Similar presentations:
Investigation of the gastrointestinal tract (GIT)
1. Investigation of the gastrointestinal tract (GIT)
2. Oral contrast investigation
Barium sulphate is the best contrast medium for thegastrointestinal tract.
its atomic number is high
it produces excellent opacification
good coating of the mucosa
non-absorbable
non-toxic
it is completely inert
3. Limitations
causes chemical peritonitis whenextravasates into the peritoneal cavity, hence
it is not used in suspected perforation of
stomach and intestine
extravasation into bronchial tree will cause
inflammation and granuloma formation
barium inspissations in case of colonic
obstruction hard stones
4. Single and double contrast studies are done with barium
In single contrast method bowel is filed onlywith barium.
In double contrast, the mucosa is coated with
barium and introduction of gas distends the
lumen of the bowel. Double contrast method
demonstrates mucosal irregularities which
are obscured in single contrast.
5. Gastrograffin
Other available oral contrast for GIT isgastrograffin, which is a water soluble
contrast medium, which does not cause
chemical peritonitis or colonic obstruction.
The principal value of water soluble contrast
media is to demonstrate leaks from the
bowel and outlining fistulous tracts as they
are safe in perforation cases.
6. Barium swallow
It is the contrast study of the swallowingmechanism and passage of food bolus from
mouth up to the fundus of the stomach
7. Barium examinations of the oesophagus
Indications:dysphagia (causes: corrosive strictures,
carcinoma and achalasia)
motility disorders of oesophagus
