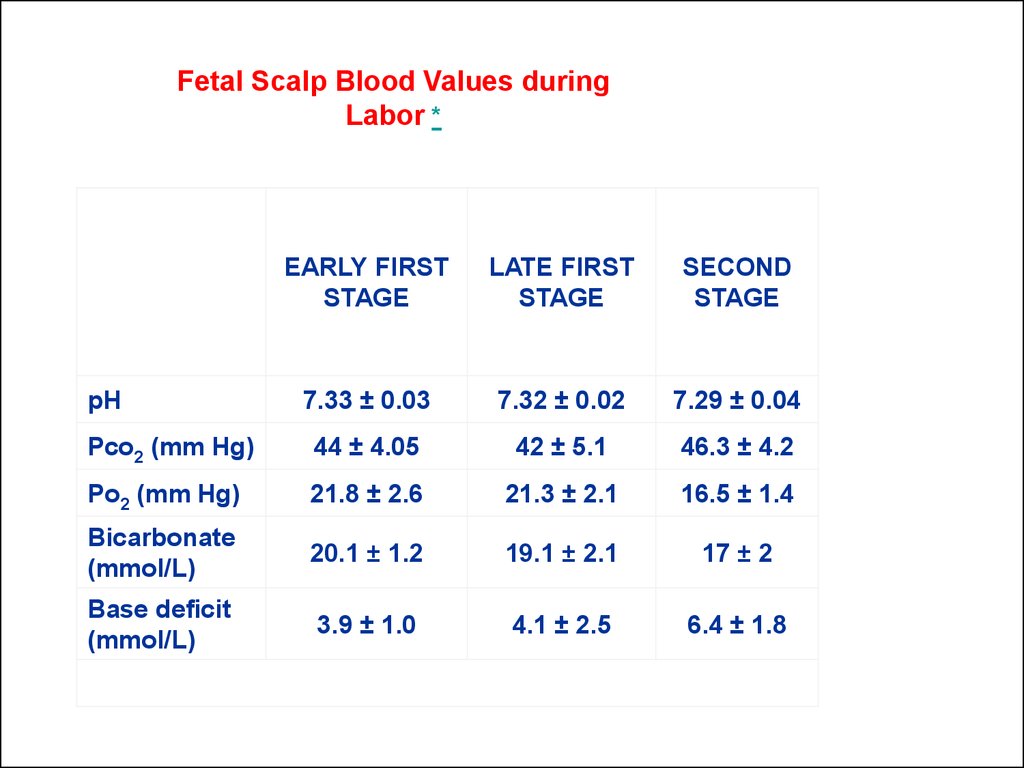
Fetal Scalp Blood Values duringLabor *
EARLY FIRST
STAGE
LATE FIRST
STAGE
SECOND
STAGE
7.33 ± 0.03
7.32 ± 0.02
7.29 ± 0.04
Pco2 (mm Hg)
44 ± 4.05
42 ± 5.1
46.3 ± 4.2
Po2 (mm Hg)
21.8 ± 2.6
21.3 ± 2.1
16.5 ± 1.4
Bicarbonate
(mmol/L)
20.1 ± 1.2
19.1 ± 2.1
17 ± 2
Base deficit
(mmol/L)
3.9 ± 1.0
4.1 ± 2.5
6.4 ± 1.8
pH
3.
4.
