Similar presentations:
Arrhythmias. Сlassification
1.
Arrhythmiasm a d e by: Koshanov Alibi
2.
ArrhythmiasHeart rhythm disorders (arrhythmias) are changes in the normal
frequency, regularity a n d source of cardiac excitation, as well as
disorders of conduction impulse, communication and/or
sequencing disorders between the activation of the
of the atria a n d ventricles.
3.
СlassificationIn a c c o r d a n c e with the mechanism of arrhythmias, all heart rhythm disorders
c a n b e conditionally subdivided into three types:
1) disorders of automaticity;
2) disorders of excitability;
3)conduction disorders. Such a division in a certain sense
conditional, because in reality it is often encountered arrhythmias
of a combined character.
For example, in ventricular a n d atrial fibrillation, both excitability a n d
conduction disorders may b e present.
4.
1.Disorders of automaticityCardiac automaticity disorders are arrhythmias caused by disturbances in the
electrophysiologic activity of the cardiac pacemakers (sinus and sinus rhythm
drivers).
These arrhythmias include:
sinus bradycardia
sinus tachycardia
sinus arrhythmia
atrioventricular tachycardia
nodal rhythm
idioventricular rhythm.
5.
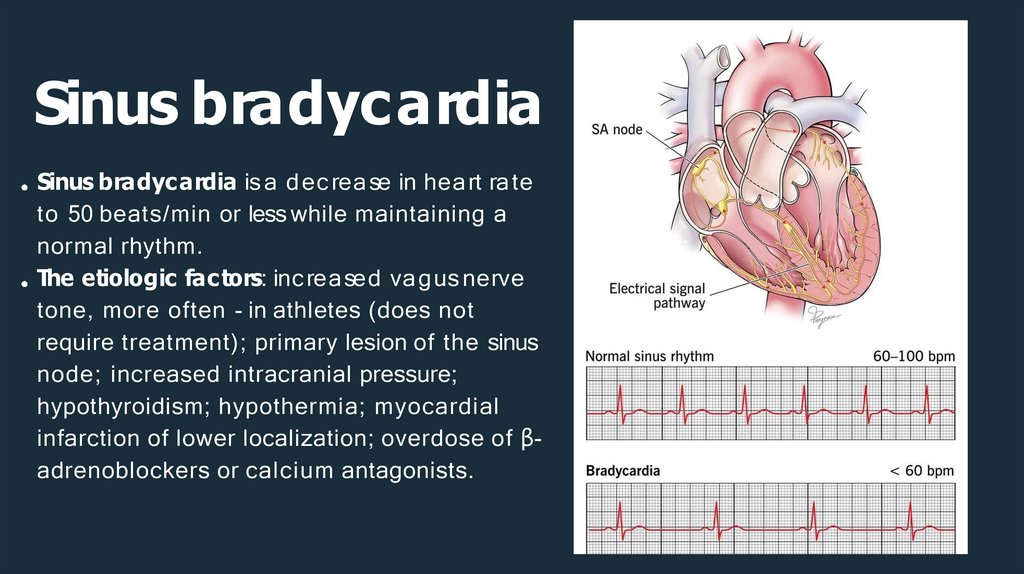
Sinus bradycardiaSinus bradyc ardia is a d ec rea se in hea rt ra te
to 50 beats/min or less while maintaining a
normal rhythm.
The etiologic fac tors: inc rea sed va g us nerve
tone, more often - in athletes (does not
require treatment); primary lesion of the sinus
node; increased intracranial pressure;
hypothyroidism; hypothermia; myocardial
infarction of lower localization; overdose of βadrenoblockers or calcium antagonists.
6.