pharingo-oesophageal malignancies
pharyngeal diverticula
webs
8. Contraindications:
tracheo-oesophageal fistulaperforation
because the barium should not pass into the
respirator passage.
Therefore, to diagnose these conditions
water soluble non-ionic contrast media such
as omnipaque, ultravist are used.
9. Procedure
The patient drinks some barium and itspassage down the oesophagus is observed
on a television monitor. Films are taken with
the oesophagus both full of barium to show
the outline, and following the passage of the
barium to show mucosal pattern (films are
taken in filling phase and empty phase).
Films are taken in frontal and lateral
projections during the process of swallowing.
10. The flow of barium is noted fluoroscopically through the:
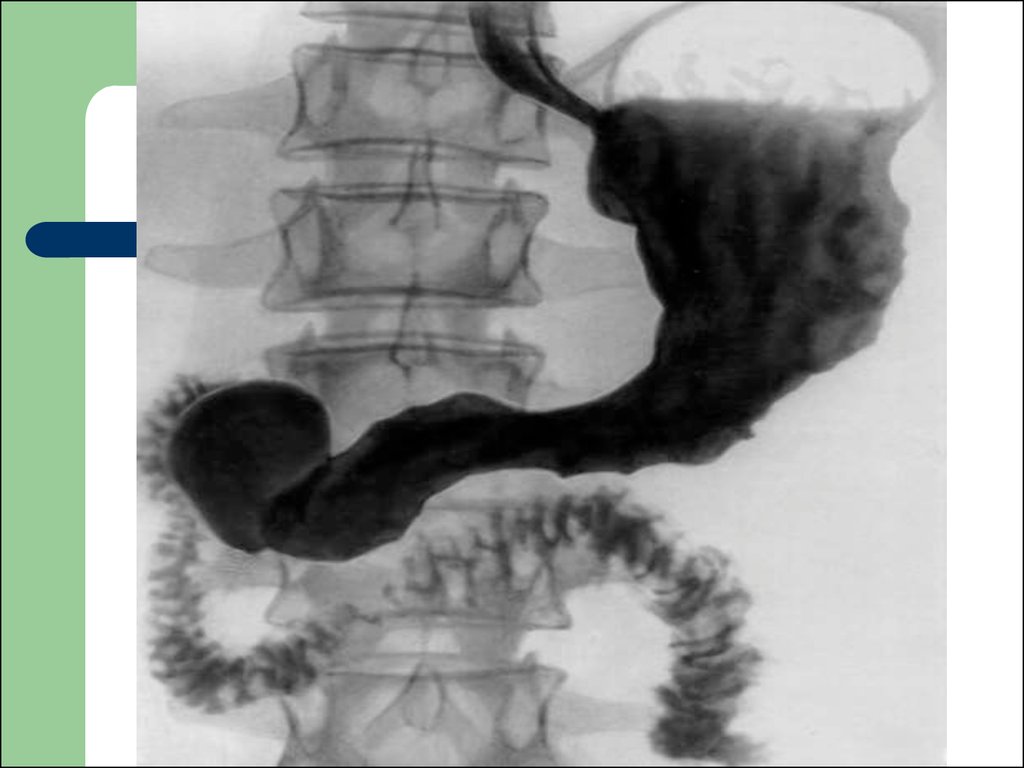
pharynxcervical oesophagus
epiphrenic oesophagus
gastro-oesophageal junction
11. Anatomy of oesophagus
The oesophagus commences at the level ofcricopharyngeus and ends at the cardia. It is
approximately 25 cm in length, the majority
of this being in the thorax, with short cervical
and intra-abdominal segments. The gastrooesophageal junction is usually found at a
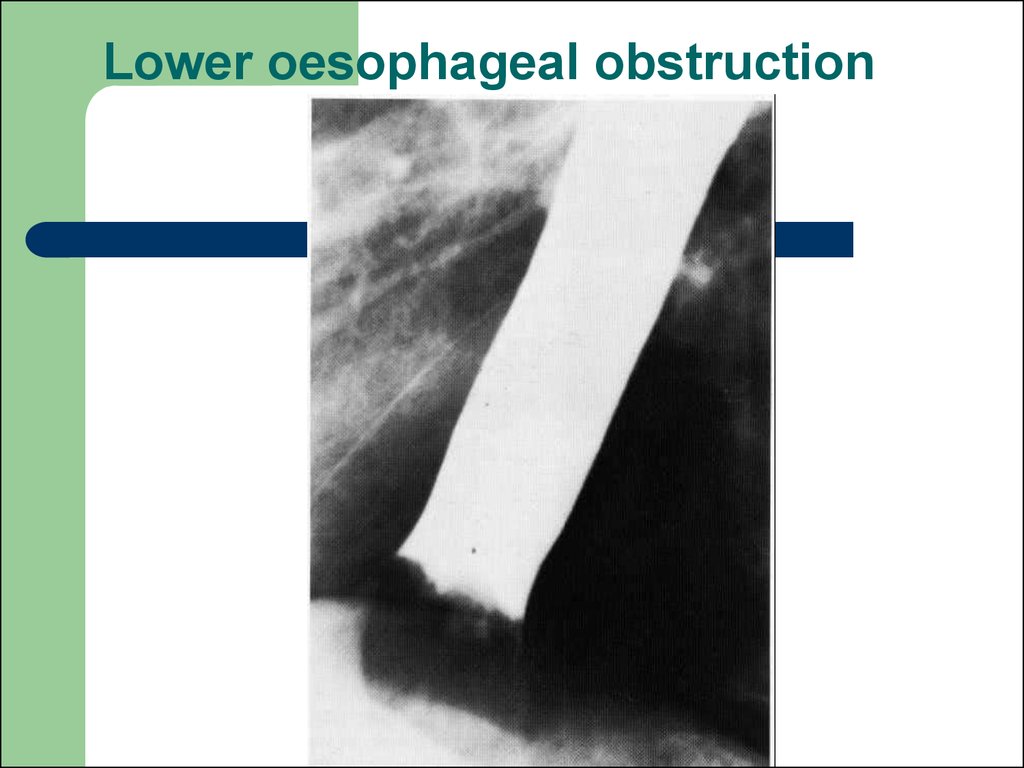
surprisingly constant 40 cm distance from the
incisor teeth.
12.
The oesophagus when full of barium shouldhave a smooth outline. When empty and
contracted, barium normally lies in between
the folds of mucosa which appear as three or
four long, straight parallel lines.
13.
The aortic arch gives a clearly visible impression onthe left side of the oesophagus, which is more
pronounced in the elderly as the aorta becomes
tortuous and elongated.