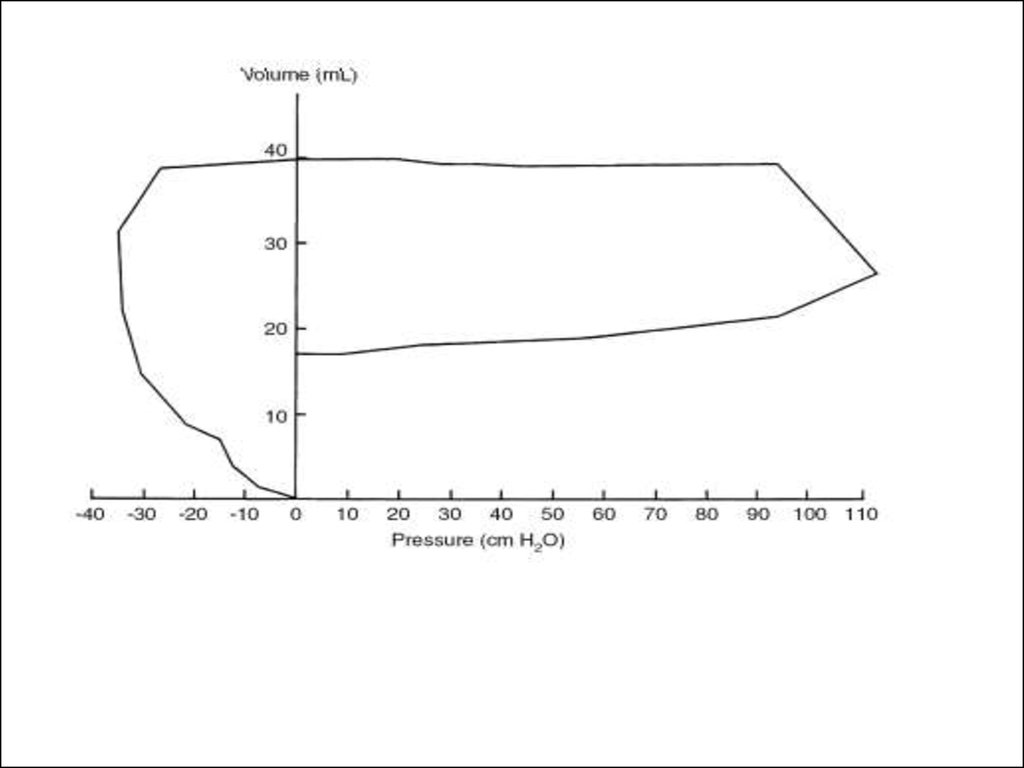
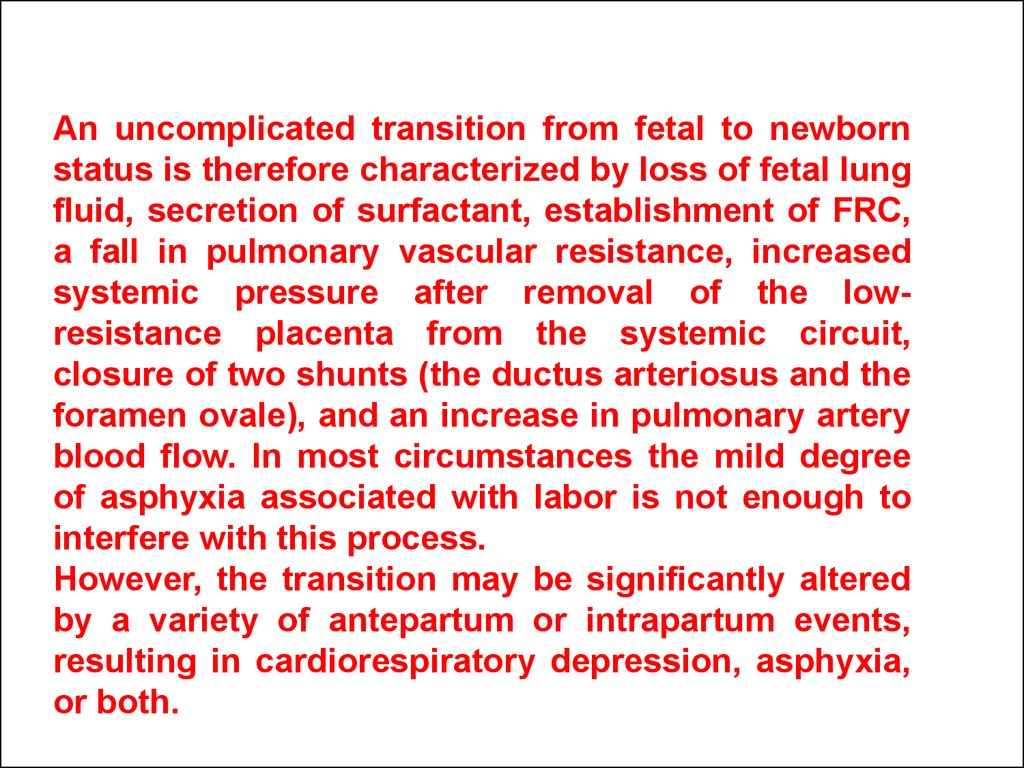
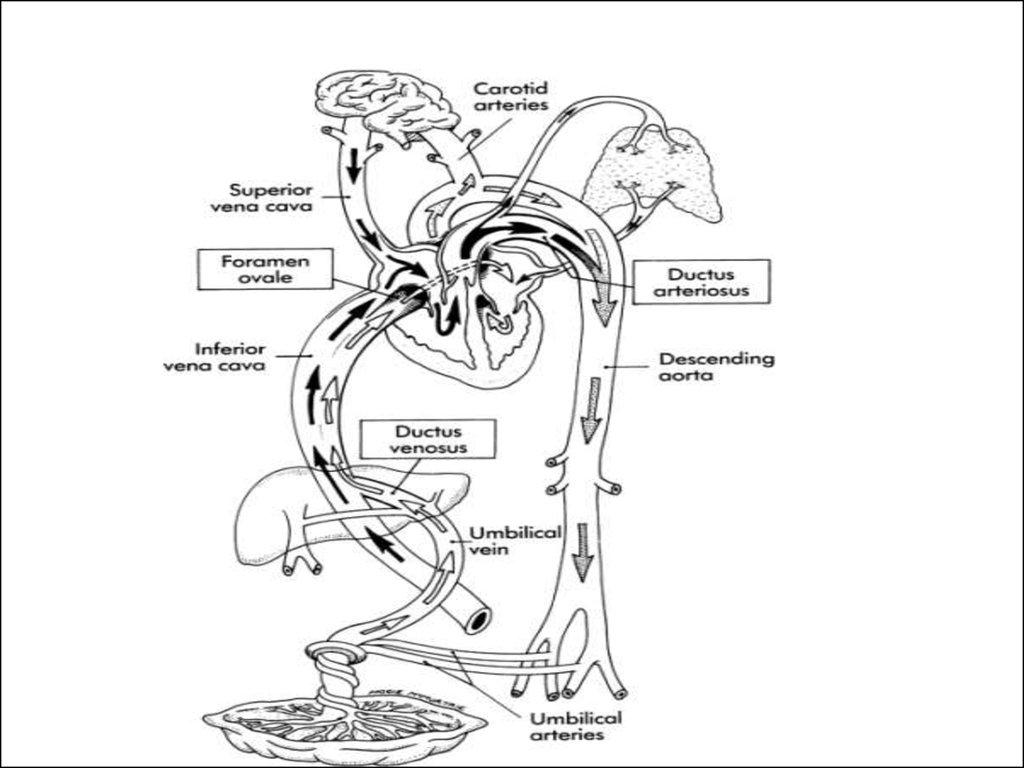
An uncomplicated transition from fetal to newbornstatus is therefore characterized by loss of fetal lung
fluid, secretion of surfactant, establishment of FRC,
a fall in pulmonary vascular resistance, increased
systemic pressure after removal of the lowresistance placenta from the systemic circuit,
closure of two shunts (the ductus arteriosus and the
foramen ovale), and an increase in pulmonary artery
blood flow. In most circumstances the mild degree
of asphyxia associated with labor is not enough to
interfere with this process.
However, the transition may be significantly altered
by a variety of antepartum or intrapartum events,
resulting in cardiorespiratory depression, asphyxia,
or both.
5.
6.
7.
8.
9.
In contrast with preterm infants, healthy termneonates have basal sodium handling similar to
that of adults.
Their FENa is less than 1%, although a
transient increase in FENa occurs during the
diuretic phase that occurs on the second and
third days of life.
10.
