Similar presentations:
Best Practices: Treating Hypothermic Patients
1. Best Practices: Treating Hypothermic Patients
2.
• When the temperature plummets, hypothermia becomes adanger.
• Hypothermia is a medical emergency in which the body's
mechanism for temperature regulation is overwhelmed by
a cold stressor.
• The body loses heat faster than it can produce heat,
resulting in a dangerously low core body temperature of
less than 35°C and impairing the functioning of the body’s
organ systems.
• If the body temperature continues to fall, organs begin to
fail, and eventually death will occur.
• Many patients have recovered from severe hypothermia, so
early recognition and prompt initiation of optimal
treatment are critically important.
[Edelstein JA. Hypothermia: Medscape Reference. Available at: http://emedicine.medscape.com/article/770542-overview. Accessed December 11,
2012. ]
3.
• The rate of hypothermia-related deaths in the U.S. increases with age (shownper 100,000 population; data from 2001).
A patient’s degree of hypothermia is defined by his/her core body temperature:
– mild hypothermia (32°C-35°C),
– moderate hypothermia (28°C-32°C),
– severe hypothermia (less than 28°C).
• Primary hypothermia results from
exposure to cold, which overwhelms
the body’s compensatory
mechanisms to maintain physiologic
temperature.
• Secondary hypothermia has
multiple causes (typically metabolic),
including:
–
–
–
–
sepsis,
hypothyroidism,
burns, and
hypothalamic disorders.
4.
5.
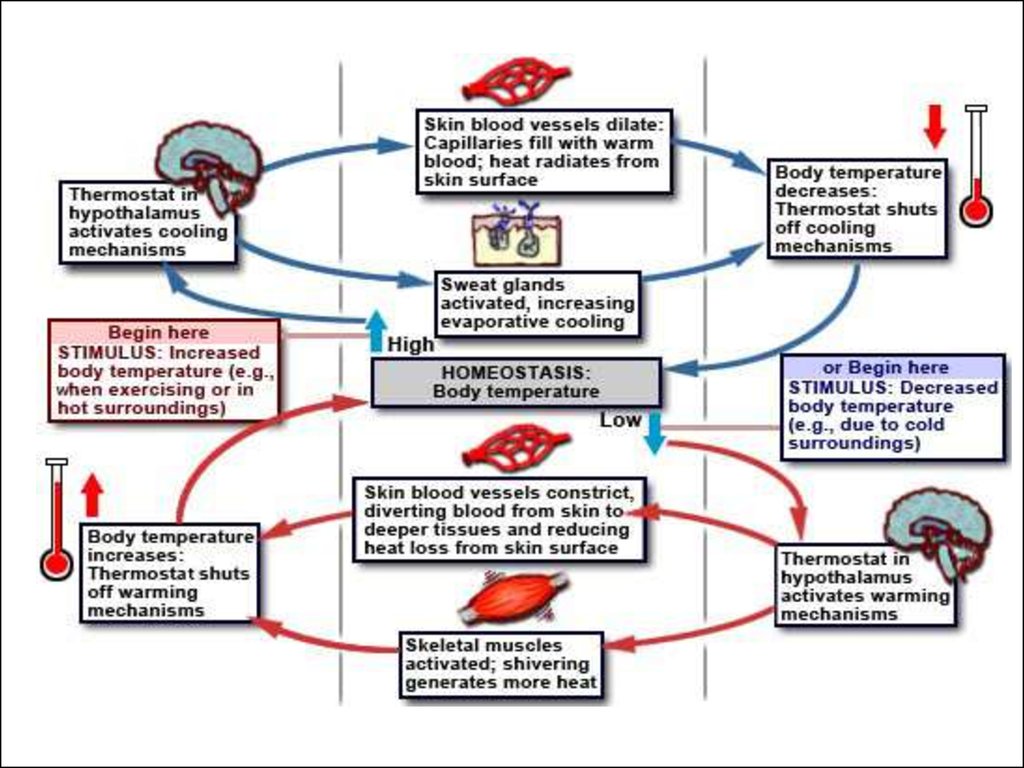
• Under normal conditions, body temperature is tightlyregulated by balancing heat production and dissipation.