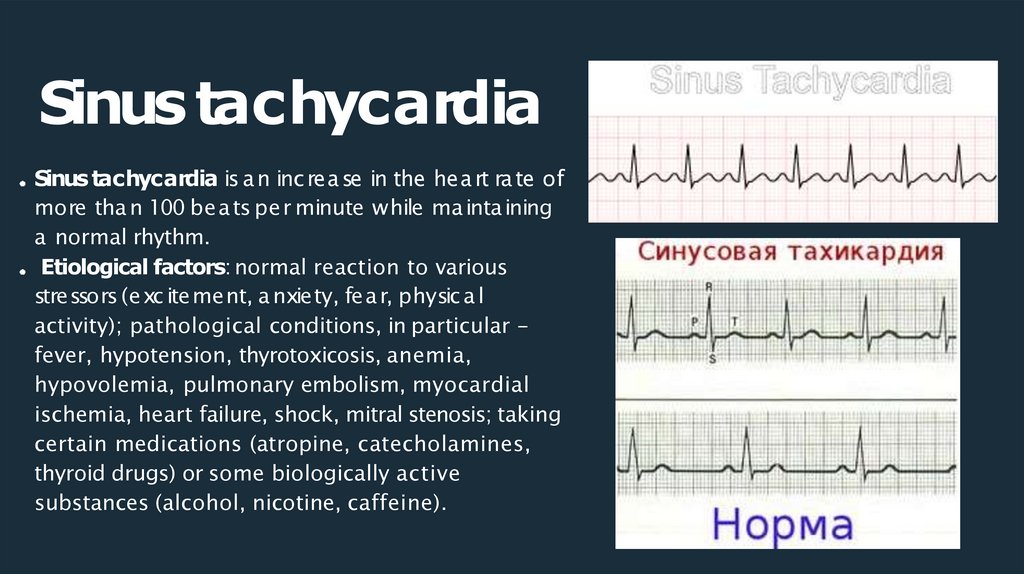
Sinus tachycardiaSinus tachycardia is a n inc rea se in the hea rt ra te of
more tha n 100 bea ts per minute while ma inta ining
a normal rhythm.
Etiological factors: normal reaction to various
stressors (exc itement, a nxiety, fea r, physic a l
activity); pathological conditions, in particular fever, hypotension, thyrotoxicosis, anemia,
hypovolemia, pulmonary embolism, myocardial
ischemia, heart failure, shock, mitral stenosis; taking
certain medications (atropine, catecholamines,
thyroid drugs) or some biologically active
substances (alcohol, nicotine, caffeine).
7.
2. Disorders of the excitability of the heartDisorders of the excitability of the heart are the basis of such types of
arrhythmias as
extrasystoles,
ventricular tachycardia,
polymorphic ventricular tachycardia,
ventricular and atrial flutter,
ventricular and atrial fibrillation,
8.
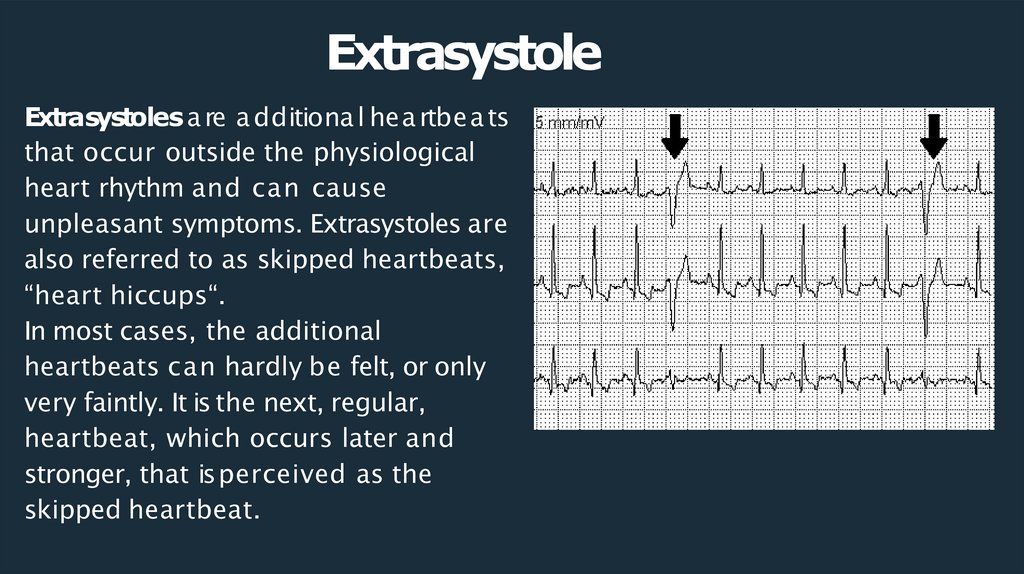
ExtrasystoleExtrasystoles a re a dditiona l hea rtbea ts
that occur outside the physiological
heart rhythm and can cause
unpleasant symptoms. Extrasystoles are
also referred to as skipped heartbeats,
“heart hiccups“.
In most cases, the additional
heartbeats can hardly be felt, or only
very faintly. It is the next, regular,
heartbeat, which occurs later and
stronger, that is perceived as the
skipped heartbeat.
9.
Ventricular extrasystoleVentricular extrasystoles are premature ventricular contractions caused by the presence of a focus
of automatism in the ventricles.