11. Transient Cutaneous Lesions
A number of benign and transient lesionsof the skin are commonly observed in a
normal nursery population.
It is important for the caregiver to
distinguish such ephemeral lesions from
significant life-threatening diseases with
cutaneous manifestations.
12.
13.
14. HARLEQUIN COLOR CHANGE
• Harlequin color change is a phenomenon observedin the immediate neonatal period and is more
common in the infant with low birthweight. The
dependent side of the body becomes intensely red
and the upper side pales, with a sharp midline
demarcation. The peak incidence of attacks in one
series occurred on the second, third, and fourth
days, but episodes were observed during the first 3
weeks of life.
• These episodes are of no pathologic significance.
They have been attributed to a temporary imbalance
in the autonomic regulatory mechanism of the
cutaneous vessels; there are no accompanying
changes in the respiratory rate, muscle tone, or
response to external stimuli.
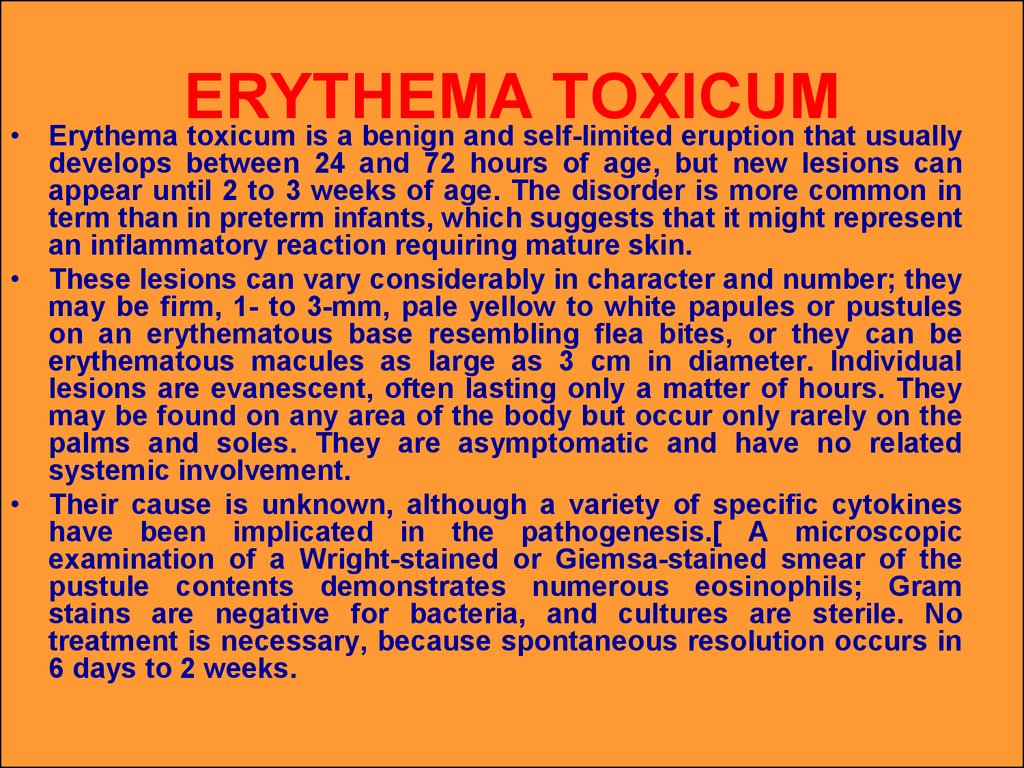
15. ERYTHEMA TOXICUM
ERYTHEMA
TOXICUM
Erythema toxicum is a benign and self-limited eruption that usually
develops between 24 and 72 hours of age, but new lesions can
appear until 2 to 3 weeks of age. The disorder is more common in
term than in preterm infants, which suggests that it might represent
an inflammatory reaction requiring mature skin.
• These lesions can vary considerably in character and number; they
may be firm, 1- to 3-mm, pale yellow to white papules or pustules
on an erythematous base resembling flea bites, or they can be
erythematous macules as large as 3 cm in diameter. Individual
lesions are evanescent, often lasting only a matter of hours. They
may be found on any area of the body but occur only rarely on the
palms and soles. They are asymptomatic and have no related
systemic involvement.