• Basal metabolic rate has multiple regulators including the
hypothalamus, thyroid, and sympathetic nervous system.
• Heat dissipation occurs via:
– radiation (55-65%; due to the gradient between the
environment and exposed body area),
– evaporation (20-35%; results from the process of
breathing),
– convection (10-15%; due to wind), and
– conduction (2-3%; results from a person’s direct contact
with cold substances).
• Heat dissipation via conduction occurs 5 times faster
in wet clothing and 25 times faster in cold water.
6.
• The clinical presentation of hypothermia dependsupon the patient’s core temperature.
• In mild hypothermia, patients present with
– shivering (increases metabolic rate and heat production),
– slurred speech,
– loss of coordination, and
– tachycardia.
• In moderate hypothermia, patients present with
– somnolence,
– declining respiratory rate and heart rate,
– loss of shivering, and
– declining metabolic rate.
7.
• In severe hypothermia, patients present– in a coma, with apnea,
– fibrillation progressing to asystole, and
– limited or no cranial nerve reflexes.
• In moderate and severe hypothermia, the
body no longer actively
produces heat and
active rewarming
is required.
8.
• Hypothermia impairs the functioning of the body’sorgan systems.
• The central nervous system response to hypothermia
initially involves sympathetic activation as part of the
compensatory mechanism.
• However, as hypothermia progresses, cerebral
metabolic rate declines 6% for each 1°C drop in
temperature.
• Temperatures of less than 30°C typically impair
consciousness, and those of less than 25°C impair
cerebral autoregulation.
• Renal consequences of hypothermia include cold
diuresis.
9.
• Peripheral vasoconstriction shunts blood tothe core, producing a relative increase in
preglomerular pressure.
• This reduces sodium and water reabsorption,
leading to diuresis.
10.
• A middle-aged man is found lying on the street in the snowin front of his home. He has a right ankle deformity and
smells of alcohol, but displays no other outward signs of
trauma. Vital signs reveal a rectal temperature of 28°C, pulse
of 40, pulse oxygenation 95% RA, respiratory rate of 12, and
blood pressure of 108/56. Glasgow Coma Score (GCS) is 3.
Pupils are dilated at 5 mm and are poorly responsive. Aside
from immediate rewarming and cervical collar placement,
what initial interventions should be used?
A. Rapid blood glucose determination
B. Trial of naloxone
C. Trial of flumazenil
D. Both rapid blood glucose determination and trial of
naloxone
E. All of the above
11.
12.
• This patient clearly has hypothermia, as evidenced by hisrectal temperature.
• All patients with altered mental status should have an
assessment of blood glucose level as a component of their
initial evaluation.
• In this case, a trial of naloxone should be administered
because opiate overdose is a possibility. (Note, however, that
pupillary dilatation is often observed in patients with
temperatures of less than 30°C, in the absence of opiate
overdose.)
• Many patients become hypothermic after becoming
intoxicated.
• In the setting of prolonged benzodiazepine use,
administering flumazenil could precipitate seizures or
withdrawal.
13.
• An electrocardiogram (ECG) is obtained on our patient (shown),revealing sinus bradycardia with a rate in the low 40s. Given our
patient’s initial temperature, which of the following cardiac
dysrhythmias is he at risk for developing?
A. Torsades de pointes
B. Ventricular fibrillation
C. Atrial fibrillation
D. Multifocal atrial tachycardia
E. Monomorphic ventricular tachycardia
14.
• The initial cardiovascular response to hypothermia is tachycardia as acomponent of increased metabolic rate, and in response to the demand
from shivering metabolically active muscle tissue.
• However, as hypothermia progresses, the heart rate becomes more
bradycardic. Bradycardia is typically resistant to atropine administration.