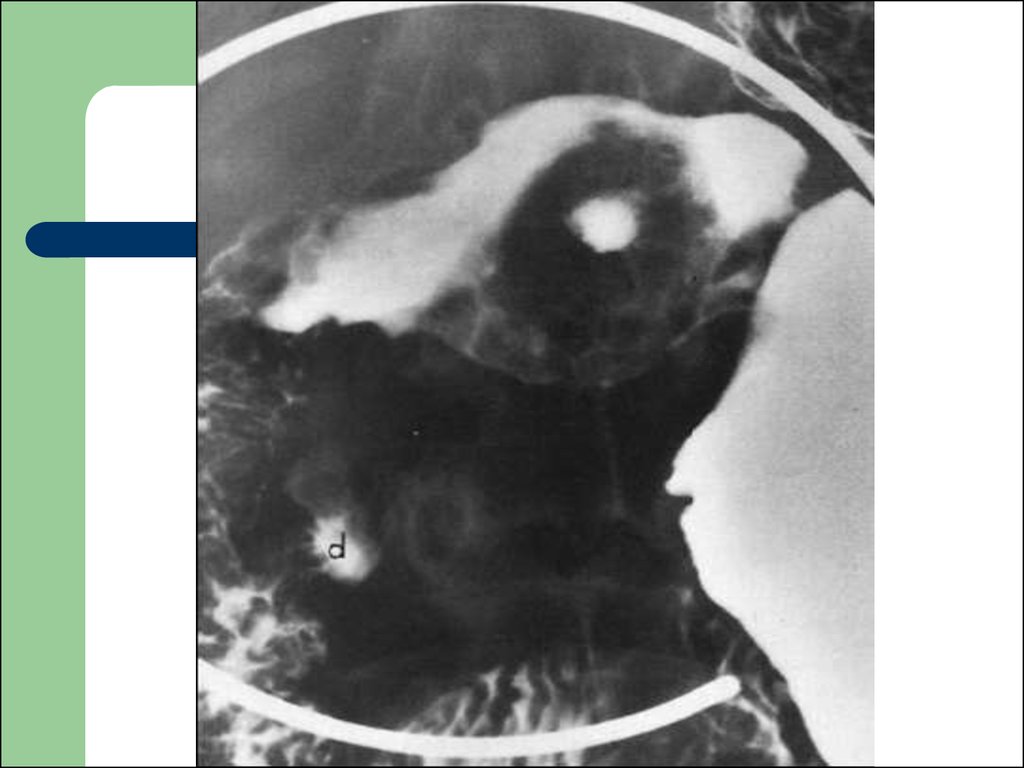
Below the aortic impression there is often a smaller
impression made by the left main bronchus.
The lower part of the oesophagus sweeps gently
forward closely applied to the back of the left atrium
and left ventricle.
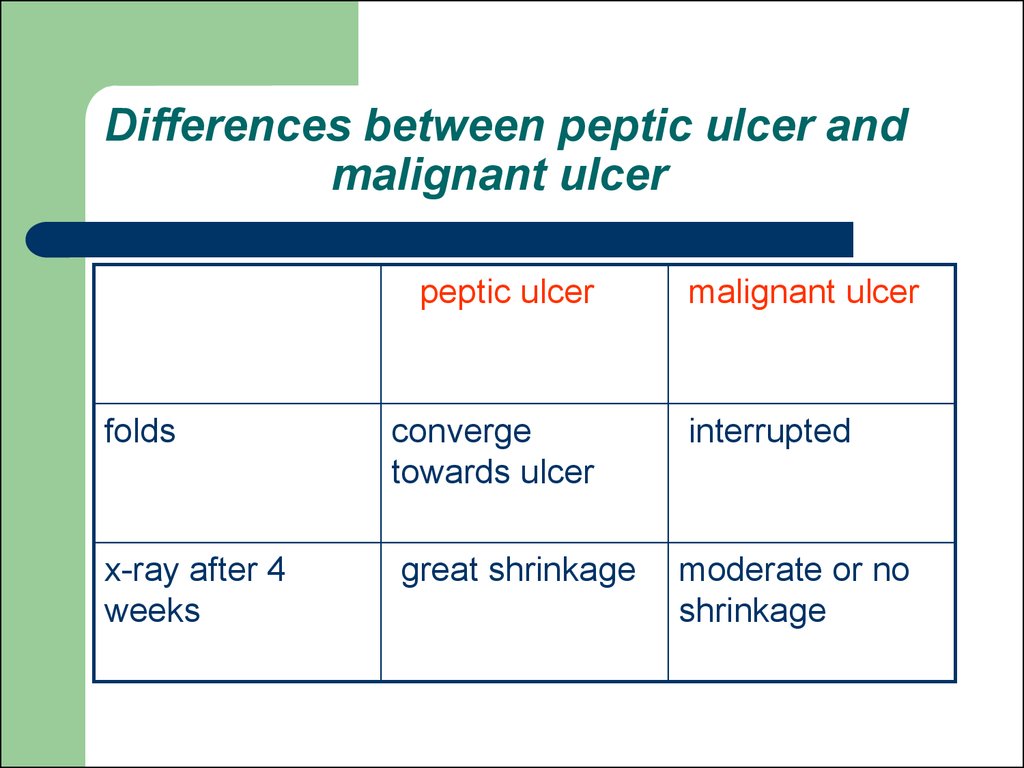
14.