Etiological factors of ventricular extrasystoles: Coronary heart disease, cardiomyopathy, electrolyte
and acid-base balance disorders, hypoxia, thyrotoxicosis, antiarrhythmics
On an ECG: premature QRS complexes that differ from normal complexes with a width of more than
0.12 s, deformation, and the presence of a previous shortened R-R interval. The Twave is enlarged,
ST segment, is discordant, i.e. directed in the other direction. Clinically, ventricular extrasystoles
manifest as a feeling of palpitation or discomfort in the chest, a feeling of heart failure
10.
Atrial fibrillationAtrial fibrillation is the a bsenc e of c oordina ted a tria l
contractions, which is electrocardiographically
characterized by the isappearance of the P wave.
Atrial fibrillation leads to the cessation of
hemodynamically effective atrial contractions. It is
manifested by irregular small atrial oscillations of
various amplitudes and shapes with a frequency of
350-600 per minute, which cannot be registered on a
conventional electrocardiograph
Etiological factors: atherosclerosis, hypotension,
cardiomyopathy and rheumatic heart disease,
thyrotoxicosis
11.
Atrial flutterAtrial flutter is a violation of the processes of excitation and conduction in the atria, which
electrocardiographic is characterized by the disappearance of the P wave and the appearance
instead of it of frequent low-amplitude osc illations, the so
-called F waves, which got their name from the English word flutter - oscillation. The frequency of
atrial contractions is more than 220 V min, and ventricles - 120-180 in min. QRS complexes are normal
There are tachy-, normo- and bradysystolic forms of atrial flutter.
The etiological factors are the same as in atrial fibrillation.
12.
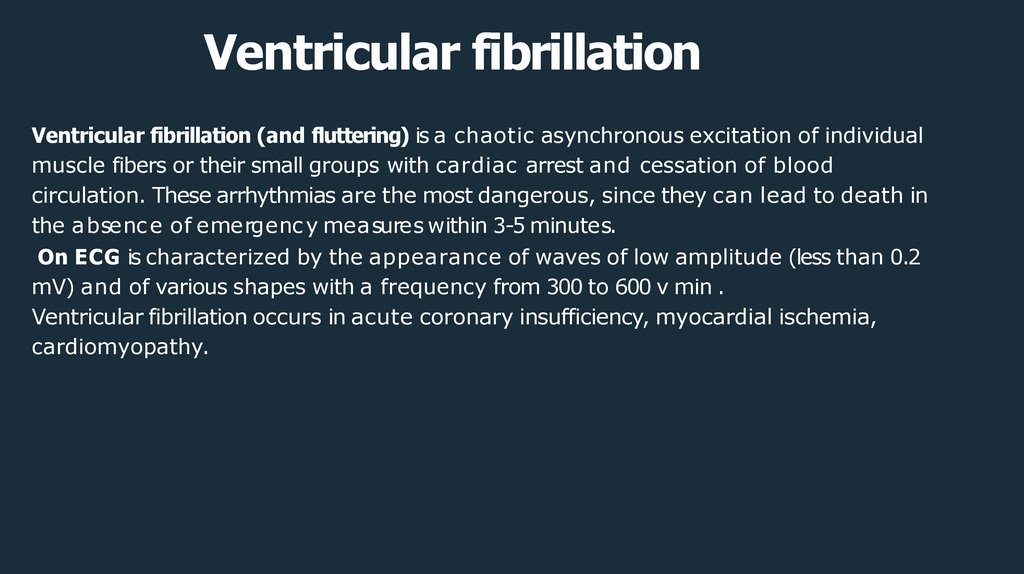
Ventricular fibrillationVentricular fibrillation (and fluttering) is a chaotic asynchronous excitation of individual
muscle fibers or their small groups with cardiac arrest and cessation of blood
circulation. These arrhythmias are the most dangerous, since they can lead to death in
the absenc e of emergenc y measures within 3-5 minutes.
On ECG is characterized by the appearance of waves of low amplitude (less than 0.2
mV) and of various shapes with a frequency from 300 to 600 v min .
Ventricular fibrillation occurs in acute coronary insufficiency, myocardial ischemia,
cardiomyopathy.
13.
14.