• Atrioventricular blocks can emerge and heart muscle tissue becomes, in
general, more susceptible to fibrillation.
• Atrial fibrillation may be seen in patients with temperatures less than
32°C, but ventricular fibrillation (shown) becomes more common with
temperatures less than 28°C.
15.
• Several ECG findings are associated with hypothermia(shown).• Muscle tremor artifact may be present and may be mistaken
for ventricular dysrhythmias.
• Initial changes may include prolongation of intervals as well as
T wave inversion.
• The Osborne J wave is often noted when the temperature
declines to below 33°C. The amplitude of the J wave is
proportional to the degree of hypothermia and is typically
best seen in V3-V6. It is thought to result from abnormal
depolarization and repolarization of ventricular tissue.
16.
• The definitive treatment for hypothermia is rewarming ofthe patient.
• Rewarming approaches are categorized as “passive
external,” “active external,” or “active internal”
17.
• Passive external rewarming focuses onreducing heat loss and allowing normal
physiologic compensatory mechanisms to
arrest the temperature decline. This approach
(when used in isolation) is indicated only for
mild hypothermia when shivering and other
compensatory measures are effective.
• Passive external rewarming includes removing
the patient from the cold environment (e.g.,
removing wet clothes) and providing a blanket
or warm clothes.
• The rewarming rate is 0.5°C-2.0°C/hour.
18.
• Active external rewarming methods typically involveproviding heat to body surfaces.
• As such, severe peripheral vasoconstriction may limit the
initial effectiveness of active external approaches.
• Methods include:
– heating blankets,
– forced air blankets,
– radiant warmers,
– heating pads, and
– warm bath immersion.
• Warm bath immersion may be the most effective means for
raising temperature, but concerns including rapid
vasoconstriction, as well as the inability to monitor,
defibrillate, and control the rate of rewarming limit its utility.
19.
20.
• With peripheral warming and vasodilation, coolerblood may circulate to the core, resulting in an initial
temperature drop, known as the afterdrop
phenomenon.
• A hypothermic patient is rapidly rewarmed using active
external approaches.
• In the absence of alcohol, most hypothermic patients
are peripherally vasoconstricted.
• As active external rewarming is commenced,
vasodilation in the cold extremities may cause cold
blood to return to the core, thereby initially decreasing
core body temperature.
• Very few studies have found core afterdrop to be
clinically significant.
21.
22.
• Active internal rewarming methods aim to directly increase coretemperature and are divided into
• noninvasive approaches (warmed humidified oxygen, warmed IV
fluids) and
• invasive approaches:
–
–
–
–
pericardial/thoracic/GI/bladder lavage,
extracorporeal membrane oxygenation [ECMO],
arteriovenous dialysis,
endovascular rewarming with a catheter that circulates warmed fluids,
and
– cardiopulmonary bypass).
• Warmed inspired gases, warmed IV fluids, and gastric or
peritoneal lavage can raise the temperature about 3°C/hour.
• Rapid active internal rewarming methods such as thoracic lavage
(6°C/hour), ECMO (7°C/hour), and cardiopulmonary bypass
(18°C/hour) are typically used on patients with severe
hypothermia.
23.
24.
• Aggressive resuscitation efforts are generally indicated,even in the presence of cardiac dysrhythmia or cardiac
arrest.
• Clinicians are concerned that endotracheal intubation will
precipitate malignant ventricular dysrhythmias, but this has
not been borne out by the literature.
• Intubation should not be withheld for this fear.
• For patients with a temperature below 30°C, advanced
cardiac life support (ACLS) medications are not indicated
because their metabolism is incomplete and excessive
dosing may lead to toxic accumulation.
• If core body temperature is below 30°C, one defibrillatory
shock should be attempted and resuscitation should then
be used to a temperature above 30°C.























 medicine
medicine