• Their cause is unknown, although a variety of specific cytokines
have been implicated in the pathogenesis.[ A microscopic
examination of a Wright-stained or Giemsa-stained smear of the
pustule contents demonstrates numerous eosinophils; Gram
stains are negative for bacteria, and cultures are sterile. No
treatment is necessary, because spontaneous resolution occurs in
6 days to 2 weeks.
16.
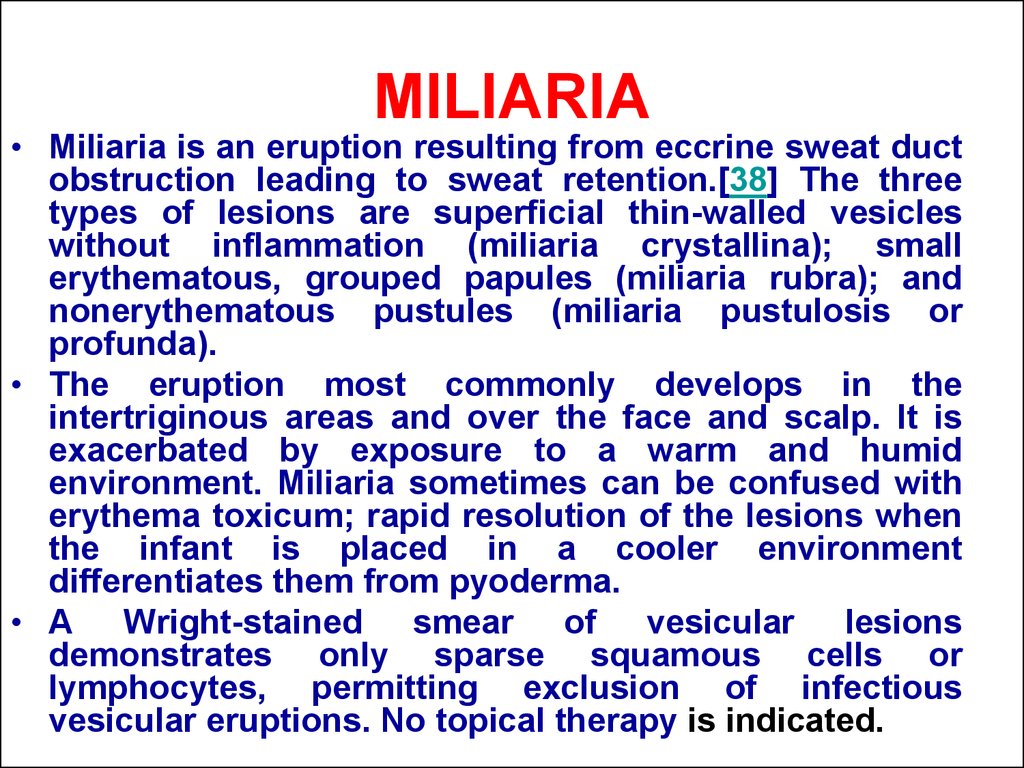
17. MILIARIA
• Miliaria is an eruption resulting from eccrine sweat ductobstruction leading to sweat retention.[38] The three
types of lesions are superficial thin-walled vesicles
without inflammation (miliaria crystallina); small
erythematous, grouped papules (miliaria rubra); and
nonerythematous pustules (miliaria pustulosis or
profunda).
• The eruption most commonly develops in the
intertriginous areas and over the face and scalp. It is
exacerbated by exposure to a warm and humid
environment. Miliaria sometimes can be confused with
erythema toxicum; rapid resolution of the lesions when
the infant is placed in a cooler environment
differentiates them from pyoderma.
• A Wright-stained smear of vesicular lesions
demonstrates only sparse squamous cells or
lymphocytes, permitting exclusion of infectious
vesicular eruptions. No topical therapy is indicated.
 medicine
medicine