Peristaltic waves can be observed duringfluoroscopy. They move smoothly along the
oesophagus to propel the barium rapidly into
the stomach. It is important not to confuse a
contraction wave with a true narrowing: a
narrowing is constant whereas a contraction
wave is transitory.
15.
16.
17.
18. Upper esophageal sphincter
19. Barium examinations of the stomach
It is a radiological study of the stomach,duodenum and proximal jejunum. It is done
by oral administration of barium.
20. Indications:
suspected malignancies of gastroesophageal junction, stomach andduodenum
gastric or duodenal obstructive lesions
gastric or duodenal ulcers
motility disorders
congenital anomalies
21. Contraindications:
suspected gastro-duodenal perforationlarge bowel obstruction
recent biopsy from GIT.
22. Procedure
The patient fasts for at least 6 hours to theexamination. Single and double contrast
studies are performed after the patient
swallows around 250 ml of barium
suspension. Air is used to produce double
contrast effect. Films are taken in various
positions with the patient both erect and lying
flat, so that each part of the stomach and
duodenum is seen.
23. Anatomy of the stomach and duodenum
The stomach has a complex shape andvaries considerably depending on the degree
of distention.
Each part of the stomach and duodenum
should be checked to ensure that no
abnormal narrowing is present. A transient
contraction wave must not be confused with
a constant pathological narrowing.
24.
The duodenal cap or bulb should beapproximately triangular in shape. It arises
just beyond the short pyloric canal and may
be difficult to recognize if deformed from
chronic ulceration.
The duodenum forms a loop around the
heard of the pancreas to reach
duodenojejunal flexure.
25.
26.
27.
28.
The outline of the lesser curve of thestomach is smooth with no filling defects or
projections visible but the greater curve is
nearly always irregular due to prominent
mucosal folds. In the stomach the mucosa is
thrown up into a number of smooth folds and
barium collects in the troughs between the
folds.
The duodenum is attached to the stomach at
the narrow pylorus and consists of the
duodenal bulb and the descending and
ascending portions, although a horizontal
segment is often added.
29.
The duodenal cap or bulb should beapproximately triangular in shape. It arises
just beyond the short pyloric canal and may
be difficult to recognize if deformed from
chronic ulceration.
The duodenum forms a loop around the
heard of the pancreas to reach
duodenojejunal flexure.
30.
31. Causes of gastric displacement
enlargement of spleen causes forward andmedial displacement of stomach
enlargement of left kidney usually displaces
the stomach forward
enlargement of left lobe of liver causes
backward displacement of fundus of body
tumors of body and tail of pancreas push
stomach forward
32. Examinations of the Small Intestine
The radiographic examination of the small bowelevaluates the mesenteric portion of the organ, which
consists of the jejunum and ileum.
The following luminal contrast methods can be
used to examine the small intestine:
* peroral small-bowel series;
* enteroclysis;
* various retrograde techniques (e.g., via an
ileostomy).
33.
However, the peroral small bowel study isprobably the least effective method of
examining this organ; techniques that better
distend the small bowel with higher volume
are now preferred depending on the
indications.
These include enteroclysis and CT or MR
imaging with volume instillation by oral
ingestion or via a tube, that is, CT or MR
enterography or CT or MR enteroclysis.
34.
Enteroclysis is an intubated examination of thesmall intestine and can be done by a variety of
techniques and using a number of different
modalities. The small intestine is intubated by a
nasal or oral route with a small-bore enteric tube
placed with fluoroscopic guidance. A variety of
luminal contrast methods exist, but filming is done
similarly to the peroral examination. The enteroclysis
techniques permit better control of small-bowel
distention and more exact visualization of smallbowel loops.
35.
Retrograde examination of the small bowelinvolves filling of the organ from the opposite
direction. Various techniques can be used
depending on the patient’s anatomy. Reflux
of the small intestine through the ileocecal
valve can be done as part of a barium
enema. If the patient has an ileostomy,
various devices can be introduced into the
ileostomy site and a barium suspension
instilled directly.