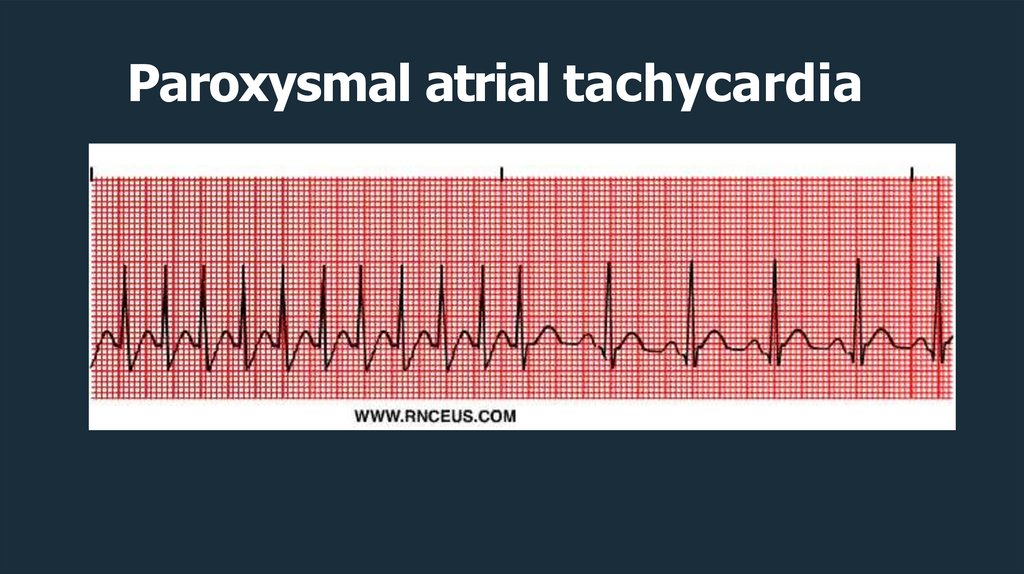
Paroxysmal atrial tachycardiaParoxysmal supraventricular tachycardia (PSVT) is a type of atrial arrhythmia. It
happens when there is abnormal electrical activity in the atria. This is caused by
an abnormally irritable area in the atria or by a short circuit in your heart causing
electrical signals to travel around and around in a circular pattern. This causes
the atria to contract quickly over and over again.
Causes
Anemia.
Ingesting drinks and foods that contain caffeine.
Drugs such as nasal decongestants
Heart attac k
hypertension
15.
Paroxysmal atrial tachycardia16.
3. Disorder of conductionC onduc tion disorders inc lude
transverse heart bloc k,
blockage of the right and/or left legs of the His bundle,
Wolf-Parkinson-White syndrome.
17.
Transverse blockadeTransverse blockade is a violation of the excitation in the
area of the atrioventricular node. Transverse blockade of
the heart, in turn, is divided into bloc kade I, II, IIIand IV
degrees. The first three degrees are also called
inc omplete, and the last one is c alled c omplete
transverse heart bloc k.
18.
Transverse blockade of the 1st degreeTransverse bloc kade of the Idegree is manifested by a
delay in the c onduc tion of the pulse in the
atrioventricular node. Electrocardiographically, it is
c harac terized by an elongation of the P-Q interval.
19.
Transverse blockade of the 2 degreeGrade IItransverse blockade is characterized by the fact that
in the structure of each subsequent ECG cycle, the PQ
interval lengthens more and more until one ventricular
complex falls out (Samoilov Wenkebach periods), after which
the duration of the P-Q interval returns to normal, but
immediately begins to lengthen again. Thus, the process is
cyclical
20.
Transverse blockade of the 2 degree21.
Transverse blockade of the 3 degreeTransverse blockade of the III degree is expressed in the fact
that only every second or third pulse passes through the
atrioventricular node from the atria to the ventricles.
The heart rate is significantly reduced, so serious
hemodynamic disorders may occur
22.
Transverse blockade of the 3 degree23.
Wolf-Parkinson-White syndromeWolf-Parkinson-White syndrome . The heart muscle contracts at such a fast
rate that it has very little time to relax and fill with blood inbetween
contractions
There are three main electrocardiographic signs of WPW syndrome:
a) the P-R interval is shortened against the background of a sinus rhythm;
b) the QRS complex is "stretched" beyond the norm with a flat initial part;
c)secondary ST segment changes in which the Twave is discordant (in the
opposite direction) with respect to the QRS complex.
24.
Wolf-Parkinson-White syndrome25.
Management and TreatmentAntiarrhythmic drugs that convert the arrhythmia to sinus rhythm (normal
rhythm) or prevent an arrhythmia.
Medicines that control your heart rate.
Anticoagulant or antiplatelet therapy drugs (such as warfarin or aspirin) that
reduc e the risk of blood c lots forming.
Medications that treat related conditions that may be causing an abnormal
heart rhythm.
















 medicine
medicine