36. Anatomy of the small intestine
The length of the mesenteric small bowel in adultsaverages about 20 feet, but varies considerably
among individuals.
The jejunum comprises just over one-third of the
length and the ileum the remainder, although no
discrete transition is seen between the two
segments. The normally distended small bowel has
a caliber of 2 to 3 cm, being slightly larger more orad
in the jejunum.
37.
Depending on the degree of distention, themucosal folds (valvulae conniventes) may
have a feathery appearance or may be
transversely oriented across the intestinal
lumen with more complete distention. The
mucosal folds are more numerous in the
jejunum and gradually decrease in number
and size in the ileum.
38. peroral small bowel study
39. Enteroclysis
40. Examinations of the Large Intestine
The radiographic examination of the largebowel evaluates the entire organ from the
rectum to the caecum. Reflux of barium
suspension into the ileum and the appendix,
if present, occurs commonly.
The colon can be evaluated by several
techniques, which include single-contrast
and double contrast barium enemas.
41.
The single-contrast method simply involvesfilling the colon with a dilute barium
suspension, whereas the double-contrast
technique requires a denser, more viscous
barium suspension and air.
In both methods, large and small
compression images of all segments of the
colon are obtained.
42. Indications
change in bowel habithemorrhage
investigation of an abdominal mass
location of the site of large-bowel obstruction
43. Contraindication
toxic megacolonpseudomembranous colitis
recent radiotherapy
full thickness bowel wall biopsy
44. Anatomy of the large intestine
The large intestine consists of the rectum, sigmoidcolon, descending colon, splenic flexure, transverse
colon, hepatic flexure, ascending colon, and
caecum.
The length of the colon varies considerably, mainly
because of differences in length and redundancy of
the sigmoid colon and colic flexures. The colon also
varies in caliber depending on location and luminal
distention achieved.
45.
The mucosal surface has a smoothappearance, and the colonic contour is
indented by the haustra, which are less
numerous in the descending colon. The
rectal valves of Houston are often seen,
especially on double-contrast imaging.
The ileocecal valve has a variety of
appearances and may be large if infiltrated
by fat.
46.
47.
48. Computed Tomography (CT) Scanning
Uses in the gastrointestinal tract include:Staging of tumors for secondary deposits
and adjacent infiltration
Localizing abscess
As an aid to biopsy and drainage procedures
49.
50.
51.
52. Magnetic Resonance Imaging
MRI imaging of the hollow organs of thegastrointestinal tract is increasingly being
used to evaluate a wide assortment of
gastrointestinal tract disorders. As with CT
imaging, mild mucosal diseases and small
focal lesions are not well detected with this
technique; however, malignancies can be
similarly evaluated and staged.
53.
Also, with the use of luminal distention andintravenous agents of various types,
assessment of obstructive and inflammatory
bowel disease has shown dramatic results.
Small-bowel obstruction and Crohn’s disease
in particular have become common
indications for use of MR imaging.
54.
55. Isotope scanning
Technetium-99 pertechnetate may be usedfor studies of:
gastric emptying
gastrointestinal hemorrhage
detection of a Meckel’s diverticulum
9accumulation in ectopic gastric mucosa)
56. Arteriography
Contrast injection into the superior andinferior mesenteric arteries may pinpoint the
source of acute small- or large-bowel
hemorrhage. Bleeding has to be fairly brisk,
however, at 1-2ml/min.
57. Patient Preparation
For an upper gastrointestinal or smallbowel examination, the patient should havenothing orally after midnight or the next
morning preceding the radiographic study.
Fluid and food in the stomach and small
intestine degrade the examination by
interfering with good mucosal visualization
and causing artifacts that may mimic
disease.
58.
Also, if patients are to have other imagingexaminations that may introduce fluid into the
upper gastrointestinal tract, such as an
abdominal CT study in which oral contrast
material is used, the examinations must be
scheduled on separate days. When multiple
abdominal radiographic studies are ordered,
discussion with the radiologist is appropriate
so that the correct sequence can be planned.
59.
Preparation for the barium enema is muchmore complicated, but must be performed
properly to obtain and accurate evaluation of
the colon; this is also required for
performance of colonoscopy and CT
colonography.
60. The standard preparation includes
(1) a 24-hour clear liquid diet(2) oral hydration;
(3) a saline cathartic (e.g., magnesium citrate) in the
afternoon;
(4) an irritant cathartic (e.g., castor oil) in the early
evening; and
(5) a tap-water cleansing enema the morning of the
radiographic examination (30 to 60 minutes before
the barium enema).
61. ACHALASIA
Achalasia is a motor disorder of theoesophagus generally occurring in the 35-50
year age group. It is caused by degeneration
of neurons of Auerbach's plexus, which is
situated between the longitudinal and circular
muscle coats. Primary and secondary
peristalsis initially fails, tertiary contractions
develop, and there is a failure of relaxation of
the lower oesophageal sphincter.
62.
Unlike strictures of the oesophagus, which initiallycause dysphagia for solids but allow liquids to pass,
achalasia causes dysphagia for both solids and
liquids.
The earliest changes are characterized by defective
distal peristalsis associated with a slight narrowing at
the gastro-oesophageal junction.
As the disease progresses, the characteristic ‘bird
beak’ or ‘rat’s tail’ appearance of the gastrooesophageal junction is observed.
63.
Often, by this stage, the body of theoesophagus has become slightly dilated and
demonstrates aperistalsis.
With severe achalasia there is substantial
dilatation of the oesophagus that contains a
huge residue of food and fluid debris.
Absent gastric fundal air bubble
64.
65. Carcinoma of oesophagus
Irregular narrowing of the lumen with slightproximal dilatation
66. Difference between carcinoma of oesophagus and achalasia cardia
Radiologicalsigns
Carcinoma
oesophagus
Achalasia
cardia
narrow lumen
eccentric
central
outline
irregular
smooth
affected area
rigid
moves freely with
heart movement
67. Difference between benign stricture of oesophagus and malignant stricture of oesophagus
Benign strictureMalignant stricture
Long segment
Short segment
Concentric and smooth
tapering
No shouldering
Eccentric, irregular
narrowing
Shouldering is seen
No mucosal irregularity
Usually associated with
mucosal irregularity
68.
69. Lower oesophageal obstruction
70. Benign stricture
71.
72. Esophageal Diverticula
Zenker’s diverticulumIn the lower cervical region, sometimes a
pharyngeal diverticulum (Zenker’s
diverticulum) projects posteriorly. Food can
be caught in this, causing dysphagia. It due
to impaired crico-pharengeal relaxation
between the oblique and horizontal fibres of
inferior constrictor muscle. The mucosa
prolapses out through the muscles.
73. Radiological sings:
widened retro-tracheal soft tissue spaceoften with an air-fluid level
pulsion type of diverticulum
74. Complications:
* Aspiration* Pneumonia
75.
Tractional diverticulae:secondary to fibrosis in lung or mediastinum
the wall of the diverticula contains all the layers
Pulsion diverticula:
the wall composed of only mucosa and submucosa
herniating the muscularis
usually it is acquired condition
76. Zenker’s diverticulum
77.
78.
79. Gastric ulcer
Gastric ulcers penetrate the stomach wall throughthe mucosa into the submucosa and frequently the
muscular is propria. Gastric ulcer is a common
gastrointestinal disorder and is amenable to reliable
radiographic detection. Almost all gastric ulcers (95
per cent) are benign, with about 70 per cent now
shown to be caused by H. pylori infection.
Gastric ulcers are most prevalent in the distal
stomach and along the lesser curvature. They are
more common on the posterior wall of the stomach
than the anterior wall and least common in the
fundus.
80. Radiographic signs
in profile (a benign ulcer in profile protrudesoutside the expected line of the stomach
wall, whereas a malignant ulcer at the apex
of a protruding tumour mass will lie within the
outline of the stomach
en face (straight on; an ulcer on the
dependent wall of the stomach fills with
barium, whereas an ulcer on the nondependent wall is seen as a ring)
81.
The en face radiographic signs of gastriculcers are best seen on double-contrast
barium studies and to a lesser extent on
compression views in the single-contrast
examination.
collection of barium on the dependent wall
most benign ulcers are round or oval
some may have tear-drop or linear contour
82.
it may be demonstrated as a ‘ring’ shadow,with barium coating the edge of the ulcer
crater
edema is often seen surrounding the ulcer
crater causing a circular filling defect
radiating folds seen in healing ulcers should
be smooth and symmetric and continue to
the edge of the crater
83. The in profile radiographic signs of gastric ulcers
‘ulcer niche’, projects beyond the lumen of thestomach
sometimes a pencil-thin line of lucency is present
crossing the base of the ulcer
more often there is a thicker (2–4 mm) smooth rim of
lucency at the base of the ulcer termed the ulcer
collar
oedema associated with an ulcer it forms an ulcer
mound
84. Duodenal ulcer
Radiological signs:deformity of the duodenal cap may be caused by an
ulcer crater, edema, fibrosis, muscular spasm or a
combination of these lesions
barium in the crater may appear a niche projection
from the general contour of the cap, if it is seen
tangentially
if it is seen en face after compression, it appears as
as isolated spot, the surrounding edema causing a
translucent area
if the ulcer is chronic, the folds may converge
towards it giving a stellate appearance
85. Differences between peptic ulcer and malignant ulcer
peptic ulcermalignant ulcer
folds
converge
towards ulcer
interrupted
x-ray after 4
weeks
great shrinkage
moderate or no
shrinkage
86.
87.
88.
89.
90. .A = benign;B = malignant; C = non-projecting benign;
91. Duodenal ulcer
92.
93.
94.
95. Gastritis
Gastritis is a descriptive term withsometimes conflicting pathological,
endoscopic and radiographic definitions.
96. The most common findings are
thick (>5 mm) folds with or without nodularityerosions, while less commonly seen, are a
frequent sign of H. pylori gastritis
antral narrowing
inflammatory polyps
The radiological findings are similar to
endoscopic findings.
97. Acute erosive gastritis.
98. antral gastritis
99. Menetrier's disease.
100. Hypertrophic pyloric stenosis
Hypertrophic pyloric stenosis is a relativelyfrequent congenital disorder diagnosed in
infancy. Presentation in adults occasionally
occurs. The morphological features are due
to hypertrophy and hyperplasia of the circular
muscle with some contribution by the
longitudinal muscle. The hypertrophied
muscle lengthens and narrows the pyloric
channel.
101. Radiographically:
shoulder sign – an indentation into the barium filledpyloric antrum is caused by thickened pyloric muscle
beak sign – this occurs where the barium column
extending into the narrowed pyloric canal is cut off
similar to a beak
double track – parallel mucosal folds extending
through the elongated pyloric canal
string sign – a thin streak of barium may be seen
extending between the pyloric antrum and the
duodenal cap
102. USG is investigation of choice and shows:
pyloric canal length>16 mmtransverse pyloric diameter >11 mm
pyloric canal does not open, therefore,
decreased gastric emptying
increased gastric peristalsis proxomaly
103.
104.
105. Polyps
Hyperplastic polyps are by far the mostcommon benign neoplasm of the stomach.
These polyps are not considered to have
malignant potential, but do occur more
commonly in patients who have other risk
factors for developing gastric malignancy,
such as atrophic gastritis, and in patients
with gastric resections and bile reflux
gastritis.
106. Radiographically:
round filling defectsmooth sessile lesions
they are usually multiple and of uniform size
(5–10 mm)
they are most common in the fundus and
body of the
107.
108.
109.
110.
111. Gastric carcinoma
ulcerativefungating
infiltrative
diffuse infiltrative
mucinous type
112.
The most common presentations on the doublecontrast upper gastrointestinal examination are as:a filling defect
a shallow ulceration with converging folds
the folds are often thickened, irregular or nodular in
shape and may have a club-like appearance
the folds may appear to converge; this appearance
is due to a fibrous reaction induced by many of these
tumours
when the antrum is primarily involved by tumour, it
may be severely narrowed or obstructed
rigidity of the gastric wall and decreased peristalsis
indicate submucosa spread of the tumor
113.
A primary neoplastic ulcer is oftenindistinguishable from a simple ulcer.
Filling defect in the barium shadow by a
large fungating mass.
Hour glass stomach due to annular
constricting type of growth.
Narrow irregular gastric outline due to
submucous, diffuse, infiltrating neoplasm.
















































































































 medicine
medicine